Published online Dec 16, 2015. doi: 10.12998/wjcc.v3.i12.1017
Peer-review started: May 4, 2015
First decision: July 10, 2015
Revised: September 8, 2015
Accepted: October 16, 2015
Article in press: October 19, 2015
Published online: December 16, 2015
Processing time: 218 Days and 16.6 Hours
Neuropathic arthropathy of the shoulder is a rare disorder characterized by joint degeneration, and is associated with loss of sensory innervation. Syringomyelia is a disease in which fluid-containing cavities (syrinxes) form within the spinal cord. Here, we report a case of neuropathic arthropathy of the shoulder secondary to syringomyelia in a 40-year-old woman. X-rays of the left shoulder revealed damage to bone and joint architecture. Blood tests indicated vitamin D deficiency and secondary hyperparathyroidism. Magnetic resonance imaging of the cervical spine showed a large syrinx from the second cervical spine to the second dorsal spine. Although neuropathic arthropathy is uncommon, it should be considered in cases of unexplained pain, discomfort, or limited range of motion of the affected joint. Symptoms related to the affected joint may precede or overshadow neurological deficits. Appropriate radiological examinations and diagnoses are imperative to prevent misdiagnosis or undetected bone and joint disorders.
Core tip: Neuropathic arthropathy, also called Charcot shoulder, is a chronic, degenerative condition associated with decreased sensory innervation. Syringomyelia patients typically suffer with shoulder and elbow involvement. Since joint symptoms often appear before other signs, neurological deficits are often overshadowed, and the condition is misdiagnosed. In cases of unexplained joint pain, discomfort, and limited range of motion, syringomyelia should always be considered even in the absence of detectable neurological features. To prevent misdiagnoses, clinicians should be aware of the clinical and radiological signs of this rare condition. Timely diagnoses are important to avoid unwanted operative procedures that could lead to unsatisfactory outcomes.
- Citation: Chakraborty PP, Datta S, Ray S, Bhattacharjee R, Chowdhury S. Unilateral neuropathic arthropathy of the shoulder secondary to syringomyelia: Diagnostic challenges. World J Clin Cases 2015; 3(12): 1017-1020
- URL: https://www.wjgnet.com/2307-8960/full/v3/i12/1017.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i12.1017
Neuropathic arthropathy of the shoulder, also called Charcot shoulder, is a chronic, degenerative condition associated with decreased sensory innervation. Patients with diabetes mellitus, syphilis, or syringomyelia are at most risk for this disease[1]. Diabetic patients are most commonly afflicted with foot and ankle disease, while the knee is typically involved in syphilis patients. Syringomyelia patients usually present with pain in the upper limbs, shoulder joint, and elbow[2]. Approximately 6% of patients with neuropathic arthropathy have shoulder joint involvement[3]. Here, we report a case of neuropathic arthropathy of the shoulder secondary to syringomyelia. The case was of particular interest, as it was initially misdiagnosed as a pseudofracture secondary to osteomalacia. Accurate, timely diagnoses are important to avoid operative procedures.
A 40-year-old woman visited her family physician with a three-month history of gradually increasing discomfort and restricted movement of the left shoulder. It was not preceded by any trauma. She was found to be non-diabetic, but her serum 25-hydroxy vitamin D level was low (12 ng/mL). She was initially thought to have frozen shoulder and was advised to undergo physiotherapy. However, upon examination of X-ray results and the presence low vitamin D levels, she was then diagnosed with osteomalacia with pseudofracture and was advised to take oral cholecalciferol and undergo physiotherapy. She had no other symptoms related to osteomalacia, such as bone pain, muscle weakness, or difficulty walking.
Due to lack of improvement, the patient was subsequently referred to our facility. Physical examination showed asymmetry of the shoulder joints and drooping of the left shoulder. The shoulder joint was not palpable and the patient had painless restriction of joint movement in all axes. She denied any history of long-term steroid use or other drug use. She had normal menstrual cycles without any history of low trauma fracture elsewhere. She had normal sensations and preserved powers in all the four limbs with normal deep tendon reflexes and downgoing plantars. No muscle wasting, or peripheral nerves thickening were evident. Despite getting a normal neurological examination, we suspected a neuropathic joint.
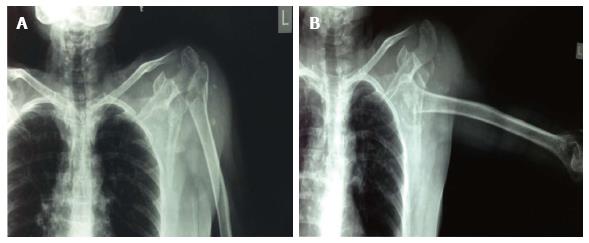
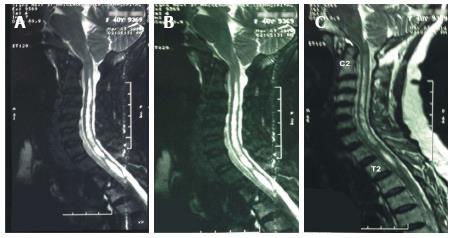
A thorough look at the radiographs of the left shoulder revealed resorption of the left humeral head and parts of the glenoid cavity, multiple loose bodies, and dislocation of the left shoulder joint (Figure 1). We also obtained blood counts, measured her erythrocyte sedimentation rate, tested for venereal diseases, and measured serum vitamin B12 and serum intact parathormone (iPTH) levels. A skeletal survey and magnetic resonance imaging (MRI) of cervical and thoracic spine were also performed. Besides an elevated iPTH level (120 pg/mL), the rest of the blood and serum results were normal. Skeletal radiographs did not indicate the presence of looser zones, which are common in patients with osteomalacia. However, the MRI of the cervicodorsal spine revealed a hyperintense intramedullary signal change extending from C2 to T2, determined to be a syrinx. The craniovertebral junction appeared normal (Figure 2). Based on the patient’s symptoms, the clinical examination, X-ray and MRI findings, we re-diagnosed the patient with neuropathic arthropathy of the shoulder. She was transferred to the physical therapy and rehabilitation department for conservative treatment.
The relationship between syringomyelia and neuropathic arthropathy is well described. Syringomyelia is a chronic disease anatomically characterized by the development of a tubular cavitation within the spinal cord. It can be congenital or can be caused by trauma, tumors, degenerative diseases, or infection[4]. The usual manifestations of syringomyelia include dissociated anesthesia in a “cape” distribution, areflexia, weakness, and of upper limb along with neuropathic joints. Less commonly, syringomyelia presents with atypical symptoms (e.g., limb hypertrophy, joint pain, swelling) with or without detectable neurological symptoms[5]. Neuropathic arthropathy is a form of chronic destructive arthropathy that occurs secondary to sensory loss of the involved joint. Twenty-five percent of patients with syringomyelia develop neuropathic arthropathies, 80% of which involve an upper limb[6].
Neuropathic arthropathy of the shoulder is a rare disorder, with very few cases reported in the English literature. A review by Hatzis et al[3] found 31 documented cases of neuropathic arthropathy of the shoulder. Although neuropathic arthropathy of the shoulder had varied clinical presentations, shoulder pain and swelling were the most common symptoms. Stiffness and decreased range of movement were the next most frequent symptoms. These more common symptoms often precede and overshadow neurological deficits. The patient first visited her family physician with discomfort and restricted movement of shoulder joint, which was suggestive of frozen shoulder.
Neuropathic arthropathy of the shoulder generally progresses slowly, but rapid progression may happen over months or even weeks. The symptoms of neuropathic shoulder may mask the symptoms of syringomyelia, which is often characterized by shoulder instability. Complete dislocation of the neuropathic shoulder may even occur. Since neurological symptoms occur much later than pain or discomfort, patients typically first visit a primary care physician or an orthopedic surgeon[3]. If neuropathic arthropathy of the shoulder is suspected, X-rays and an MRI of the cervical cord should be taken to look for syringomyelia since it is the most common underlying disease.
Low dietary intake of calcium often leads to vitamin D deficiency in the Indian population. In reproductive vs post-menopausal age groups, 25-hydroxy vitamin D tests show a deficiency (< 20 ng/mL) in 76% vs 16.5% of those measured, or an insufficiency (20-30 ng/mL) in 7.5% vs 70%[7]. Vitamin D deficiency can lead to low bone mass, muscle weakness, and an increased risk of osteoporotic fractures. In our patient, the vitamin D deficiency was detected by her primary care physician. She was referred to us with a suspicion that her shoulder pathology was secondary to osteomalacia. Secondary hyperparathyroidism was detected upon further investigation at our clinic based on elevated iPTH levels. Although the presence of low 25-hydroxy vitamin D levels and high iPTH levels made osteomalacia highly likely, a low serum 25-hydroxy vitamin D is a poor indicator of osteomalacia. We therefore performed skeletal radiographs to look for pseudofractures or looser zones, which are common in patients with osteomalacia. These are lucent lines seen perpendicular to cortex which spans the cortex incompletely looser zones occur most commonly in ribs, outer borders of scapulae, and the pubic rami. However, the shoulder radiograph in this case strongly suggested a neuropathic joint. Neuropathic arthropathy of the shoulder leads to rapid, extensive degradation of the proximal humerus and glenoid cavity, and is sometimes destroyed in less than 6 wk[8]. Radiographs of neuropathic arthropathy often show osseous fragmentation and debris. Fractures are lesser-known manifestation of the disorder. The treatment strategy for neuropathic arthropathy is conservative. The prevention of trauma to the joint with proper splinting is the key to treatment. Aspiration of large effusions and splinting prevents further ligamentous laxity[9,10]. Our patient showed satisfactory improvement upon conservative treatment.
The case presented with shoulder-related signs and symptoms. Since a vitamin D deficiency was detected, the patient’s physician suspected osteomalacia rather than a neuropathic disorder. Neuropathic arthropathy, although rare, should be considered as the possible source of unexplained joint pain, discomfort, and limited range of motion. Neuropathic arthropathy is often misdiagnosed, especially that occurring at non-weight-bearing joints. It is commonly misattributed, even with radiographs, to other etiologies such as osteoarthritis, infection, or tumors. Even in the absence of prominent neurological features, syringomyelia should always be considered as the underlying cause of neuropathic arthropathy of the shoulder.
A 40-year-old woman presented with stiffness and restricted movement of the left shoulder.
Neuropathic arthropathy of the shoulder secondary to syringomyelia.
Neuropathic joint, osteonecrosis, and pathological fracture from neoplasms.
Blood and serum levels were normal, with the exception of elevated intact parathormone levels (120 pg/mL) and low serum 25-hydroxy vitamin D levels (12 ng/mL).
X-rays of left shoulder revealed resorption of the left humeral head and parts of the glenoid cavity, multiple loose bodies, and dislocation of the left shoulder joint. Magnetic resonance imaging of the cervicodorsal spine showed a hyperintense intramedullary signal change extending from C2 to T2, indicating the presence of a syrinx.
Patient received physical therapy.
Neuropathic arthropathy involving the shoulder joint is an uncommon disorder, with less than 70 cases reported in the English literature.
Neuropathic arthropathy represents a spectrum of bone and joint destructive processes associated with neurosensory deficit. Loss of proprioception has been implicated as a causative factor in pathogenesis of the disease.
Even in the absence of prominent neurological features, syringomyelia should always be considered as a differential diagnosis of upper limb neuropathic joints.
This is a good article.
P- Reviewer: Disthabanchong S, Yu ZW S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Allman RM, Brower AC, Kotlyarov EB. Neuropathic bone and joint disease. Radiol Clin North Am. 1988;26:1373-1381. [PubMed] |
| 2. | Shapiro G, Bostrom M. Heterotopic ossification and Charcot neuroarthropathy. Chapman’s Orthopaedic Surgery. Philadelphia: Lippincott Williams and Wilkins 2001; 3245-3262. |
| 3. | Hatzis N, Kaar TK, Wirth MA, Toro F, Rockwood CA. Neuropathic arthropathy of the shoulder. J Bone Joint Surg Am. 1998;80:1314-1319. [PubMed] |
| 4. | Klekamp J. The pathophysiology of syringomyelia - historical overview and current concept. Acta Neurochir (Wien). 2002;144:649-664. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 138] [Cited by in RCA: 121] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 5. | Chakraborty PP, Bandyopadhyay D, Mandal SK, Banerjee R, Chowdhury SR, Majumdar S, Bhattacharji R. Unilateral limb hypertrophy and shoulder weakness in a 37-year-old woman. Med J Aust. 2006;184:130-131. [PubMed] |
| 6. | Yanik B, Tuncer S, Seçkin B. Neuropathic arthropathy caused by Arnold-Chiari malformation with syringomyelia. Rheumatol Int. 2004;24:238-241. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 22] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Harinarayan CV, Sachan A, Reddy PA, Satish KM, Prasad UV, Srivani P. Vitamin D status and bone mineral density in women of reproductive and postmenopausal age groups: a cross-sectional study from south India. J Assoc Physicians India. 2011;59:698-704. [PubMed] |
| 8. | Brower AC, Allman RM. Pathogenesis of the neurotrophic joint: neurotraumatic vs. neurovascular. Radiology. 1981;139:349-354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 157] [Cited by in RCA: 115] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 9. | Jones J, Wolf S. Neuropathic shoulder arthropathy (Charcot joint) associated with syringomyelia. Neurology. 1998;50:825-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 42] [Cited by in RCA: 32] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Johnson JT. Neuropathic fractures and joint injuries. Pathogenesis and rationale of prevention and treatment. J Bone Joint Surg Am. 1967;49:1-30. [PubMed] |