Published online Sep 16, 2014. doi: 10.12998/wjcc.v2.i9.466
Revised: April 25, 2014
Accepted: July 12, 2014
Published online: September 16, 2014
Processing time: 195 Days and 21.8 Hours
A 75-year-old male patient had stable angina pectoris. After coronary angiography we decided to perform a coronary artery bypass graft surgery. Twenty years ago the patient underwent radical cystectomy and bilateral ureterosigmoidostomy because of bladder cancer. After that, his micturition was via the rectum. We did not experience that before. As is known, monitoring of urine output is very important after cardiac surgery. The patient was consulted with an urologist for how to monitor urine output in him. Transrectal catheterization was recommended for our follow-up, but before the catheterization bowel cleansing is necessary. Four-vessel on-pump coronary artery bypass graft surgery was performed without any problem. Peroperative urine volume and arterial blood gas results were normal. Urine output is a sensitive variable reflecting the patient’s effective blood volume and tissue perfusion. Urinary catheterization is a standard for all cardiac surgeries, and it allows the patients’ urine to drain freely from the bladder for collection. Monitoring of urine output in patients with ureterosigmoidostomy is impossible by standard urinary catheterization method. In this case we performed transrectal catheterization for Urine flow follow-up. Urine flow follow-up is essential after the open-heart surgery and it can be measured in different ways, as in our case.
Core tip: With this case, we had experience that we can monitor urine output in different ways rather than urethral catheterization such as catheterization in a transrectal way that we had to do in a patient who had ureterosigmoidostomy.
- Citation: Haberal I, Ozsoy D, Sipahi E, Mert M. Coronary artery bypass graft surgery in a patient with ureterosigmoidostomy. World J Clin Cases 2014; 2(9): 466-468
- URL: https://www.wjgnet.com/2307-8960/full/v2/i9/466.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i9.466
Urine output is a sensitive variable reflecting the patient’s effective blood volume and tissue perfusion[1]. Urinary catheterization is a standard for all cardiac surgeries, and it allows the patients’ urine to drain freely from the bladder for collection. Monitoring of urine output in patients with ureterosigmoidostomy is impossible by standard urinary catheterization method. We could not find any such case report in the literature. Hence we decided to write this case report to explain how we can monitor urine output and which complications may occur after coronary artery bypass graft surgery operation in patients with ureterosigmoidostomy.
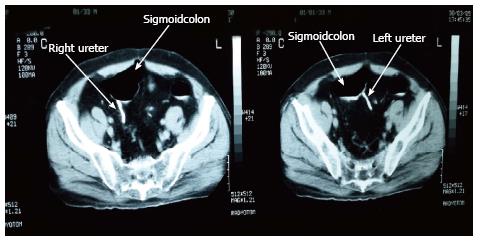
A 75-year-old male patient had stable angina pectoris. After coronary angiography we decided to perform a coronary artery bypass graft surgery. Preoperative laboratory tests were normal. Twenty years ago the patient underwent radical cystectomy and bilateral ureterosigmoidostomy because of bladder cancer (Figure 1). His urologist confirmed that, he was fully cured after this surgery. After that, his micturition was via the rectum. We did not experience that before. As is known, monitoring of urine output is very important after cardiac surgery. The patient was consulted with an urologist for how to monitor urine output in him. Transrectal catheterization was recommended for our follow-up, but before the catheterization bowel cleansing is necessary. After this recommendation we performed a high enema the night before the operation. A 24F urinary catheter was applied in a transrectal way as much as possible to the distal end. A 24F Foley urethral catheter with a 30 cc balloon was inflated to 50 cc in order to minimize the chance that the catheter will be pulled down through the sigmoid colon and then we could monitor urine output by this method perfectly. Four-vessel on-pump coronary artery bypass graft surgery was performed without any problem. Peroperative urine volume and arterial blood gas results were normal. The patient had respiratory problems postoperatively but hemodynamic parameters were normal. Third generation cephalosporins were used to prevent possible urosepsis during the catheterization. During the catheterization the patient was not fed via the enteral route. Urine flow was followed for three days until hemodynamic stability was achieved. The catheter was removed three days after the operation and the patient was transferred from intensive care unit to the ward four days after the operation. The patient was discharged from hospital nine days after the surgery without any problem.
Monitoring of urine output could improve the clinical management of cardiac patients and enable clinicians to early recognition of volume status, cardiac output and kidney injury. A urinary catheter is inserted preoperatively in the operation room and kept in place for a minimum of 24-48 h to monitor hourly urine flow. Catheterization is difficult in some patients such as those with prostatic hypertrophy. In some cases, consideration should be given to use of a trocar–introduced suprapubic catheter in adults, rather than a urethral catheter. Our patient was operated 20 years ago because of bladder cancer. Today, orthotopic urinary diversion is an essential component of the surgical procedure after cystectomy. Replacement with an orthotopic ileal neobladder should be the first choice if external urethral sphincter sparing surgery is possible, offering good long-term function, quality of life and patient’s acceptance with few complications[2,3]. However in our case, radical cystectomy and bilateral ureterosigmoidostomy were performed because of bladder cancer. Patients undergoing this procedure must be closely monitored for the development of hyperchloremic acidosis. This will occur in the majority of instances, and it is wise to initiate a bicarbonate replacement program at the outset[4]. After the coronary artery bypass graft surgery, apparent acidosis did not occur at the postoperative arterial blood gas follow-up, and this may be because ureterosigmoidostomy was performed 20 years ago. Obviously, all of such patients have exposure of the urinary tract to fecal flora. Most authors would advocate chronic antibacterial agent administration in all patients[5]. Third generation cephalosporins were used in our case to prevent possible urosepsis during the catheterization. Because of the definite concern for the occurrence of rectal cancer some 5 to 50 years (average 21 years) after ureterosigmoidostomy[6], it is suggested that patients with long-term ureterosigmoidostomy be subjected to annual colonic investigation. His urologist confirmed that he was fully cured after radical cystectomy and bilateral ureterosigmoidostomy. At colonoscopic investigations we could not determine any pathological results. In this case, paying particular attention to a few details both preoperatively and postoperatively, coronary artery bypass graft surgery was performed without any problem.
In conclusion, urine flow follow-up is essential after the open-heart surgery and it can be measured in different ways, as in our case.
A 75-year-old male patient with a history of ischemic heart disease presented with dispnea and angina.
Scar to inspection over suprapubic area.
Aortic dissection, pericarditis, and pneumothorax.
Hematologic and metabolic panels were normal.
Coronary angiography revealed multi-vessel coronary artery disease and computed tomography scan showed bilateral ureterosigmoidostomy.
Coronary artery disease with radical cystectomy and bilateral ureterosigmoidostomy operation because of bladder cancer.
Four-vessel on-pump coronary artery bypass graft surgery was performed without any problem.
Catheterization is difficult in some patients such as those with prostatic hypertrophy. In some cases, consideration should be given to use of a trocar–introduced suprapubic catheter in adults, rather than a urethral catheter.
Ureterosigmoidostomy is not widely used in patients with bladder cancer. Nowadays, orthotopic urinary diversion is an essential component of the surgical procedure after cystectomy.
Urinary output can be monitored transrectally in patients with ureterosigmoidostomy.
Authors describe the case of a patient undergoing CABG who had undergone radical cystectomy with ureterosigmoidostomy. Monitoring urine output is important in these patients, which was performed using a Foley catherther in the colon after bowel cleaning in this case. It is an unusual interesting clinical dilemma with good discussion.
P- Reviewer: Mehta Y S- Editor: Song XX L- Editor: Wang TQ E- Editor: Lu YJ
| 1. | Legrand M, Payen D. Understanding urine output in critically ill patients. Ann Intensive Care. 2011;1:13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 68] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 2. | Lee RK, Abol-Enein H, Artibani W, Bochner B, Dalbagni G, Daneshmand S, Fradet Y, Hautmann RE, Lee CT, Lerner SP. Urinary diversion after radical cystectomy for bladder cancer: options, patient selection, and outcomes. BJU Int. 2014;113:11-23. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 199] [Cited by in RCA: 228] [Article Influence: 20.7] [Reference Citation Analysis (0)] |
| 3. | Nagele U, Sievert KD, Merseburger AS, Anastasiadis AG, Stenzl A. Urinary Diversion Following Cystectomy. EAU Update Series 3. 2005;129-137. |
| 4. | Miller K, Matsui U, Hautmann R. The functional rectal bladder-prevention of hyperchloremic acidosis following vesico-sigmoidostomy in dogs. Urology. 1990;144:375-380. |
| 5. | Spirnak JP, Caldamone AA. Ureterosigmoidostomy. Urol Clin North Am. 1986;13:285-294. [PubMed] |