Published online Nov 16, 2015. doi: 10.12998/wjcc.v3.i11.946
Peer-review started: February 12, 2015
First decision: May 13, 2015
Revised: May 30, 2015
Accepted: August 30, 2015
Article in press: August 31, 2015
Published online: November 16, 2015
Processing time: 273 Days and 1.3 Hours
Thymoma and thymic carcinoma are rare epithelial tumors, which originate from the thymus gland. According to the World Health Organization there are “organotypic” (types A, AB, B1, B2, and B3) and “non-organotypic” (thymic carcinomas) thymomas. Type B3 thymomas are aggressive tumors, which can metastasize. Due to the rarity of these lesions, only 7 cases of extradural metastasis are described in the literature. We report the first and unique case of a man with cervical intradural B3 thymoma metastasis. A 46-year-old man underwent thymoma surgical removal. The year after the procedure he was treated for a parietal pleura metastasis. In 2006 he underwent cervical-dorsal extradural metastasis removal and C5-Th1 stabilization. Seven years after he came to our observation complaining left cervicobrachialgia and a reduction of strength of the left arm. He underwent a cervical spine magnetic resonance imaging, which showed a new lesion at the C5-C7 level. The patient underwent a surgery for the intradural B3 thymoma metastasis. Neurological symptoms improved although the removal was subtotal. He went through postoperative radiation therapy with further mass reduction. Spinal metastases are extremely rare. To date, only 7 cases of spinal extradural metastasis have been described in the literature. This is the first case of spinal intradural metastasis. Early individuation of these tumors and surgical treatment improve neurological outcome in patients with spinal cord compression. A multimodal treatment including neoadjuvant chemotherapy, surgery and postoperative radiation therapy seems to improve survival in patients with metastatic thymoma.
Core tip: To date, only 7 cases of spinal extradural thymoma metastasis have been described in the literature. We report the first case of spinal intradural thymoma metastasis. Early individuation of these tumors and surgical treatment improve neurological outcome in patients with spinal cord compression. A multimodal treatment including neoadjuvant chemotherapy, surgery and postoperative radiation therapy seems to improve survival in patients with metastatic thymoma.
- Citation: Marotta N, Mancarella C, Colistra D, Landi A, Dugoni DE, Delfini R. First description of cervical intradural thymoma metastasis. World J Clin Cases 2015; 3(11): 946-950
- URL: https://www.wjgnet.com/2307-8960/full/v3/i11/946.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i11.946
Thymoma and thymic carcinoma are uncommon epithelial lesions, which originate from the thymus gland. To date, the true incidence is not known, but it is estimated to be 0-15 cases/100000 people. Between the fifth and sixth decades of life, this pathology represents 0.2%-1.5% of all malignancies[1]. According to the World Health Organization there are “organotypic” (types A, AB, B1, B2, and B3) and “non-organotypic” (thymic carcinomas) thymomas. Types A, AB, B1 and B2 thymomas are benign tumors. Type B3 thymomas are aggressive tumors of intermediate malignancy[2]. Spinal metastases are very uncommon. In the literature, only 7 patients with spinal extradural metastasis have been described. We report the first and unique case of a man with cervical intradural B3 thymoma metastasis.
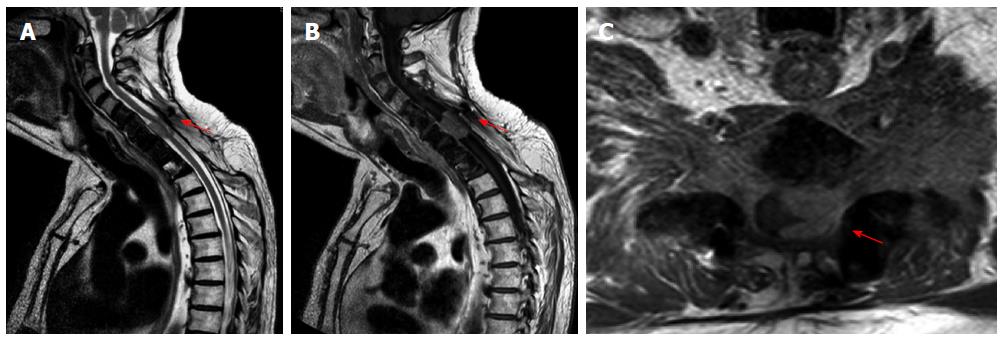
A thymoma was resected in a 46-year-old male in 1989. He did not submit himself to adjuvant therapy. A year after the procedure he underwent parietal pleura metastasis resection. The patient remained disease-free until 2006, when he complained a reduction of strength of the left arm, for the presence of a cervico-dorsal extradural metastasis. He underwent resection of the lesion and C5-Th1 stabilization (Figure 1). The lesion was totally removed (R0) and the dura mater appeared intact.
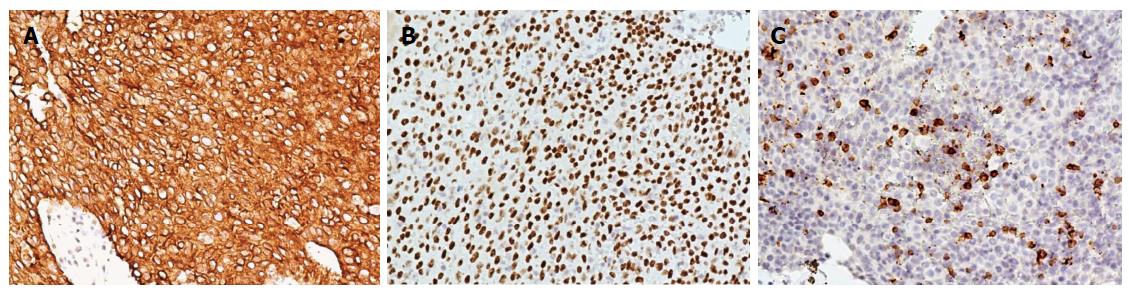
In 2013, the patient came to our observation complaining left cervicobrachialgia and a reduction of strength of the left arm. A cervical spine magnetic resonance imaging (MRI) showed a new lesion at the C5-C7 level (Figure 2). The lesion showed a homogeneous enhancement after gadolinium administration in the T1-weighted sequences, and enclosed the spinal cord, especially on the left side. From the imaging, it was not clear if the lesion was extradural or intradural. Intraoperatively, there was not pathological tissue in the epidural space; it appeared only after opening the dura mater. The patient underwent a sub-total resection, in order to preserve the spinal cord from the surgical manipulation. The lesion was intradural-extramedullary. It was adherent to the spinal cord surface in its lateral and anterior portions.
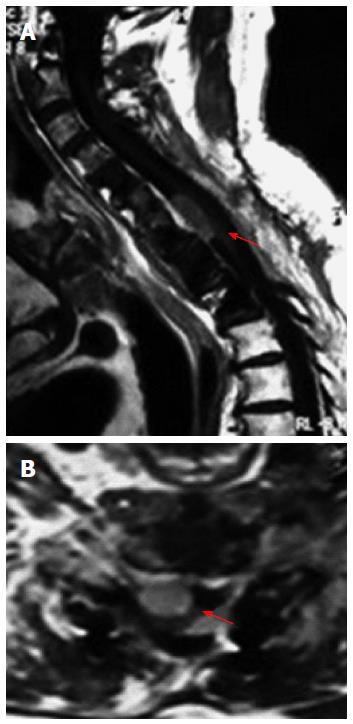
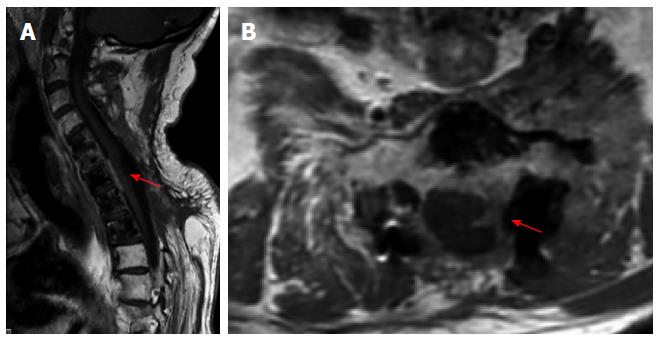
A spinal metastasis of the type B3 thymoma according to the World Health Organization 2004 was diagnosed (well-differentiated thymic carcinoma according to Marino and Muller-Hermelick)[3]. The immunohistochemical examination demonstrated positivity of neoplastic cells for CK19 and p63 and CD1a positive T-cells (Figure 3). Even if the resection was not total, no postoperative neurological deficits were observed. After 3 mo, the cervico-thoracic spine MRI showed a small residual tumor, especially anteriorly to the cervical spinal cord (Figure 4). Subsequently, focal radiotherapy (25.5 grays) was given. Cervical MRI after radiation treatment showed almost total disappearance of the mass (Figure 5). The patient is free of symptoms.
A search was carried out about spinal thymoma metastasis in the English language literature. We excluded one work because it is available only in Japanese language[4] and another because it did not report sufficient data to be included in our series. We used the following key words: “thymoma metastasis”, “thymic carcinoma”, “spinal cord compression”, and “spinal metastasis”. The data were extracted according to these parameters: (1) author and year of publication; (2) age; (3) sex; (4) time to spinal metastasis; (5) site of spinal metastasis; (6) sign and symptoms; (7) surgery; (8) follow-up; (9) radiotherapy; and (10) classification of histological type of the thymoma[5-9].
We found 6 papers, in which 7 cases were described. We included our case in the review, for a total number of 8 cases of spinal thymoma metastasis. Four patients were male and 3 were female. About the age, the average was 51.4 years old (range, 29-70 years). The median time from thymoma diagnosis to spinal metastasis was 7.9 years (range, 1-17 years); in one case the spinal metastasis was diagnosed before primary tumor; the case with longer time to spinal metastasis was our case. The spinal metastases were localized at the thoracic level in 4 cases, at the cervico-thoracic site in 1 case, cervical level in 2 cases, and lumbar level in 1 case. Patients presented symptoms related to the thymoma in 2 cases (myasthenia gravis); in all cases they had neurological symptoms related to the spinal metastasis (motor deficit, sensitive deficit or pain). All patients underwent surgical treatment. During the follow-up, 3 patients died after 3 mo, 5 mo and 2 years, respectively; 4 patients survived with a time of follow-up from 9 mo to 8 years (our case). Five patients did not receive radiation therapy, and 2 underwent RT. Histological diagnosis was not based on the actual WHO classification in 2 cases; the histological subtype was B2 in 1 case, B3 in 2 cases, and C in 2 cases.
Thymoma and thymic carcinoma are uncommon epithelial lesions, which originate from the thymus gland. Thymoma is a rare tumor, commonly associated with the myasthenia gravis (15%); local dissemination occurs quickly, but distant spinal metastasis may occur up to 16 years after the diagnosis of thymomas. They can metastasize to the pleura regional nodes, liver and lung. Spinal metastases are very uncommon. In the literature, only 7 patients with spinal extradural metastasis have been described. We report a unique case of spinal intradural metastasis. On MRI, the vertebral metastases appear hypointense on T1-weighted images and hyperintense on T2-weighted images. Infiltration of the paravertebral muscles and vertebral elements, evident on axial views, is possible. Imaging after gadolinium administration shows an important enhancement. A computed tomography scan shows infiltration of the vertebral body, with both osteolytic and osteoblastic lesions. The spinal metastasis can cause, in fact, vertebral collapse, spinal instability and neurological deterioration. Early diagnosis and surgery have the goal to control pain and reduce motor deficits. It is fundamental to take in account that an invasive thymoma can metastasize both extradurally and intradurally, because patient’s survival may be extended by an early diagnosis followed by an appropriate treatment.
We report the first case of spinal intradural metastasis. It is not yet known the gold standard of treatment, but a multimodal treatment which includes neoadjuvant chemotherapy, surgery and postoperative radiotherapy seems to improve survival in patients with metastatic thymoma.
Left cervicobrachialgia and a reduction of strength of the left arm.
It is fundamental to take in account that an invasive thymoma can metastasize both extradurally and intradurally.
The lesion showed a homogeneous enhancement after gadolinium administration in the T1-weighted sequences, and enclosed the spinal cord, especially on the left side.
A spinal metastasis of the type B3 thymoma according to the World Health Organization 2004 was diagnosed (well-differentiated thymic carcinoma according to Marino and Muller-Hermelick).The immunohistochemical examination demonstrated positivity of neoplastic cells for CK19 and p63 and CD1a positive T-cells.
Surgical sub-total resection and focal radiotherapy.
The spinal metastasis can cause, in fact, vertebral collapse, spinal instability and neurological deterioration. Early diagnosis and surgery have the goal to control pain and reduce motor deficits.
Extradural, outside the dura mater.
Multimodal treatment which includes neoadjuvant chemotherapy, surgery and post-operatory radiotherapy seems to improve survival in patients with metastatic thymoma.
The present case report is worth publishing, as it documents an extremely rare case of an intradural thymoma metastasis.
P- Reviewer: Sotelo J, Takahashi H, Widmann G S- Editor: Tian YL L- Editor: Wang TQ E- Editor: Wang CH
| 1. | Engels EA, Pfeiffer RM. Malignant thymoma in the United States: demographic patterns in incidence and associations with subsequent malignancies. Int J Cancer. 2003;105:546-551. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 327] [Cited by in RCA: 347] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 2. | Okumura M, Ohta M, Tateyama H, Nakagawa K, Matsumura A, Maeda H, Tada H, Eimoto T, Matsuda H, Masaoka A. The World Health Organization histologic classification system reflects the oncologic behavior of thymoma: a clinical study of 273 patients. Cancer. 2002;94:624-632. [PubMed] |
| 3. | Marino M, Müller-Hermelink HK. Thymoma and thymic carcinoma. Relation of thymoma epithelial cells to the cortical and medullary differentiation of thymus. Virchows Arch A Pathol Anat Histopathol. 1985;407:119-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 304] [Cited by in RCA: 249] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 4. | Akamatsu H, Tsukuura T, Matsunaga H, Suzuki A. [Study of combination therapy for thymoma: a case of stage IV which presented as total spinal block caused by epidural metastasis and which preoperative combination therapy was effective for minimizing the tumor]. Kyobu Geka. 1993;46:1156-1160. [PubMed] |
| 5. | Alafaci C, Salpietro FM, Grasso G, Passalacqua M, Lucerna S, Romano A, Tomasello F. Spinal cord compression by a metastasizing thymoma. Acta Neurochir (Wien). 1999;141:215-216. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Farin A, Aryan HE, Abshire BB. Thymoma metastatic to the extradural spine. J Clin Neurosci. 2005;12:824-827. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 12] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Liu T, Qiu G, Tian Y. Thymic carcinoma with primary spine metastasis. J Clin Neurosci. 2011;18:840-842. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 8. | Toba H, Kondo K, Takizawa H, Tangoku A. Recurrent thymoma with a pleural dissemination invading the intervertebral foramen. Eur J Cardiothorac Surg. 2009;35:917-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 9. | Hong B, Nakamura M, Hartmann C, Brandis A, Ganser A, Krauss JK. Delayed distant spinal metastasis in thymomas. Spine (Phila Pa 1976). 2013;38:E1709-E1713. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.8] [Reference Citation Analysis (0)] |