Published online Oct 16, 2015. doi: 10.12998/wjcc.v3.i10.915
Peer-review started: February 10, 2015
First decision: April 24, 2015
Revised: June 12, 2015
Accepted: August 28, 2015
Article in press: September 7, 2015
Published online: October 16, 2015
Processing time: 250 Days and 17.3 Hours
Primary mediastinal neuroendocrine tumors are a rare malignancy that accounts for < 10% of all mediastinal tumors. The case presented here involves a 52-year-old man who had been suffering for 3 mo from chronic cough, anorexia and substantial weight loss, as well as 2 wk of jaundice prior to his admission. A computed tomography scan showed a 4.3 cm × 6.6 cm mediastinal mass with multiple liver nodules scattered along both hepatic lobes. Endoscopic ultrasound showed a large heterogeneous hypoechoic mass at the mediastinum with multiple target-like nodules in the liver. Fine-needle aspiration specimens revealed numerous, small, round cells with hyperchromatic nuclei, scarce cytoplasm, and frequent mitotic features. Immunohistochemical study revealed positive results for AE1/AE3, CD56 and chromogranin A, with negative findings for synaptophysin, CK20, vimentin, CK8/18 and CD45. The patient was subsequently diagnosed with a poorly differentiated neuroendocrine carcinoma, small cell type. A bone marrow biopsy also revealed extensive involvement by the carcinoma.
Core tip: Neuroendocrine tumors are rare tumors that arise from the gastrointestinal tract and bronchopulmonary system. Primary mediastinal neuroendocrine tumors are exceptionally rare malignancies, accounting for < 10% of all mediastinal tumors. The common clinical manifestation of this rare tumor is a mediastinal mass, but the condition can mimic lymphoma in advanced cases. The liver is the most common site of metastasis.
- Citation: Nawarawong N, Pongpruttipan T, Aswakul P, Prachayakul V. Mediastinal small cell carcinoma with liver and bone marrow metastasis, mimicking lymphoma. World J Clin Cases 2015; 3(10): 915-919
- URL: https://www.wjgnet.com/2307-8960/full/v3/i10/915.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v3.i10.915
The most common malignancy of the mediastinum is Hodgkin’s lymphoma, which usually involves the anterior mediastinum and typically presents as adjacent organ invasion, superior vena cava obstruction, pleural effusion, or erosion of the sternum. The most common site of metastasis for Hodgkin’s disease is the liver[1]. In contrast, primary mediastinal neuroendocrine tumors are a rare malignancy that account for < 10% of all mediastinal tumors, with a reported incidence of 0.2-2.0 per 100000 people. These tumors are typically detected as incidental findings from chest radiography, as 40%-70% of advanced cases present with chronic cough, chest pain, dyspnea, or superior vena cava obstruction syndrome[2].
According to Travis[3], pulmonary neuroendocrine tumors are classified as: (1) typical carcinoid tumors; (2) atypical carcinoid tumors; (3) large cell neuroendocrine carcinomas; and (4) small cell neuroendocrine carcinomas. The prognoses of these mediastinal neuroendocrine tumors differ, with typical carcinoids associated with the best prognosis due to their slow growth and late metastasis, and the worst prognosis found with small cell neuroendocrine tumors[4]. Only a few cases of these tumors have been reported, with the liver as the most common site of metastasis[5,6]. This report describes a rare case involving a mediastinal mass with clinical manifestations mimicking lymphoma. To our knowledge, this is the first case report of primary neuroendocrine carcinoma with bone marrow and liver metastases.
A 52-year-old man presented to our hospital with a chronic cough, anorexia and substantial weight loss that had occurred over the previous 3 mo. He also presented with painless jaundice that had appeared 2 wk prior to his admission. He reported that he was a heavy smoker and had not experienced fever or shivering. His physical exam showed marked pallor and moderate jaundice, with a normal chest examination. The abdominal examination revealed hepatomegaly without splenomegaly and a negative finding for peripheral lymphadenopathy. Laboratory blood tests showed marked anemia with 6.8 g/dL hemoglobin (reference range: 12.0-18.0 g/dL), and normal white blood cell (7.7 × 103 cells/μL; reference range: 4-11 × 103 cells/μL) and reduced platelet (139 × 103 cells/μL; reference range: 150-440 × 103 cells/μL) counts. Liver chemistry results were as follows: total bilirubin, 4.2 mg/dL (reference range: 0-1.2 mg/dL); direct bilirubin, 3.7 mg/dL (reference range: 0-0.3 mg/dL); aspartate transaminase, 138 U/L (reference range: 0-32 U/L); alanine transaminase, 141 U/L (reference range: 0-32 U/L); and alkaline phosphatase, 403 U/L (reference range: 35-105 U/L). A markedly elevated lactate dehydrogenase level was noted at 3971 U/L (reference range: 240-480 U/L). Carcinoembryonic antigen measured 3.1 ng/mL (reference range: 0-5.0 ng/mL), with carbohydrate antigen 19-9 at 60.6 U/mL (reference range: 0-37.0 U/mL) and alpha-fetoprotein at 3.02 ng/mL (reference range: 1.09-8.04 ng/mL). The anti-HIV test was negative.
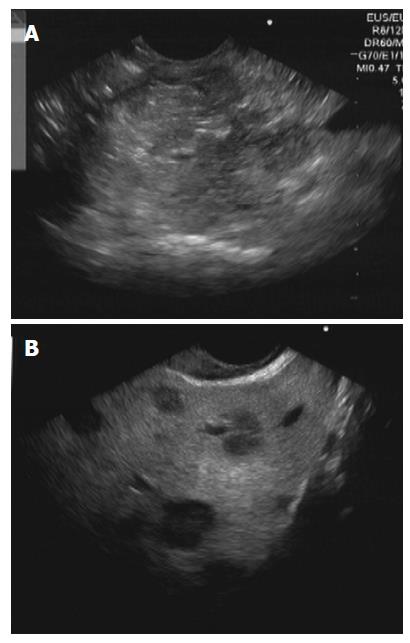
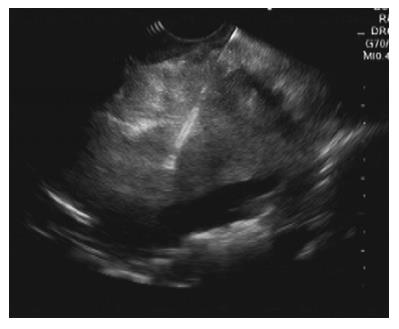
A computed tomography (CT) scan of the chest and upper abdomen showed a 4.3 cm × 6.6 cm mediastinal mass (Figure 1) with multiple liver nodules scattered along both hepatic lobes without any noteworthy pulmonary lesions. The provisional diagnosis was lymphoma, and the patient was therefore scheduled for endoscopic ultrasound and tissue sample collection. After deep sedation was induced using intravenous propofol with full anesthetic monitoring, a curvilinear endoscopic ultrasound scope (EG530UT2; Fujifilm, Minato-ku, Tokyo, Japan) was used for scanning. The echoview showed a large heterogeneous hypoechoic mass > 6 cm in diameter at the mediastinum, with multiple target-like nodules in the liver (Figure 2). Next, fine-needle aspiration of the mediastinal mass was performed with four passes using a 22-gauge needle (EchoTip Procore; Cook Group Inc., Bloomington, IN, United States) (Figure 3). A diagnosis of primary mediastinal lymphoma with liver metastasis was strongly suspected.
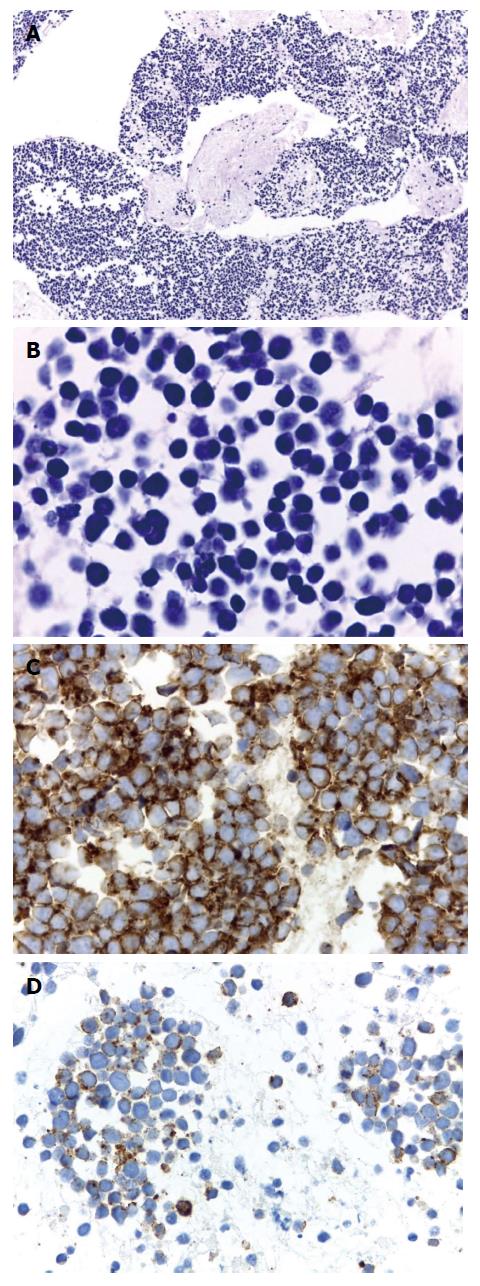
The patient’s clinical status worsened despite administration of intravenous corticosteroids. The histopathologic results finally revealed numerous small, individual, round cells with hyperchromatic nuclei, scarce cytoplasm, and frequent mitotic features. An immunohistochemical study was positive for AE1/AE3, CD56 and chromogranin A (Figure 4), but negative for synaptophysin, CK20, vimentin, CK8/18 and CD45. Based on these findings, a diagnosis of poorly differentiated neuroendocrine carcinoma, small cell type was made.
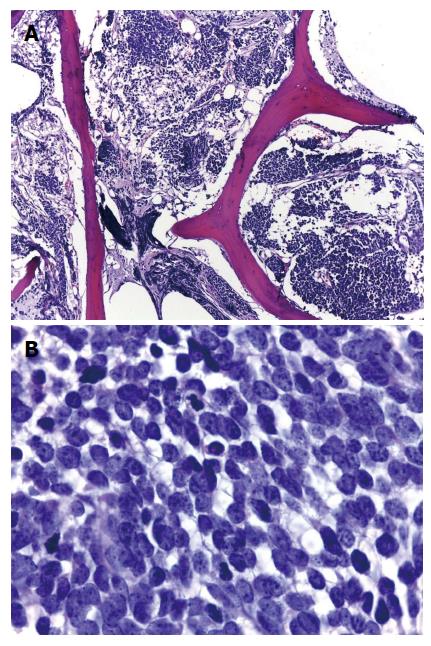
A bone marrow biopsy was also performed, which showed extensive involvement by the carcinoma (Figure 5). However, intravenous chemotherapy was not administered due to the poor performance status at this point. The patient subsequently died a few weeks later, after developing progressive liver failure, edema in both legs, and a sudden onset of dyspnea and cyanosis, due to a suspected acute pulmonary embolism. No autopsy was performed in this case.
Neuroendocrine tumors are rare tumors that typically involve the gastrointestinal tract and the bronchopulmonary system. Primary mediastinal neuroendocrine tumors are extremely rare[7-13], and can present as lymphoma, particularly Hodgkin’s type. Indeed, the case described here initially presented with similar clinical symptoms, such as chronic cough, anorexia, weight loss, and a bulky mediastinal mass with liver metastasis. However, a final diagnosis of a poorly differentiated neuroendocrine tumor, small cell type was made after histopathologic and immunohistochemical study. The multiple liver nodules were strong indicators of liver metastasis, and this is the first reported case of mediastinal neuroendocrine tumor with liver and bone marrow metastases.
Li et al[14] reported a case series of six patients with primary small cell neuroendocrine carcinoma and found that most of the cases were in advanced stages, with tumors > 6 cm. Moreover, more than two-thirds of those cases involved the anterior-middle mediastinum with 44% scattered punctate calcification on CT. However, the immunohistochemical studies were positive for different markers, indicating the tumors had differentiated from a carcinoid tumor, mediastinal lymphoma, germ cell tumor of mediastinum, and thymoma. The poor prognosis for primary small cell neuroendocrine carcinoma was demonstrated by only half of the cases responding to chemotherapy, and the 2-year mortality rate of 50%[14]. The patient described in this case report had an advanced stage neuroendocrine tumor with fatal outcome. Definitive treatment for this small cell carcinoma should be guided by the definite histopathological and immunohistochemistry results.
A 52-year-old man presented with a chronic cough, weight loss, anemia and progressive jaundice.
Metastatic small cell neuroendocrine tumor with liver and bone marrow involvement.
Lymphoma; Carcinoid tumor; Mediastinal lymphoma; Germ cell tumor of mediastinum; Thymoma.
Hemoglobin, 6.8 g/dL; White blood cell count, 7.7 × 103 cells/μL; Platelet count, 139 × 103 cells/μL; Total bilirubin, 4.2 mg/dL; Direct bilirubin, 3.7 mg/dL; Aspartate transaminase, 138 U/L; Alanine transaminase, 141 U/L; Alkaline phosphatase, 403 U/L; Lactate dehydrogenase, 3971 U/L; Carcinoembryonic antigen, 3.11 ng/mL; Carbohydrate antigen 19-9, 60.62 U/mL; Alpha-fetoprotein, 3.02 ng/mL.
Computed tomography scan of the chest and upper abdomen showed a 4.3 cm × 6.6 cm mediastinal mass with multiple liver nodules scattered along both hepatic lobes without any marked pulmonary lesions.
Poorly differentiated neuroendocrine carcinoma, small cell type.
Palliative treatment.
Neuroendocrine tumors are a very rare malignancy of the mediastinum, and there are very few reports in the literature.
Mediastinal neuroendocrine tumors may have a clinical presentation similar to lymphoma of the mediastinum. Histologic diagnosis and immunohistochemical study are crucial for definite diagnosis.
The authors describe a case of primary mediastinal neuroendocrine tumor with liver and bone marrow metastases, which mimicked lymphoma. This is a rare tumor with malignant lymphoma as the primary differential diagnosis.
P- Reviewer: Moyana TN, Zhao HD S- Editor: Yu J L- Editor: O’Neill M E- Editor: Jiao XK
| 1. | Macchiarini P, Ostertag H. Uncommon primary mediastinal tumours. Lancet Oncol. 2004;5:107-118. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 104] [Cited by in RCA: 84] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 2. | Caplin ME, Baudin E, Ferolla P, Filosso P, Garcia-Yuste M, Lim E, Oberg K, Pelosi G, Perren A, Rossi RE. Pulmonary neuroendocrine (carcinoid) tumors: European Neuroendocrine Tumor Society expert consensus and recommendations for best practice for typical and atypical pulmonary carcinoids. Ann Oncol. 2015;26:1604-1620. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 514] [Cited by in RCA: 466] [Article Influence: 46.6] [Reference Citation Analysis (0)] |
| 3. | Travis WD. Pathology and diagnosis of neuroendocrine tumors: lung neuroendocrine. Thorac Surg Clin. 2014;24:257-266. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 87] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 4. | Chong S, Lee KS, Chung MJ, Han J, Kwon OJ, Kim TS. Neuroendocrine tumors of the lung: clinical, pathologic, and imaging findings. Radiographics. 2006;26:41-57; discussion 57-58. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 147] [Cited by in RCA: 125] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 5. | Wick MR, Rosai J. Neuroendocrine neoplasms of the mediastinum. Semin Diagn Pathol. 1991;8:35-51. [PubMed] |
| 6. | Del Vescovo R, Cazzato RL, Battisti S, D’Agostino F, Vincenzi B, Grasso RF, Zobel BB. Neuroendocrine tumor presenting like lymphoma: a case report. J Med Case Rep. 2011;5:506. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 7. | Cheung TT, Chok KS, Chan AC, Tsang S, Dai JW, Lang BH, Yau T, Chan SC, Poon RT, Fan ST. Long term survival analysis of hepatectomy for neuroendocrine tumour liver metastases. ScientificWorldJournal. 2014;2014:524045. [PubMed] |
| 8. | Modlin IM, Lye KD, Kidd M. A 5-decade analysis of 13,715 carcinoid tumors. Cancer. 2003;97:934-959. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1848] [Cited by in RCA: 1851] [Article Influence: 84.1] [Reference Citation Analysis (1)] |
| 9. | Lim KH, Huang MJ, Yang S, Hsieh RK, Lin J. Primary carcinoid tumor of prostate presenting with bone marrow metastases. Urology. 2005;65:174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Khan M, Nizami S, Mirrakhimov AE, Maughan B, Bishop JA, Sharfman WH. Primary small cell neuroendocrine carcinoma of paranasal sinuses. Case Rep Med. 2014;2014:874719. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | Wang HY, Zou J, Zhou GY, Yan JQ, Liu SX. Primary small cell neuroendocrine carcinoma of the tonsil: a case report and review of the literature. Int J Clin Exp Pathol. 2014;7:2678-2682. [PubMed] |
| 12. | Case Reports In Dentistry. Retracted: Primary small cell undifferentiated (neuroendocrine) carcinoma of the maxillary sinus. Case Rep Dent. 2014;2014:609802. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Koo YJ, Kim DY, Kim KR, Kim JH, Kim YM, Kim YT, Nam JH. Small cell neuroendocrine carcinoma of the endometrium: a clinicopathologic study of six cases. Taiwan J Obstet Gynecol. 2014;53:355-359. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 18] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 14. | Li J, Xia T, Zhang W, He P, Guan Y. Primary small cell neuroendocrine carcinoma of the mediastinum: computed tomography and histopathological correlation. J Comput Assist Tomogr. 2014;38:174-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |