Published online Sep 16, 2014. doi: 10.12998/wjcc.v2.i9.463
Revised: May 23, 2014
Accepted: June 18, 2014
Published online: September 16, 2014
Processing time: 168 Days and 14.8 Hours
The objective of this study is to increase awareness of the rare presentation, diagnostic difficulties and management of glomus tympanicum of the middle ear. A 49 years old male, with a background of hypertension and epilepsy, presented with a two month history of left sided conductive hearing loss, pulsatile tinnitus and headache. Clinically and radiologically a diagnosis of glomus tympanicum was made. Intraoperatively, extensive osteogenesis of the middle ear resulting in ossicular fixation and erosion was found. This patient required a two stage operation for full clearance of disease. A stapedectomy drill was used to drill off the bony overgrowth surrounding the ossicles resulting in improved hearing thresholds and full clearance of the disease at two year follow up. Glomus tympanicum can result in new bone formation in the middle ear with resultant ossicular fixation and conductive hearing loss. This can be effectively treated surgically with restoration of hearing.
Core tip: Glomus tympanicum can result in new bone formation in the middle ear with resultant ossicular fixation and conductive hearing loss. This can be effectively treated surgically with restoration of hearing. We describe this previously unreported presentation of glomus tympanicum in the world literature (with reactive osteogenesis and resultant severe conductive hearing loss). We therefore believe our findings would be of interest to the readers of your journal and raise awareness of this as a differential diagnosis which may be under-recognised.
- Citation: Kumar G, Andreou Z, Virk JS, Owa A. Unusual presentation of glomus tympanicum tumour: New bone formation in the middle ear. World J Clin Cases 2014; 2(9): 463-465
- URL: https://www.wjgnet.com/2307-8960/full/v2/i9/463.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i9.463
Glomus tumours or paragangliomas are benign neoplasms that arise from paraganglionic tissue throughout the body with glomus tympanicum being the most common primary soft tissue tumour arising in the middle ear[1,2]. The paraganglionic system is a collection of cells derived from the neural crest and are found in the autonomic nervous system. They act as a source of catecholamines before the development of the adrenal medulla. The term “glomus” is a historical misnomer which was applied to these tumors before a true understanding of the characteristics of these tumors was understood. Extra-adrenal or craniocervical paraganglioma are distributed along the arteries and cranial nerves in head and neck region. Craniocervical paragangliomas can be broadly classified into temporal and vagal.
Temporal paragangliomas commonly arise from “paraganglion cells” along the course of Jacobson’s nerve or Arnold’s nerve[2]. They present as a soft tissue mass in the middle ear cavity which is often visible on otoscopy. Patients classically complain of pulsatile tinnitus and conductive hearing loss although depending on the extent of the disease they can experience imbalance, facial nerve palsy, otorrhoea or endocrine symptoms if the tumour is releasing catecholamines[3]. These clinical features lead to a need for further radiological investigations in the form of computed tomography and magnetic resonance imaging of the temporal bones to confirm the likely diagnosis and assess severity. A 24 h urine collection should be performed and analysed for vanillylmandelic acid (VMA) levels to determine whether indeed the lesion is endocrine-active[1-3].
We present a rare variant of a glomus tympanicum tumour that induced extensive osteogenesis in the middle ear causing severe conductive hearing loss secondary to ossicular fixation and erosion.
A 49 years old male presented to otolaryngology outpatient department with a 2 mo history of left-sided “throbbing” earache. He also complained of pulsatile tinnitus and worsening left sided hearing loss. His general practitioner initially diagnosed him with otitis externa and when his symptoms failed to improve he was referred for further specialist management. His past medical history included epilepsy and hypertension.
Examination revealed a red mass arising from behind his tympanic membrane in the attic area and a diagnosis of glomus tympanicum was suspected although the position of the lesion was slightly unusual for a glomus. A pure tone audiogram revealed a mild conductive deafness of 20db especially on high frequencies. A computed tomography (CT) scan of his temporal bone revealed a non-gravity dependent opacification with bony erosion and 24 h urine collection did not show elevated VMA levels indicating a non-secretory glomus tumour.
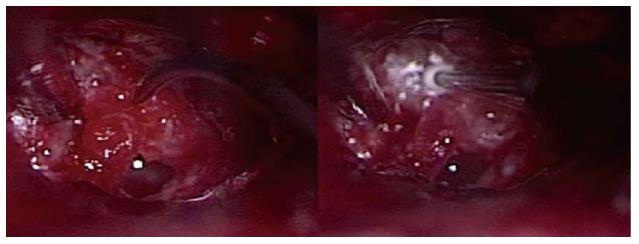
Multidisciplinary team and patient choice resulted in surgical management of this lesion. Intraoperatively, after exposing the middle ear, apart from inflamed mucosa there was no obvious soft tissue mass found. There was however a bony growth arising from the medial wall of the middle ear and extending between the incus and malleus handle encasing the anterior crura of stapes (Figure 1). After careful dissection the extra bone was peeled of the ossicles and sent for histology leaving the ossicular chain intact. The patient made a very good recovery and his conductive hearing loss improved with closure of the air-bone gap to 5db. Histology revealed thickened and sclerotic bone. The intervening connecting tissue traversing the bone was infiltrated by tumour consisting of hyperchromatic cells with rich vascular stroma and no signs of atypia or mitosis. A diagnosis of benign glomus tumour was made.
During follow up, (ADD COMMA) despite an initial mild improvement in his hearing, the patient developed a worsening conductive hearing loss with thresholds of 60-70db across most frequencies. Computed tomography imaging, 18 mo after his initial operation, (ADD COMMA) suggested recurrent disease and the patient required revision surgery.
Intra-operatively a recurrent bony overgrowth was identified which this time had encased the stapes superstructure and was causing malleo-incudal fixation. The disease could not be removed with a curette and so a stapedectomy drill was used to drill the overgrowth off the stapes superstructure. The malleus and incus were sacrificed and the ossicular chain was reconstructed with conchal cartillage. Histology once again demonstrated bone overgrowth with intervening tumour cells. The patient made a very good recovery and he has a sustained improved hearing of 40db two years postoperatively.
Glomus tumours are fairly rare with an incidence of around 1 per 1 million[4]. They are usually hypervascular tumours that arise within the jugular foramen of the temporal bone[1-4]. They characteristically present with conductive hearing loss and a pulsatile tinnitus as demonstrated in our case. Histologically, chief or granular cells (Type I) and sustentacular cells or satellite cells (Type II) are present in glomus tumours[2]. Management is dependent on the tumour extent and the patient’s fitness with the mainstay being surgery and radiotherapy[1-4]. Small tumours can be accessed via a transcanal approach with larger ones necessitating a post-auricular approach with mastoid exploration. The tumour is commonly a highly vascular soft tissue lesion which may require pre-operative embolization.
Bony overgrowth over a glomus tumour has not been previously reported in the world literature and as such represents a new clinical entity. The only other incidence of bone in the middle ear associated with a glomus tumour was reported by Yanagisawa et al[5], where a glomus tumour coexisted with otosclerosis in a patient. However, our patient did not show any histological features of otosclerosis in that his conductive hearing loss was unilateral, his ossicular chain was mobile after resection of the extra bone in the middle ear and his hearing improved post-operatively without the need for a stapes prosthesis. Furthermore, histology from the bone overgrowth confirmed glomus tumour cells intervening the bony overgrowth. All Fisch class I mesotympanic paragangliomas involve careful resection of tumour around the ossicles. We cleared osteogenesis around the stapes suprastructure using a stapedectomy drill, thus improving upon the incumbent conductive hearing loss. Another management option available in such cases would be removal of the glomus along with stapes suprastucture and reconstructing hearing using a total ossicular replacement prosthesis. Our treatment option, of drilling the bone around the ossicular chain and in particular the stapes, with a stapedectomy drill, proved successful in terms of hearing restoration (whilst ensuring tumour removal) and we propose this as a treatment modality for such rare cases.
In conclusion: (1) Glomus tumours or paragangliomas are rare tumours arising from paraganglionic tissue; (2) Glomus tympanicum tumours are the commonest soft tissue tumour of the middle ear; (3) These lesions typically present with pulsatile tinnitus and hearing loss; (4) A new clinical entity of osteogenesis in the middle ear is described - leading to ossicular fixation and erosion; and (5) Bony overgrowth can be managed by careful dissection off the ossicles or by use of a stapedectomy drill, resulting in improved hearing thresholds.
A 49 years old male with a two month history of left sided conductive hearing loss, pulsatile tinnitus and headache.
Examination revealed a red mass arising from behind his tympanic membrane in the attic area with an associated mild conductive deafness.
Differentials included glomus tympanicum although the mass was unusually located meaning cholesteatoma, schwannoma and meningioma remained possible.
Twenty-four hour urine collection did not show elevated VMA levels indicating a non-secretory glomus tumour.
Computed tomography scan of his temporal bone revealed a non-gravity dependent opacification with bony erosion.
Histology revealed thickened and sclerotic bone with intervening connecting tissue traversing the bone infiltrated by tumour consisting of hyperchromatic cells with rich vascular stroma and no signs of atypia or mitosis, leading to a diagnosis of benign glomus tumour.
Surgical excision with drilling of newly formed bone and reconstruction of hearing mechanism.
Glomus tumours are rare, hypervascular tumour that arises within the jugular foramen of the temporal bone. New bone formation in the middle ear has not previously been reported in the world literature.
VMA is Vanillylmandelic Acid, a metabolic by-product of norepinephrine and epinephrine.
Glomus tympanicum can result in new bone formation in the middle ear with resultant ossicular fixation and conductive hearing loss which can be effectively treated surgically with restoration of hearing.
The manuscript reports a clinical case about glomus tympanicum tumour related bone formation in middle ears leading to conductive hearing loss.
P- Reviewer: Cai KY, Horii A S- Editor: Ji FF L- Editor: A E- Editor: Lu YJ
| 1. | Sanna M, Fois P, Pasanisi E, Russo A, Bacciu A. Middle ear and mastoid glomus tumors (glomus tympanicum): an algorithm for the surgical management. Auris Nasus Larynx. 2010;37:661-668. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 53] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 2. | Kaylie DM, O’Malley M, Aulino JM, Jackson CG. Neurotologic surgery for glomus tumors. Otolaryngol Clin North Am. 2007;40:625-649, x. [PubMed] |
| 3. | Fayad JN, Keles B, Brackmann DE. Jugular foramen tumors: clinical characteristics and treatment outcomes. Otol Neurotol. 2010;31:299-305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 90] [Article Influence: 6.0] [Reference Citation Analysis (0)] |
| 4. | Moffat DA, Hardy DG. Surgical management of large glomus jugulare tumours: infra- and trans-temporal approach. J Laryngol Otol. 1989;103:1167-1180. [PubMed] |
| 5. | Yanagisawa E, Principato JJ. Glomus tympanicum tumor in an otosclerotic ear. Arch Otolaryngol. 1970;91:299-301. [PubMed] |