Published online Nov 16, 2015. doi: 10.12998/wjcc.v3.i11.965
Peer-review started: May 9, 2015
First decision: June 19, 2015
Revised: July 6, 2015
Accepted: August 30, 2015
Article in press: September 9, 2015
Published online: November 16, 2015
Processing time: 190 Days and 21.4 Hours
Fitz-Hugh-Curtis syndrome is a type of perihepatitis that causes liver capsular infection without infecting the hepatic parenchyma or pelvis. Fitz-Hugh-Curtis syndrome is known to occur commonly in women of childbearing age who do not use oral contraceptives and have sexual partners older than 25 years of age. However, the syndrome has been reported to occur rarely in males. The clinical symptoms are right upper quadrant pain and tenderness, and pleuritic right sided chest pain. The clinical presentation is similar in male and female. We experienced a case of Fitz-Hugh-Curtis syndrome in a 60-year-old man with the chief complaint of right upper quadrant abdominal pain. Despite a previous history of gonorrhea, we have also described our experiences of improved symptoms and recovery with allopathic medicines and have thereby reported the present case with a literature review.
Core tip: Fitz-Hugh-Curtis syndrome is known to occur commonly in sexually active women and very rarely in males. We experienced a case of Fitz-Hugh-Curtis syndrome in a 60-year-old man with the chief complaint of right upper quadrant abdominal pain on inspiration. Despite of negative laboratory result, we diagnosed as Fitz-Hugh-Curtis syndrome by symptom and liver computed tomography scan. We have also described our experiences of improved symptoms and recovery with allopathic medicines.
- Citation: Yi H, Shim CS, Kim GW, Kim JS, Choi IZ. Case of Fitz-Hugh-Curtis syndrome in male without presentation of sexually transmitted disease. World J Clin Cases 2015; 3(11): 965-969
- URL: https://www.wjgnet.com/2307-8960/full/v3/i11/965.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i11.965
Fitz-Hugh-Curtis syndrome is a type of perihepatitis that causes liver capsular infection without infecting the hepatic parenchyma or pelvis. In 1920, Carlos Stajano first described the surgical confirmation of an adhesion that connected the anterior peritoneum and hepatic parenchyma in a gonorrheal patient who had complained of right upper quadrant abdominal pain. In 1930, Curtis[1] reported an adhesion of the peripheral hepatic parenchyma in a patient with salpingitis. In 1934, Fitz-Hugh[2] identified Neisseria gonorrhoeae (N. gonorrhoeae) on a peripheral liver adhesion in a patient complaining of right upper quadrant abdominal pain and reported that these findings were associated with the violin string-shaped adhesions around the liver observed in female patients with pelvic infection and salpingitis, which was at that time suggested as a new syndrome in terms of the pathophysiology of venereal diseases. Initially, only N. gonorrhoeae was considered a causative bacterium; however, in recent years, additional causative bacteria such as Chlamydia trachomatosis (C. trachomatosis) have been reported, and this condition was also found to be caused by other bacterial sexually transmitted diseases in addition to gonorrhea[3-5].
Traditionally, Fitz-Hugh-Curtis syndrome is known to occur commonly in women of childbearing age who do not use oral contraceptives and have sexual partners older than 25 years of age; because of unclear statistical results, it is uncertain whether this condition is accompanied by pelvic inflammation. However, since its detection in men after the 1970s[6], more extensive studies of this disease have been performed.
Based on the diagnostic criteria of a disease history and clinical patterns, cases in which a violin string-shaped abdominal adhesion is confirmed through laparoscopy or laparotomy to exclude other diagnoses and in which causative bacteria are identified in the liver capsule exudate are generally diagnosed as Fitz-Hugh-Curtis syndrome. In 2003, Nishie et al[7] and colleagues observed more definite hepatic capsule enhancement in the arterial phase relative to other phases during a computed tomography (CT) scan. Using abdominal dynamic CT scans, Joo et al[8] detected Fitz-Hugh-Curtis syndrome with a sensitivity of 88% and specificity of 95%, and Woo et al[9] diagnosed Fitz-Hugh-Curtis syndrome with 95.5%. In recent years and in consideration of surgical complications, non-invasive diagnoses not requiring surgery have increased for cases with mild symptoms by integrating the outcomes of clinical patterns, culture tests, and CT scan results.
In South Korea, Fitz-Hugh-Curtis syndrome was previously reported in women; however, in 2010, Mycoplasma genitalium was first identified via blood testing, an abdominal dynamic CT scan, and urine culture testing in a 35-year-old male patient complaining of right upper quadrant abdominal pain[10]. In addition to a literature review, the authors herein report a case of non-invasively diagnosed Fitz-Hugh-Curtis syndrome in a sexually inactive, hepatitis B virus (HBV)-positive elderly patient who presented with right upper quadrant abdominal pain; this diagnosis was achieved via blood testing and an abdominal dynamic CT scan, and excluded other diseases despite the inability to identify the causative bacteria.
A 60-year-old male patient was admitted to the emergency room with right upper quadrant abdominal pain that had gradually increased in severity beginning three days earlier. This pain was not affected by meals, and became sharp and severe upon inhalation. The patient had a disease history of gonorrhea while in his 20s, although this had completely recovered, and had no family medical history. He was divorced, a non-smoker, drank 1 bottle of soju 3-4 times a week, and had no external injuries. At the time of admission, his vital signs were as follows: Blood pressure, 140/70 mmHg; pulse rate, 80 times/min; respiration, 20 times/min; and body temperature, 36.5 °C. He presented with acute symptoms, no specific sphygmoscopic findings, a soft abdomen, normal bowel sounds, oppressive pain in the right upper abdominal quadrant, no rebound tenderness or abdominal distension, and Murphy’s sign negativity. He did not present with shifting dullness or fluid waves indicative of ascites, enlarged organs or masses, or bilateral costovertebral pain.
Peripheral blood tests revealed the following (Table 1). The following serum biochemical test results (Table 1) were observed: Increased C-reactive protein, aspartate aminotransferase, and alanine aminotransferase. Urine tests revealed no specific findings, and the results of simple chest and abdominal radiography were normal.
| Peripheral blood test | |
| Leukocyte | 3610/mm3 |
| Neutrophils | 50.90% |
| Lymphocytes | 35.50% |
| Hemoglobin | 146 g/L |
| Platelet | 164000/mm3 |
| Erythrocyte sedimentation rate | 25 mm/h |
| Serum biochemical test | |
| C-reactive protein | 15.6 mg/L |
| Total protein | 67 mg/L |
| Albumin | 37 mg/L |
| Total bilirubin | 5.8 mg/L |
| Aspartate aminotransferase | 52 IU/L |
| Alanine aminotransferase | 47 IU/L |
| Alkaline phosphatase | 93 IU/L |
| Blood urea nitrogen | 148 mg/L |
| Creatinine | 6.1 mg/L |
| Na | 134 mmol/L |
| K | 4.01 mmol/L |
| Cl | 98.3 mmol/L |
| Creatine kinase-myocardial band | 2.27 ng/mL |
| Troponin-T | 0.003 ng/mL |
| Amylase | 61 U/L |
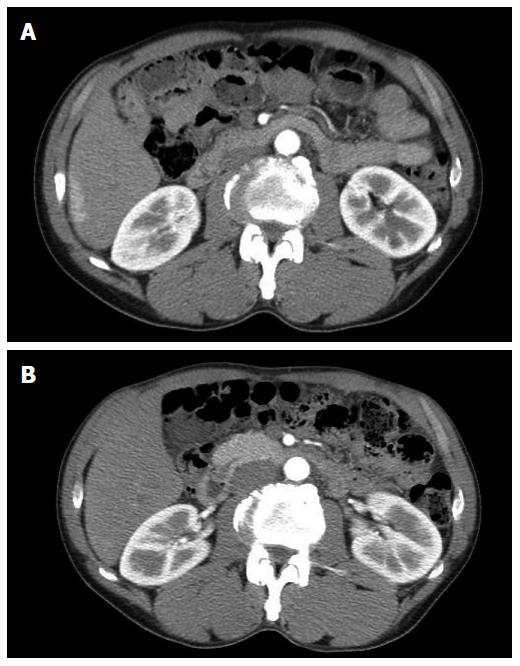
An abdominal pelvic CT scan was performed, and linear capsular enhancement of the inferior segment of the liver was observed in the arterial phase (Figure 1A). No specific findings were observed in other abdominal and pelvic organs, including the hepatic parenchyma, gallbladder, biliary tract, and pancreas. Hepatitis virus tests were planned to evaluate the increased hepatosomatic index, and a fluid treatment involving daily intravenous levofloxacin administration (500 mg) as well as experimental antibiotics were planned to treat suspected Fitz-Hugh-Curtis syndrome. Based on the findings observed in known cases of this disease, examinations of previous urinary tract infections or venereal diseases, blood tests, and urine culture tests were performed. In a subsequent examination, the patient reported having 1 sexual relationship 20 d earlier; all results for the following tests were negative: Human immunodeficiency virus (HIV) Ag/Ab combi test, urine culture test, and PCR for N. gonorrhoeae, C. trachomatis, Ureaplasma urealyticum, M. genitalium, M. hominis, Trichomonis vaginalis, Treponema palladium, Candida albicans, Herpes simplex VI and VII, Haemophilus ducreyi, and Condyloma 6, 11, which was performed after prostate massage. The hepatitis virus test indicated the following: Hepatitis A virus IgM, HBV surface antibody (enzyme-linked immunoassay; EIA), HBV extracellular antigen (HBeAg), and hepatitis C virus Ab negativity; HBV surface antigen (EIA) and HBV extracellular antibody (HBeAb) positivity; and an HBV DNA copy number of 1.59 × 107/mL. A tumor marker test measured to exclude cancer and showed no abnormalities (Table 2). Gastroscopy and colonoscopy were performed to exclude cancer, and no specific findings were observed besides chronic superficial gastritis and a gastric ulcer. No findings indicative of liver cancer besides the previously observed capsular enhancement of the inferior segment of liver were observed on a liver abdominal dynamic CT scan.
| Carbohydrate antigen 19-9 | 0.6 U/mL |
| Alpha-fetoprotein | 19.28 ng/mL |
| Carcinoembryonic antigen | 4.69 ng/mL |
| Protein induced by vitamin K absence or antagonist II | 17 nAU/mL |
On the second day of hospitalization, the right upper quadrant abdominal symptoms improved and on the third day of hospitalization, the patient’s pain upon inhalation had decreased. The patient requested outpatient clinic care and he was discharged from the hospital. Two weeks after the initial medical treatment, the right upper quadrant abdominal pain disappeared during outpatient clinic care, and pain during inhalation decreased to 1-2 times per day. After four weeks of antibiotic treatment, the right upper quadrant abdominal pain improved, and the liver capsule enhancement completely disappeared on a liver abdominal dynamic CT scan performed three months after treatment (Figure 1B).
Fitz-Hugh-Curtis syndrome refers to perihepatitis accompanied by pelvic inflammation in 5%-15% of cases; young women of childbearing age are mainly affected by this disease. The symptoms can be divided into acute and chronic phases. Patients in the acute phase have characteristic pathologic findings of exudative hepatic capsule inflammation with inflammatory reactions and bleeding of the inferior liver and vessels in the abdominal wall adjacent to the liver[11]. Accordingly, in the acute phase, the right upper quadrant abdominal pain is sharp and pleuritic and occasionally radiates to the right shoulder or inside of the arm. In the chronic phase, exudative inflammation causes a violin string-like adhesion between the hepatic capsule and inferior abdominal wall or between the hepatic capsule and diaphragm. Although this adhesion rarely causes clinically significant symptoms, laparoscopic synecotomy can be performed in cases involving persistent right upper quadrant abdominal pain that are refractory to antibiotic therapy[12].
Previously, N. gonorrhoeae was identified as the causative bacterium of Fitz-Hugh-Curtis syndrome, but in recent years C. trachomatis has also been identified as a major causative bacterium. In the present case, the patient had a previous history of gonorrhea and was an HBV carrier; however, there are no previous reports of secondary Fitz-Hugh-Curtis syndrome onset resulting from a previous gonorrheal infection and HBV positivity.
Regarding the infection route, traditionally direct infection has been dominant as determined via culture tests of the uterine tubes and hepatic lesions. However, blood-mediated infection has been reported in other cases[13] via blood culture tests, supporting the use of antibiotic treatment. However, most case reports remain controversial because of a lack of positive culture test results. Infection via lymphatic vessels could explain the cases of perihepatitis in both men and women without gonohemia, although as yet there is no clear evidence to support this. Money et al[14] suggested an immune reaction-based pathophysiology following a comparison of IgG values in the context of chlamydia infection, but currently this hypothesis remains unconfirmed.
Long-term complications of Fitz-Hugh-Curtis syndrome are rare and include pelvic inflammatory complications, chronic pain, small intestinal obstruction due to adhesion, and infertility.
A suspicion of Fitz-Hugh-Curtis syndrome is most important when diagnosing and detecting pleural or right upper quadrant abdominal pain in young, sexually active women in the absence of clear evidence for other diseases such as acute cholecystitis. As mentioned earlier, invasive surgical procedures such as laparoscopic surgery or laparotomy are required to confirm a diagnosis of Fitz-Hugh-Curtis syndrome, but these are not desirable or practically feasible in many cases. Therefore, in actual clinical settings, it is common to diagnose and treat this syndrome under only a presumptive diagnosis and the identification of characteristic strains after excluding other diagnoses. Blood tests mostly reveal a normal or elevated leukocyte count and erythrocyte sedimentation rate and a normal or slightly increased hepatosomatic index, which assist with the diagnosis. CT scans reveal hepatic capsule contrast enhancement, a characteristic finding of perihepatitis, in the arterial phase and are thereby used as a non-invasive method for diagnosing Fitz-Hugh-Curtis syndrome. Although cervical exudate is mainly used for stain identification, vaginal, anal, urethral, and pharyngeal exudates may also be used. Generally, culture tests are most widely used although genetic tests such as PCR or gene amplification provide better sensitivity and specificity. According to recent studies, however, increasing numbers of cases have been observed with C. trachomatosis negative PCR results but positive antigen-antibody reactions, and it is therefore recommended that antibody tests for causative bacteria identification should be performed concurrently[15]. In the present case, both culture tests and PCR were conducted to identify sexually transmitted microbes; however, an antigen-antibody test was not performed and the causative bacteria could not be identified.
Fitz-Hugh-Curtis syndrome can be treated experimentally with antibiotics, according to the principle of using antibiotics suitable for each identified causative bacterium. However, because of the rejection of some patients with venereal diseases, some cases have reportedly been treated with experimental antibiotics in the absence of causative bacteria identification or even attempted identification. Experimental antibiotics use is based on pelvic inflammatory treatment, and antibiotics such as cefotetan, doxycycline, clindamycin, gentamicin, and ofloxacin have been used[16]. Cefotetan and doxycycline are mainly administered intravenously, and levofloxacin and metronidazole can also be used. Intravenous antibiotics are continued for 48 h after the improvement of clinical symptoms, and metronidazole or levofloxacin are used orally for 2 wk. If pain persists even with proper treatment, a peripheral liver adhesion should be confirmed via laparoscopy[17].
Fitz-Hugh-Curtis syndrome is known to be extremely rare in men. In 1970, Kimball and Knee first reported a case of Fitz-Hugh-Curtis syndrome caused by N. gonorrhoeae in a 22-year-old man[6]. In 1982, Davidson and Hawkins[18] reported the development of this syndrome from gonorrheal sepsis concomitant with pustular bacterid in a 35-year-old bisexual man with an identified N. gonorrhoeae infection. In 1985, Winkler et al[19] reported a case of Fitz-Hugh-Curtis syndrome and discussed the possibility that N. gonorrhoeae entered via damaged rectal mucous membranes and directly spread through the abdominal cavity in a 35-year-old homosexual man with a history of acquired immune deficiency syndrome.
In the present case, we have reported a diagnosis of Fitz-Hugh-Curtis syndrome via blood tests and abdominal dynamic CT in a 60-year-old man with the chief complaint of right upper quadrant abdominal pain. Blood culture tests, urine culture tests, and PCR of sexually transmitted disease-causing microbes were performed to identify the causative agent, although N. gonorrhoeae was not proven to be the causative bacterium, despite a previous history of gonorrhea. We have also described our experiences of improved symptoms and recovery with allopathic medicines and have thereby reported the present case with a literature review.
A 60-year-old male patient was admitted to the emergency room with right upper quadrant abdominal pain that had gradually increased in severity beginning 3 d earlier.
Fitz-Hugh-Curtis syndrome.
Hepatocellular carcinoma (right upper quadrant abdominal pain) -gastroscopy, colonoscopy, abdominal computed tomography (CT), and tumor marker test.
Aspartate aminotransferase was 52 IU/L and Alanine aminotransferase was 47 IU/L.
Abdominal CT showed linear capsular enhancement of the inferior segment of the right lobe is visible on an arterial phase.
Blood culture tests, urine culture tests, and PCR of sexually transmitted disease-causing microbes were negative.
Empirical intravenous antibiotics were administered, maintained oral medication.
Fitz-Hugh-Curtis syndrome occurs rarely in male. Cases reported in English and Korean literature were reviewed.
Fitz-Hugh-Curtis syndrome is a type of perihepatitis that causes liver capsular infection without infecting the hepatic parenchyma or pelvis is known to be locally aggressive and requires extensive surgical resection.
Fitz-Hugh-Curtis syndrome was considered as sexually transmitted disease. Although causative pathogen was not proven, we diagnosed and treated patient.
This article can nicely contribute to increasing the awareness of Fitz-Hugh-Curtis syndrome.
P- Reviewer: Ocker M S- Editor: Ma YJ L- Editor: A E- Editor: Wang CH
| 1. | Curtis AH. A cause of adhesions in the right upper quadrant. JAMA. 1930;94:1221-1222. [DOI] [Full Text] |
| 2. | Fitz-hugh Jr T. Acute gonococcic peritonitis of the right upper quadrant in women. JAMA. 1934;102:2094-2096. [RCA] [DOI] [Full Text] [Cited by in Crossref: 140] [Cited by in RCA: 139] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 3. | Müller-Schoop JW, Wang SP, Munzinger J, Schläpfer HU, Knoblauch M, Tammann RW. Chlamydia trachomatis as possible cause of peritonitis and perihepatitis in young women. Br Med J. 1978;1:1022-1024. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 111] [Cited by in RCA: 122] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 4. | Wang SP, Eschenbach DA, Holmes KK, Wager G, Grayston JT. Chlamydia trachomatis infection in Fitz-Hugh-Curtis syndrome. Am J Obstet Gynecol. 1980;138:1034-1038. [PubMed] |
| 5. | Wølner-Hanssen P, Svensson L, Weström L, Mårdh PA. Isolation of Chlamydia trachomatis from the liver capsule in Fitz-Hugh-Curtis syndrome. N Engl J Med. 1982;306:113. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 22] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 6. | Kimball MW, Knee S. Gonococcal perihepatitis in a male. The Fitz-Hugh--Curtis syndrome. N Engl J Med. 1970;282:1082-1084. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 53] [Cited by in RCA: 57] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 7. | Nishie A, Yoshimitsu K, Irie H, Yoshitake T, Aibe H, Tajima T, Shinozaki K, Nakayama T, Kakihara D, Matsuura T. Fitz-Hugh-Curtis syndrome. Radiologic manifestation. J Comput Assist Tomogr. 2003;27:786-791. [PubMed] |
| 8. | Joo SH, Kim MJ, Lim JS, Kim JH, Kim KW. CT diagnosis of Fitz-Hugh and Curtis syndrome: value of the arterial phase scan. Korean J Radiol. 2007;8:40-47. [PubMed] |
| 9. | Woo SY, Kim JI, Cheung DY, Cho SH, Park SH, Han JY, Kim JK. Clinical outcome of Fitz-Hugh-Curtis syndrome mimicking acute biliary disease. World J Gastroenterol. 2008;14:6975-6980. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 10. | Baek HC, Bae YS, Lee KJ, Kim DH, Bae SH, Kim DW, Yoon JB, Song CS. [A case of Fitz-Hugh-Curtis syndrome in a male]. Korean J Gastroenterol. 2010;55:203-207. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 8] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Lopez-Zeno JA, Keith LG, Berger GS. The Fitz-Hugh-Curtis syndrome revisited. Changing perspectives after half a century. J Reprod Med. 1985;30:567-582. [PubMed] |
| 12. | Owens S, Yeko TR, Bloy R, Maroulis GB. Laparoscopic treatment of painful perihepatic adhesions in Fitz-Hugh-Curtis syndrome. Obstet Gynecol. 1991;78:542-543. [PubMed] |
| 13. | Banerjee B, Rennison A, Boyes BE. Sonographic features in a case of Fitz-Hugh-Curtis syndrome masquerading as malignancy. Br J Radiol. 1992;65:342-344. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 14. | Money DM, Hawes SE, Eschenbach DA, Peeling RW, Brunham R, Wölner-Hanssen P, Stamm WE. Antibodies to the chlamydial 60 kd heat-shock protein are associated with laparoscopically confirmed perihepatitis. Am J Obstet Gynecol. 1997;176:870-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 15. | Ossewaarde JM, Rieffe M, Rozenberg-Arska M, Ossenkoppele PM, Nawrocki RP, van Loon AM. Development and clinical evaluation of a polymerase chain reaction test for detection of Chlamydia trachomatis. J Clin Microbiol. 1992;30:2122-2128. [PubMed] |
| 16. | Peter NG, Clark LR, Jaeger JR. Fitz-Hugh-Curtis syndrome: a diagnosis to consider in women with right upper quadrant pain. Cleve Clin J Med. 2004;71:233-239. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 81] [Cited by in RCA: 88] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 17. | Reichert JA, Valle RF. Fitz-Hugh-Curtis syndrome. A laparoscopic approach. JAMA. 1976;236:266-268. [PubMed] |
| 18. | Davidson AC, Hawkins DA. Pleuritic pain: Fitz Hugh Curtis syndrome in a man. Br Med J (Clin Res Ed). 1982;284:808. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Winkler WP, Kotler DP, Saleh J. Fitz-Hugh and Curtis syndrome in a homosexual man with impaired cell mediated immunity. Gastrointest Endosc. 1985;31:28-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.2] [Reference Citation Analysis (0)] |