Published online Nov 16, 2015. doi: 10.12998/wjcc.v3.i11.951
Peer-review started: May 9, 2015
First decision: June 3, 2015
Revised: June 27, 2015
Accepted: August 4, 2015
Article in press: August 7, 2015
Published online: November 16, 2015
Processing time: 187 Days and 14.1 Hours
A littoral cell angioma (LCA) is a primary vascular tumor of the spleen, that can have malignant potential and may present association with other malignancies. This is a case of LCA that was discovered incidentally in a 79-year-old woman who presented with a polycythemia at the time of consultation. The neoplasm was evaluated by ultrasound and computed tomography. The patient underwent a splenectomy that revealed LCA by pathological evaluation. The post-operative outcome was favorable with no complications or recurrent disease. This case presentation, clinical, radiographic, and pathological features of an uncommon splenic tumor can be studied in order to advance our knowledge in our understanding of LCA.
Core tip: We invite readers to read “laparoscopic splenectomy for littoral cell angioma of the spleen: Case report”, because we understand how pathological evaluation, after splenectomy, allows the definite diagnosis of this rare vascular neoplasm and given its potential malignancy and its association with other cancer types, splenectomy should be always performed.
- Citation: Marzetti A, Messina F, Prando D, Verza LA, Vacca U, Azabdaftari A, Rubinato L, Reale D, Favat M, Barbujani M, Agresta F. Laparoscopic splenectomy for a littoral cell angioma of the spleen: Case report. World J Clin Cases 2015; 3(11): 951-955
- URL: https://www.wjgnet.com/2307-8960/full/v3/i11/951.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i11.951
LCA was first reported by Falk et al[1] in 1991. They reviewed 200 surgical specimens of benign vascular tumors of the spleen and described 17 similar tumors correlated to the cells lining the red pulp splenic sinuses[1]. The littoral cell, the original one, presents both epithelial and histiocytic features[1].
Both sexes at any age are affected by this tumor. Usually patients are asymptomatic and the dignosis leads to an incidental founding. When patient presents symptoms they arise later and are splenomegaly, thrombocytopenia and anemia.
The neoplasm take its origin in the sinus of the red pulp of the spleen. These endothelial cells show the same immunoreactivity for markers CD31 and factor VIII, as showed by hemangiomas situated in different places.
Pathogenetic mechanism of this tumor is still uncertain, but has been thought as a possible one an immune system dysfunction because it has been observed an important association with autoimmune disorders like Crohn’s disease and metabolic diseases like Gaucher’s one[2,3].
Our patient, a 79-year-old woman, entered to the hospital for a polycythemia and during medical examinations it was discovered an hypointense lesion of the spleen and splenomegaly without hypersplenism (Figure 1). The patient did not present abdominal pain, nausea, episodes of vomite and changes in bowel habits. Her BMI was 35.8. The evaluation of EPO (5 IU/L) and genetic mutation of Jak2 (30%) revealed a chronic myeloproliferative syndrome. Ultrasound and computed tomography (CT) scan were performed. The ultrasound showed a round, solid, hypoechogenic mass of 45 mm of size at the superior pole of the spleen (Figure 2). A large, solitary, low-density lesion appeared in the early arterious phase of the contrast-enhanced CT (Figure 1). Laboratory tests showed normal liver enzymes and renal function, they only revealed an elevated count of platelets (587000/mcL) and a polycythemia (RBC = 5920000/mm, Hb = 17 g/dL) that was the primary reason why the patient entered to the Hospital.
Our patient underwent CT scan, that showed a hypoattenuating nodule of 4 cm × 5 cm of size with contrast enhancement on the arterious phase (Figure 1) and a hypointense lesion at Ultrasonography (Figure 2). Several studies have described the contrast-enhanced sonographic findings of various splenic lesions[4-6]. Characteristically benign vascular tumors show isoenhancement or a little hyperenhancement during the arterial phase and isoenhancement or hypoenhancement during the venous phase.
Rarely imaging can dignose the benign vascular neoplasm because many other splenic tumors mimic LCA. It is important a differential diagnosis with other splenic tumors that have a similar appearance with LCA like lymphangiomatosis, hamartoma, hemangiomatosis, hemangioendothelioma, hemangiopericytoma, and angiosarcoma; it has to be included in the differential diagnosis also lymphoma, metastases, Kaposi sarcoma and infectious diseases like Pneumocystis and Mycobacterium.
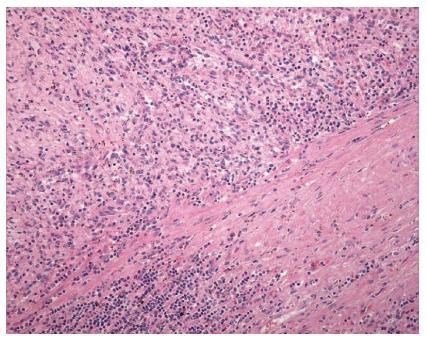
The neoplasm arises from the littoral cells in the splenic red pulp sinuses. Hemangiomas of other sites share the same immunoreactivity for vascular endothelial markers CD31 and factor VIII. It is interesting to observe that the tumor cells express histiocytic marker CD68 that explain why this neoplasm may begin in the splenic sinus lining cells or littoral cells.
Pathological evaluation, after laparoscopic splenectomy, allowed the definite diagnosis of this rare vascular neoplasm.
The surgical outcome was favorable without post-operative complications or recurrence.
Given certain diagnosis by pathological evaluation, associated to clinical features and imaging of an uncommon splenic tumor can be studied in order to advance our knowledge in our understanding of LCA.
The pathogenesis of LCA is nowadays still indefinite. We speculate as a possible pathogenic mechanism an immune system dysfunction, as demonstrates the association with autoimmune disorders like Gaucher’s disease and Crohn’s disease.
Pathological evaluation, after splenectomy, allows the definite diagnosis of this rare vascular neoplasm. Given its potential malignancy, splenectomy is usually performed.
The lining of vascular splenic sinuses, made by endothelial cells, presents both phagocytic and hematopoietic characteristics, that is the reason why they are thought to be unique since the 1930s[2].
The littoral cell of the spleen, the cell of origin, presents both epithelial and histiocytic features[7,8]. Overall the incidence of hemangioma of the spleen changes from 0.003% to 14% in autopsy reports[9], however the real incidence of LCA is unrecognized.
From a clinical point of view, the majority of patients with LCA are asymptomatic, while usually symptoms are anemia, thrombocytopenia both can be hypersplenism associated, splenomegaly, or unrecognized fever[10].
Abdominal pain can be also the main symptom at the time of consultation, otherwise the neoplasm is an incidental finding[11].
Our patient infact, entered to the hospital for a polycythemia and during medical examinations it was discovered an hypointense lesion of the spleen and splenomegaly without hypersplenism. She did not describe episodes of abdominal pain.
Normally, splenectomy performed for other reasons leads to diagnosis of LCA.
Only a minority of patients presents with splenomegaly, fever and features of hypersplenism like anemia and thrombocytopenia[12].
The vascular neoplasm can look like a single or multiple lesions in the spleen, while a massive splenomegaly can mimic a pancreatic tumor.
Recently LCA has been associated with tumors of the colon, kidney, pancreas, lung and ovary[13]. Have been described also associations with leiomyosarcoma, melanoma and lymphoma. Considering this malignancy association in patients with LCA, it should be always excluded visceral tumor.
The laparoscopic approach permitted to operate an old age, obese and cardiopathic patient and to dismiss her in 6 d without any postoperative complication.
Reports[10] comparing laparoscopic splenectomy to open splenectomy for diagnosed diseases like idiopathic thrombocytopenic purpura, reveal superiority of miniinvasive procedure because of its several benefits of lower post-operative pain and quicker post-operative recovery. Kercher et al[11] found that a laparoscopic approach was beneficial for massive splenomegaly (defined as craniocaudal dimension ≥ 17 cm and weight ≥ 600 g), which is also supported by our experience with this patient. Brodsky et al[12] also support laparoscopic splenectomy for several splenic diseases, also in case of splenomegaly. Rosen et al[13] found laparoscopic splenectomy to be safe for benign and malignant hematologic conditions, including Idiopathic Thrombocytopenic Purpura and a case of LCA, with a conversion rate of 5%.
Our patient was discharged by postoperative day 2 and did not present any complication, so that splenectomy allowed the definite dignosis of LCA, without compromise the outcome in an old, cardiopathic, obese patient.
Pathological evaluation, after splenectomy, allows the definite diagnosis of this rare vascular neoplasm and given its potential malignancy, even though most of LCAs are benign, and its association with other cancer types, splenectomy should be always performed. So their differential diagnosis must observe primary and secondary malignancy.
This rare case shows the interest of studying vascular tumors of the spleen even most of all are incidental foundings.
Considering these concepts, gold standard management appears to be splenectomy (in our experience and in literature, laparoscopic approach reveals a better surgical outcome) and a strict follow-up to recognize synchronous tumors or metastatic lesions.
The authors’ patient, a 79-year-old woman, entered to the hospital for a polycythemia and during medical examinations it was discovered an hypointense lesion of the spleen and splenomegaly without hypersplenism (Figure 1). The patient did not present abdominal pain, nausea, episodes of vomite and changes in bowel habits.
Splenomegaly, polycythemia, chronic myeloproliferative syndrome, elevated counts of platelets.
Lymphangiomatosis, hamartoma, hemangiomatosis, hemangioendothelioma, hemangiopericytoma and angiosarcoma; lymphoma, metastases, Kaposi sarcoma and infectious diseases like Pneumocystis and Mycobacterium.
Laboratory tests showed normal liver enzymes and renal function, they only revealed an elevated count of platelets (587000/mcL) and a polycythemia (RBC = 5920000/mm, Hb = 17 g/dL) that was the primary reason why the patient entered to the Hospital.
CT scan showed a hypoattenuating nodule of 4 cm × 5 cm of size with contrast enhancement on the arterious phase, and US revealed an hypointense splenic lesion.
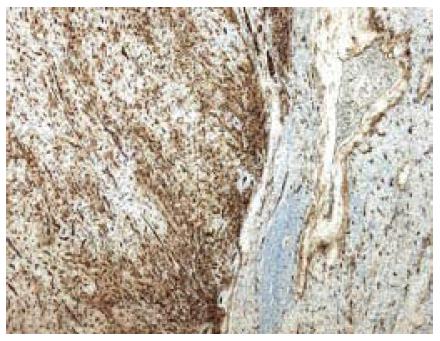
Splenectomy revealed at the pathological examination vascular structures anastomosed and positivity of vascular proliferation for immunohistochemical marker CD34 , diagnosing LCA (Figures 3 and 4).
Laparoscopic splenectomy.
Recently LCA has been associated with neoplasms of the colon, kidney, pancreas, lung and ovary. Have been described also associations with leiomyosarcoma, melanoma and lymphoma. Considering this malignancy association in patients with LCA, it should be always excluded visceral tumor.
LCA is primarily a benign tumor, however may be associated with others visceral neoplasms and may have malign potential.
Pathological evaluation, after splenectomy, allows the definite diagnosis of this rare vascular neoplasm because radiological and clinical foundings do not lead to a certain diagnosis. So, given its potential malignancy, even though the vast majority of LCAs are benign, and its association with other cancer types, splenectomy remains the golden standard in the managment of this disease.
Best management of this disease remains splenectomy (in our experience and in literature, laparoscopic approach reveals a better surgical outcome) and a strict follow-up to recognize synchronous tumors or metastatic lesions.
P- Reviewer: Amaro F, Santos-Antunes J, Tan XR S- Editor: Tian YL L- Editor: A E- Editor: Wang CH
| 1. | Falk S, Stutte HJ, Frizzera G. Littoral cell angioma. A novel splenic vascular lesion demonstrating histiocytic differentiation. Am J Surg Pathol. 1991;15:1023-1033. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 180] [Cited by in RCA: 160] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 2. | Gupta MK, Levin M, Aguilera NS, Pastores GM. Littoral cell angioma of the spleen in a patient with Gaucher disease. Am J Hematol. 2001;68:61-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 3. | Suvajdzić N, Cemerikić-Martinović V, Saranović D, Petrović M, Popović M, Artiko V, Cupić M, Elezović I. Littoral-cell angioma as a rare cause of splenomegaly. Clin Lab Haematol. 2006;28:317-320. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 4. | Görg C, Görg K, Bert T, Barth P. Colour Doppler ultrasound patterns and clinical follow-up of incidentally found hypoechoic, vascular tumours of the spleen: evidence for a benign tumour. Br J Radiol. 2006;79:319-325. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 5. | Catalano O, Sandomenico F, Matarazzo I, Siani A. Contrast-enhanced sonography of the spleen. AJR Am J Roentgenol. 2005;184:1150-1156. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 44] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 6. | Stang A, Keles H, Hentschke S, von Seydewitz CU, Dahlke J, Malzfeldt E, Braumann D. Differentiation of benign from malignant focal splenic lesions using sulfur hexafluoride-filled microbubble contrast-enhanced pulse-inversion sonography. AJR Am J Roentgenol. 2009;193:709-721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 49] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 7. | Heese J, Bocklage T. Specimen fine-needle aspiration cytology of littoral cell angioma with histologic and immunohistochemical confirmation. Diagn Cytopathol. 2000;22:39-44. [PubMed] |
| 8. | Kim HG, Park IS, Lee JI, Jeong S, Lee JW, Kwon KS, Lee DH, Kim PS, Kim HG, Shin YW. Littoral cell angioma (LCA) associated with liver cirrhosis. Yonsei Med J. 2005;46:184-188. [PubMed] |
| 9. | Harmon RL, Cerruto CA, Scheckner A. Littoral cell angioma: a case report and review. Curr Surg. 2006;63:345-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 33] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Tanoue K, Okita K, Akahoshi T, Konishi K, Gotoh N, Tsutsumi N, Tomikawa M, Hashizume M. Laparoscopic splenectomy for hematologic diseases. Surgery. 2002;131:S318-S323. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Kercher KW, Matthews BD, Walsh RW, Sing RF, Backus CL, Heniford BT. Laparoscopic splenectomy for massive splenomegaly. Am J Surg. 2002;183:192-196. [RCA] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 71] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 12. | Brodsky JA, Brody FJ, Walsh RM, Malm JA, Ponsky JL. Laparoscopic splenectomy. Surg Endosc. 2002;16:851-854. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 43] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 13. | Rosen M, Brody F, Walsh RM, Tarnoff M, Malm J, Ponsky J. Outcome of laparoscopic splenectomy based on hematologic indication. Surg Endosc. 2002;16:272-279. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 70] [Cited by in RCA: 75] [Article Influence: 3.3] [Reference Citation Analysis (0)] |