Published online Nov 16, 2015. doi: 10.12998/wjcc.v3.i11.970
Peer-review started: May 20, 2015
First decision: July 29, 2015
Revised: August 16, 2015
Accepted: September 16, 2015
Article in press: September 18, 2015
Published online: November 16, 2015
Processing time: 175 Days and 16.2 Hours
Meckel diverticulum is an embryonic remnant of the Gastrointestinal duct which causes symptoms < 5% in the 2% population. Painless bleeding and abdominal pain are the most often reported symptoms. Dieulafoy lesion/dieulafoy-like lesion often cause upper gastrointestinal (GI) tract bleeding, but massive lower gastrointestinal bleeding is rare. We reported a 19-year-old male presented massive lower GI tract bleeding caused by Meckel diverticulum synchronous dieulafoy-like lesion.
Core tip: Dieulafoy-like lesion often causes upper gastrointestinal (GI) tract bleeding, and meckel diverticulum is another common cause of GI tract bleeding. The two of them happened at the same person is rare. We observed a 19-year-old man complained of upper stomachache was admitted to hospital. He underwent left hemi-colectomy on day 5 after admitted. Pathology confirmed the diagnosis of dieulafoy-like lension of descending colon. The bleeding ceased for 2 d. But another attack came on day 3 after surgery. He underwent a second laparotomy which united endoscopy, a 2 cm × 1.5 cm meckel diverticulum in terminal ileum was detected. Resection was performed. Pathology revealed meckel diverticulum. He was fully recovered with no sign of bleeding in the next year’s following up.
- Citation: Li SH, Wu GY, Lin XD, Wen ZQ, Huang MT, Yu SP, Zhang H. Lower gastrointestinal tract bleeding caused by dieulafoy-like lesion synchronous meckel diverticulum: A rare case report. World J Clin Cases 2015; 3(11): 970-972
- URL: https://www.wjgnet.com/2307-8960/full/v3/i11/970.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i11.970
A 19-year-old man was admitted to hospital due to upper stomachache for 6 d, hematochezia for 3 d and syncope twice. He had recurrent massive hematochezia and conservative therapy was inefficacy. He had left hemi-colectomy on day 5 after admitted. Pathology confirmed the diagnosis of dieulafoy-like lesion of descending colon. The bleeding ceased for 2 d. He had another attack of hematochezia on day 3 after surgery (day 7 after admitted). He underwent a second laparotomy which united colonoscopy, a 2 cm × 1.5 cm meckel diverticulum in terminal ileum was detected. Resection was performed. Pathology revealed meckel diverticulum, atopia gastric mucosa polyp accompany with chronic ulcer. He recovered well and was discharged 20 d later. The next year’s following up shows no sign of bleeding.
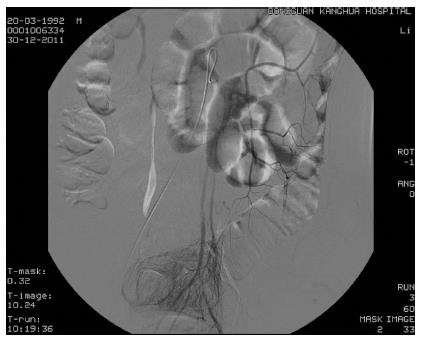
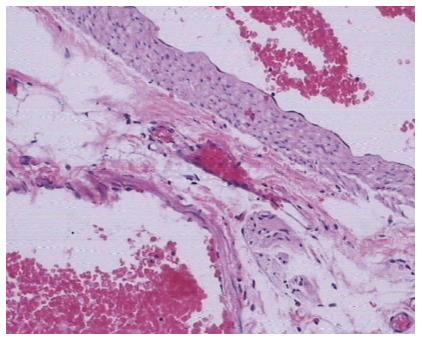
A 19-year-old man was admitted to hospital due to upper stomachache for 6 d, hematochezia for 3 d and syncope twice. He looked pale and weak when admitted. Blood count reveals RBC 2.44 × 1012/L, Hb 71 g/L, HCT 0.20. There is no sign of abnormal of his colon except retention of fresh blood in the following day’s colonoscopy. Tc-99m pertechnetate scan in the third day revealed no positive sign neither. The patient had a third time of hematochezia for about 300 mL. Bleeding from the left hemicolon was highly suspected during the second colonoscopy, but exact bleeding point was not observed. He was treated with hemostasia to stop the bleeding and fluid infusion therapy. A fourth time hematochezia occured in day 5. Digital subtraction angiography supported bleeding from left hemi-colon (Figure 1). He was sent to OR for left hemi-colectomy. Pathology confirmed the diagnosis of dieulafoy-like lension of descending colon (Figure 2). The bleeding ceased for 2 d. On day 3 post colectomy (day 7 after admitted), he had the fifth hematochezia, discharged about 1000 mL of blood. Blood transfusion and blood coagulant were used to stop bleeding. Those treatments did not stop the bleeding. He underwent a second laparotomy united colonoscopy. During the surgery laparotomy united colonoscopy, a 2 cm × 1.5 cm meckel diverticulum in terminal ileum was detected (Figure 3). A wide base, smooth, about 0.6 cm × 0.6 cm hemispherical polyp beside it was observed, resection was performed meanwhile. Pathology revealed meckel diverticulum, atopic gastric mucosa polyp accompany with chronic ulcer. The patient recovered in 20 d with neither bleeding nor other complications and was discharged. There was no more hematochezia in the next year’s follow up.
Dieulafoy lesion/dieulafoy-like lesion is a cause of GI tract bleeding which cannot be ignored, most commonly results the proximal stomach bleeding, but very rare entity that can cause massive lower gastrointestinal track bleeding[1]. Meckel diverticulum is an embryonic remnant of the gastrointestinal duct which is presented in approximately 2% of the population and is estimated to cause symptoms < 5% of the time. It generally results in painless bleeding or abdominal pain[2]. The technetium 99m pertechnetate scan is the best of choice for detecting Meckel diverticulum, with a reported sensitivity of 85% to 90% in the pediatric population[3]. In adults, however, the sensitivity falls on to only 62%[4]. It is an ideal noninvasive and sensitive way to detective meckel diverticulum. We performed surgery though this patient’s technetium 99m pertechnetate scan is negative and a meckel diverticulum was found. This case presented of massive lower gastrointestinal bleeding caused by descend colon dieulafoy-like lesion and small bowl meckel diverticulum at same time is a rare condition.
A 19-year-old man complained of upper stomachache was admitted to hospital.
Massive lower gastrointestinal bleeding caused by descend colon dieulafoy-like lesion and small bowl meckel diverticulum at same time.
Tumor of the colon, ischemic colitis, Crohn’s disease, Ulcerative colonitis.
Blood count reveals RBC 2.44 × 1012/L, Hb 71 g/L, HCT 0.20.
Tc-99m pertechnetate scan in the third day revealed no positive sign. Digital subtraction angiography supported bleeding from left hemi-colon.
Pathology confirmed the diagnosis of dieulafoy-like lension of descending colon at the first surgery. Pathology reveals meckel diverticulum, atopic gastric mucosa polyp accompany with chronic ulcer after the second surgery.
Left hemi-colectomy and resection of the bowl with meckel diverticulum.
Dieulafoy lesion of the colon is reported to be bleeding cause of lower GI tract bleeding, and so does meckel diverticulum.
Massive lower gastrointestinal bleeding caused by descend colon dieulafoy-like lesion and small bowl meckel diverticulum at same time is a rare condition. Both of them may be missed at the first endoscopy examination. Repeated endoscopy examination may be needed when bleeding occurs over and over again.
This case is interesting.
P- Reviewer: Kim ST, Sergi C S- Editor: Tian YL L- Editor: A E- Editor: Wang CH
| 1. | Abdulian JD, Santoro MJ, Chen YK, Collen MJ. Dieulafoy-like lesion of the rectum presenting with exsanguinating hemorrhage: successful endoscopic sclerotherapy. Am J Gastroenterol. 1993;88:1939-1941. [PubMed] |
| 2. | Kline RM. Ruptured Meckel diverticulum mimicking mucositis in a patient receiving induction therapy for high-risk acute lymphoblastic leukemia. J Pediatr Hematol Oncol. 2007;29:423-424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 3. | Sfakianakis GN, Conway JJ. Detection of ectopic gastric mucosa in Meckel’s diverticulum and in other aberrations by scintigraphy: ii. indications and methods--a 10-year experience. J Nucl Med. 1981;22:732-738. [PubMed] |
| 4. | Schwartz MJ, Lewis JH. Meckel’s diverticulum: pitfalls in scintigraphic detection in the adult. Am J Gastroenterol. 1984;79:611-618. [PubMed] |