Published online Jul 16, 2014. doi: 10.12998/wjcc.v2.i7.272
Revised: February 25, 2014
Accepted: June 10, 2014
Published online: July 16, 2014
Processing time: 38 Days and 7.8 Hours
AIM: To determine the cut-off values of body mass index (BMI) and waist circumference to predict hypertension in adults in north India.
METHODS: A community based cross-sectional study was conducted in 801 subjects in Kanpur, aged 20 years and above, using multistage stratified random sampling technique. A pre-tested structured questionnaire was used to elicit the required information from the study participants and the diagnostic criteria for hypertension were taken according to the Seventh Joint National Committee Report on Hypertension (JNC-7). Receiver operating characteristic (ROC) analysis was used to estimate the cut-off values of BMI and waist circumference to predict hypertension.
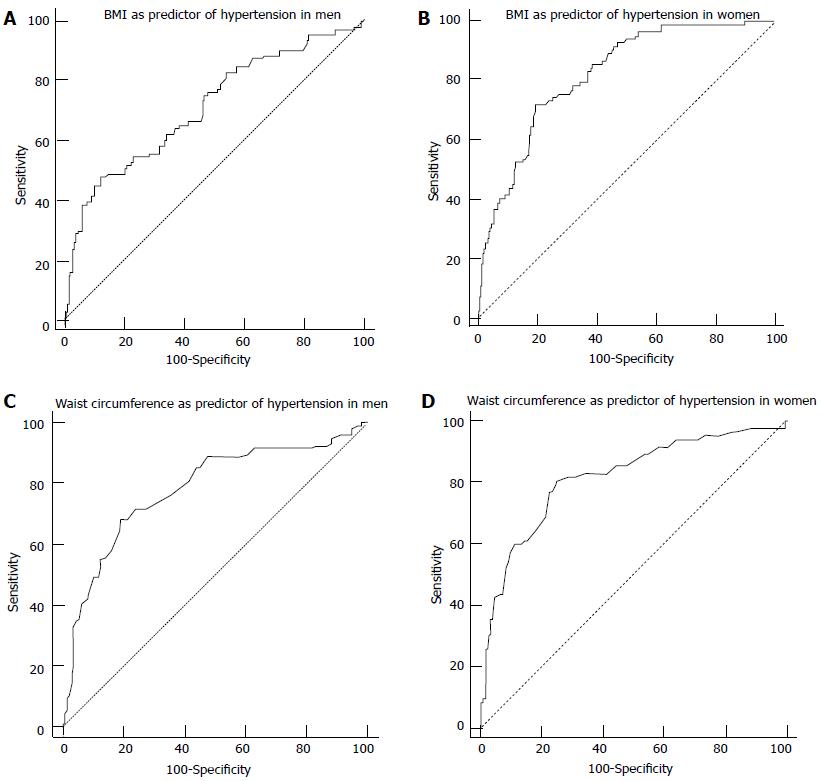
RESULTS: The ROC analysis revealed that BMI is a good predictor of hypertension for both men (area under the ROC curve 0.714) and women (area under the ROC curve 0.821). The cut-off values of BMI for predicting hypertension were identified as ≥ 24.5 kg/m2 in men and ≥ 24.9 kg/m2 in women. Similarly, the ROC analysis for waist circumference showed that it is a good predictor of hypertension both for men (area under the ROC curve 0.784) and women (area under the ROC curve 0.815). The cut-offs for waist circumference for predicting hypertension were estimated as ≥ 83 cm for men and ≥ 78 cm for women. Adults with high BMI or high waist circumference had a higher prevalence of hypertension, respectively.
CONCLUSION: Simple anthropometric measurements such as BMI and waist circumference can be used for screening people at increased risk of hypertension in order to refer them for more careful and early diagnostic evaluation. Policies and programs are required for primary and secondary prevention of hypertension.
Core tip: The Receiver operating characteristic analysis for body mass index (BMI) and waist circumference, respectively, showed good discriminatory power for hypertension in both men and women. The cut-off for BMI was identified as ≥ 24.5 kg/m2 in men and ≥ 24.9 kg/m2 in women. The cut-off for waist circumference for screening of hypertension was estimated as ≥ 83 cm in men and ≥ 78 cm in women. BMI and waist circumference, being simple tools in identifying hypertension, can be used for primordial and primary prevention and can thereby bring about a substantial reduction in cardiovascular morbidity and mortality which occurs as a consequence of hypertension.
- Citation: Midha T, Krishna V, Nath B, Kumari R, Rao YK, Pandey U, Kaur S. Cut-off of body mass index and waist circumference to predict hypertension in Indian adults. World J Clin Cases 2014; 2(7): 272-278
- URL: https://www.wjgnet.com/2307-8960/full/v2/i7/272.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i7.272
According to World Health Organization (WHO), cardiovascular diseases (CVDs) are the number one cause of death globally: more people die annually from CVDs than from any other cause[1]. An estimated 17.3 million people died from CVDs in 2008, representing 30% of all global deaths. The prevalence of hypertension in adults aged 25 years and above, worldwide, was around 40% in 2008[1]. Globally, raised blood pressure is estimated to cause 7.5 million deaths, about 12.8% of the total mortality. This, accounts for 57 million disability adjusted life years (DALYS) or 3.7% of total DALYS[1]. WHO has estimated that hypertension is directly responsible for about 62% of CVDs and 49% of ischemic heart disease (IHD) worldwide[2].
A meta-analysis of prevalence studies on hypertension in India, from January 2000 to June 2012, revealed a high prevalence of hypertension in the urban (40.8%) as well as rural population (17.9%)[3]. India accounts for 17% of the world’s population, second largest in the world, thereby contributing largely to the statistics of any disease in the world[4].
Hypertension is a controllable disease and it has been reported that targeted reductions in blood pressure in hypertensives as well as modest population-wide blood pressure reductions are expected to produce large reductions in the burden of cardiovascular disease[5]. Miall suggested that genetic influences contribute not more than a third to the variance in blood pressure levels[6]. If the remaining two-thirds are environmental in origin, then an understanding of these environmental factors and appropriate preventive measures could help to bring down the burden of hypertension in the world. According to the Seventh Report of the Joint National Committee (JNC-7) on prevention, detection, evaluation, and treatment of high blood pressure, modification of risk factors plays an important role in the prevention and control of high blood pressure[7].
Recent studies show that for every known person with hypertension there are two persons with either undiagnosed hypertension or prehypertension[8]. Screening the population for hypertension can go a long way in identifying individuals with undiagnosed hypertension and prevent a significant proportion of cardiovascular morbidity and mortality due to inapparent hypertension.
Being overweight in adulthood is well known to increase the risk of CVD especially hypertension[9]. It has also been seen that having a body mass index (BMI) outside the normal range significantly worsens risk parameters for CVD in school aged children[10]. Recognizing obesity using BMI and waist circumference as a marker, and thereby screening for cardiovascular risk can be a simple and inexpensive method of combating CVDs at the primary health care level. Given the magnitude of the problem of hypertension in India and its grave cardiovascular consequences, accurate estimates of cut-offs of BMI and waist circumference in predicting hypertension in the Indian population are necessary to plan effective control measures.
The study population consisted of the total population of Kanpur district aged more than 20 years.
This was a population based cross-sectional study. The sample size required (N = 372) was calculated taking a prevalence of obesity of 6.2%, as reported in the “Five City study” from Moradabad, with a precision of 2.5% and a confidence level of 95%[11]. The formula used was, n = Z(1-α/2 )2pq/d2 (where Z(1-α/2) was taken at 95% confidence; p = prevalence of obesity, q = 100-p; d = absolute precision). For this study, p = 6.2%; q = 93.8%; d = 2.5%. Adding a 10% for incomplete answers, the total number came out to be 409. Since it was a multistage stratified random sampling, a design effect of 2 was included to minimize any error due to inherent variation in the population. The calculated sample size was multiplied by 2 to obtain the sample size of 818. The data was analyzed for 801 subjects only who had provided complete answers.
Urban Kanpur has 110 wards and a total population of 2797511 according to 2001 census, and rural Kanpur has 10 blocks and a population of 1370488 which implies a ratio of 2:1 respectively[12]. Therefore, applying Probability Proportional to Size (PPS), out of 818 subjects, two-thirds (545) were selected from the urban population and one- third (273) were selected from the rural population. Multistage stratified random sampling technique was used to select representative subjects of Kanpur district. At the first stage, 8 wards were randomly selected to study the urban population[13]. Similarly, to study the rural population, 4 blocks were randomly selected[14]. At the second stage, 1 urban locality from each ward was randomly selected. Similarly, 1 village from each block was randomly selected. A total of 68 subjects from each urban locality/village were interviewed to complete the required sample size.
The households in every urban area/village were selected for the study by systematic sampling. Depending upon the population of the particular urban locality/village, a random number was chosen and every nth household was selected for the study. This process was continued till the required sample size was completed. In every household, only one member, aged more than 20 years was randomly selected. Out of the 545 respondents interviewed in the urban area, 10 were excluded owing to incomplete answers, whereas of the 273 respondents interviewed in the rural area 7 were excluded. Therefore, the final analysis included the responses from a total of 801 study subjects. Data collection was done from December 2006 to February 2007.
A pre-tested structured questionnaire was used to elicit the required information from the study participants. A standard mercury sphygmomanometer was used for recording blood pressure. Before the measurement was taken, the patient was seated comfortably for at least 5 min. Care was taken that the arm muscles were relaxed and the arm was supported at heart level. The cuff was applied to the right upper arm and was inflated until the manometer reading was 30 mm Hg above the level at which the radial pulse disappears, and then slowly deflated at a rate of approximately 2 mmHg/s. During this time, the Korotkoff sounds were monitored using a stethoscope placed over the brachial artery. The first (appearance) and the fifth (disappearance) Korotkoff sounds were recorded as the systolic and diastolic blood pressure, respectively. Blood pressures were measured twice and their mean was recorded. According to JNC-7[15], normal blood pressure was defined as a systolic blood pressure (SBP) < 120 mmHg and a diastolic blood pressure (DBP) < 80 mmHg; pre-hypertension as SBP 120-139 mmHg and/or DBP 80-89 mmHg; Stage I hypertension as SBP 140-159 mmHg and/or DBP 90-99 mmHg and stage II hypertension as ≥ 160 mmHg and/or DBP ≥ 100 mmHg. In the present study, subjects in stage I and Stage II were considered as hypertensive. Waist circumference was measured to the nearest 0.1 cm using a non-extensible tape. Measurement was made at the level of the umbilicus, with the subject in the erect position, breathing silently.
Data was compiled in Microsoft Excel and analysed using MedCalc12.7.5 software. Receiver operating characteristic (ROC) analysis was used to compare the predictive validity, and to determine the optimal cut-off values of anthropometric indices. Area under the curve was also measured to determine the diagnostic power of the test, and to describe the probability that the anthropometric indices would correctly identify subjects with hypertension. Optimal cut-off values were measured by calculating the sensitivity and specificity of the anthropometric measurements at various cut-off points. Youden index was calculated to find out the associated criterion with maximum sensitivity and specificity for predicting hypertension.
In the present study, the mean age of the study subjects was 35.5 ± 12.6 years, while that of men and women respectively was 36.4 ± 13.8 years and 34.8 ± 11.6 years (Table 1). Average BMI of the study population was 21.9 ± 4.3 kg/m2. The mean waist circumference of men was 78.9 ± 11.0 cm and that of women was 74.4 ± 11.1 cm. Average systolic and diastolic blood pressure of the study population was 124 ± 17 mmHg and 80 ± 9 mmHg respectively. The mean systolic blood pressure among men was 127 ± 16 mmHg and that among women was 122 ± 18 mmHg. The mean diastolic blood pressure among men and women was 82 ± 9 mmHg and 78 ± 10 mmHg respectively.
| Parameters | Men(n =356) | Women(n =445) | Total(n = 801) |
| Age (yr) | 36.4 ± 13.8 | 34.8 ± 11.6 | 35.5 ± 12.6 |
| Weight (kg) | 58.6 ± 11.5 | 51.7 ± 11.7 | 54.8 ± 12.1 |
| Height (cm) | 165.3 ± 7.1 | 151.7 ± 5.9 | 157.7 ± 9.3 |
| BMI (kg/m2) | 21.4 ± 3.9 | 22.4 ± 4.6 | 21.9 ± 4.3 |
| Waist circumference (cm) | 78.9 ± 11.0 | 74.4 ± 11.1 | 76.5 ± 11.3 |
| SBP (mmHg) | 127 ± 16 | 122 ± 18 | 124 ± 17 |
| DBP (mmHg) | 82 ± 9 | 78 ± 10 | 80 ± 9 |
The ROC analysis for BMI showed good discriminatory power for hypertension for both men and women. Area under the ROC curve was 0.714 for men and 0.821 for women respectively (Figure 1 A and B). The cut-off for BMI with better properties for screening of hypertension was identified as ≥ 24.5 kg/m2 in men and ≥ 24.9 kg/m2 in women (Table 2). The sensitivity and specificity of cut-off for BMI in men was 48.1% and 87.2% respectively, and that for women was 71.9% and 80.7% respectively.
| Indicators | BMI in men | BMI in women | WC in men | WC in women |
| Area under the ROC curve | 0.714 | 0.821 | 0.784 | 0.815 |
| Standard error | 0.0312 | 0.0237 | 0.0286 | 0.0284 |
| 95%CI | 0.664 to 0.760 | 0.783 to 0.856 | 0.737 to 0.826 | 0.776 to 0.850 |
| z statistic | 6.857 | 13.572 | 9.922 | 11.117 |
| Significance level P (Area = 0.5) | < 0.0001 | < 0.0001 | < 0.0001 | < 0.0001 |
| Youden index J | 0.3611 | 0.5294 | 0.4912 | 0.5542 |
| Associated criterion | > 24.5 | > 24.9 | > 83 | > 78 |
Similarly, the ROC analysis for waist circumference revealed that it is a predictor of hypertension for both men and women. Area under the ROC curve was 0.784 for men and 0.815 for women respectively (Figure 1C and D). The cut-offs for waist circumference for screening of hypertension was estimated as ≥ 83 cm for men and ≥ 78 cm for women (Table 2). The sensitivity and specificity of cut-off of waist circumference in men was 67.9% and 80.4% respectively while that for women was 81.7% and 71.3% respectively. Adults with high BMI or high waist circumference had a higher prevalence of hypertension, respectively.
ROC analysis was also done after combining the prehypertensive and hypertensive subjects as non-normotensive and the remaining normal subjects as normotensive. It was observed that BMI was not a good predictor of non-normotensive status both in men and women. Area under the curve was 0.452 for BMI among men and 0.540 among women respectively. Similarly it was found that waist circumference did have good discriminatory power for non-normotensive status both in men and women. Area under the curve was 0.429 among men and 0.552 among women respectively. These results were not statistically significant.
Therefore, BMI and waist circumference can be considered good predictors of hypertension but not of pre-hypertension.
In the present study, cut-off for BMI for predicting hypertension was identified as ≥ 24.5 kg/m2 in men and ≥ 24.9 kg/m2 in women. In a study from Malaysia, the mean age of the study subjects was 44 ± 14 years and the cut-off for BMI as predictor of hypertension was 25.5 kg/m2 in men and 24.9 kg/m2 in women, which was very similar to our study. Areas under the curves of BMI as a predictor of hypertension were 0.59 and 0.61 in men and women, respectively[16]. Area under the curves of 0.6-0.7 are considered to be poor while 0.7-0.8 are considered fair, as seen in our study. Increased CVD risks related to obesity at lower BMIs have been found in Asians[17,18]. In addition, Asians are also predisposed to visceral or abdominal obesity[19]. Therefore, WHO recently proposed lower BMI values to define overweight and obesity in people of the Asia-Pacific region[20]. According to the World Heart Federation, if a person’s BMI is more than 30, he/she is obese and at serious risk of cardiovascular disease, whereas in our study, optimal cut-off for BMI for predicting hypertension was identified as ≥ 24.5 kg/m2 in men and ≥ 24.9 kg/m2 in women[21].
However, some studies have also revealed that BMI follows a J-shaped curve to predict all case mortality. BMI is a strong predictor of overall mortality both above and below the apparent optimum of about 22.5-25 kg/m²[22]. The progressive excess mortality above this range is mainly due to vascular diseases and is probably causal at large. At 30-35 kg/m², median survival is reduced by 2-4 years; at 40-45 kg/m², it is reduced by 8-10 years (which is comparable with the effects of smoking). The definite excess mortality below 22.5 kg/m² is mainly due to smoking-related diseases, and is not fully explained.
In the present study, the optimal cut-offs of waist circumference for screening of hypertension was estimated as ≥ 83 cm for men and ≥ 78 cm for women. The waist circumference cut-offs for risk of hypertension obtained in this study are comparable to those reported by Snehalatha et al[23] for South Indians, which was reported as 85 cm for men and 80 cm for women wherein the mean age of the study population was 40.4 ± 14.2 years. These were also similar to the cut-offs observed by Rao et al[24] in Maharashtra as 86 cm in the male population averaging 42.9 ± 7.9 years and 79 cm in the female population averaging 42.2 ± 7.8 years[23,24]. The cut-offs in the present study were slightly lower for men when compared to those reported by Misra et al[25] for North Indians (90 cm for men averaging 40.5 ± 14.7 years) and slightly higher for women (80 cm for women having mean age of 38.8 ± 14.8 years). In other Asian populations, cut-offs reported by Wildman et al[26] for Chinese adults (86 cm for both sexes) and those observed by Lin et al[27] for adults from Taiwan as 80.5 cm for men and 71.5 cm for women with mean age 37.3 ± 10.9 years in men and 37.0 ± 11.1 years in women, were on the lower side. Ethnicity plays an important role in determining the predictive power of waist circumference for hypertension. Also, nutrition habits vary among different populations which may be the reason for the difference in waist circumference cut-offs.
According to the World Heart Federation, if the waist circumference is more than 102 cm among men, the person is at serious risk of CVDs, but for Asian men the cut-off has been set at 90 cm[21]. Similarly for women the high risk cut-off is 88 cm whereas in Asian women, it is 80 cm. In our study, the optimal cut-offs for waist circumference for predicting hypertension were ≥ 83 cm for men and ≥ 78 cm for women, which approximate the Asian cut-offs. In Asians, more than in the Western population, there is a strong association between blood pressure and stroke. It has been estimated that reduction of 3 mmHg in DBP would reduce the number of strokes in Asia by one third. Identification of indicators predicting risk of hypertension therefore has an important implication towards prevention of morbidity and mortality due to CVDs[28].
A major limitation of the study was that the classification of hypertension was based on a single measurement of blood pressure. Secondly, the number of female study subjects was greater than males which might act as a source of bias in studying the difference in the cut-offs for predicting hypertension in men and women, respectively. Although this is not a meta-analysis, it is a useful study with practical application for the prevention and control of hypertension.
The present study reveals that BMI and waist circumference are simple tools in identifying hypertension. Although it is not easy to determine how low the cut-off should be, the findings in this study provide sufficient evidence that BMI and waist circumference can be used as a screening tool for hypertension. Since high blood pressure itself is the entry point to other non-communicable diseases, this emphasizes the need for further research to identify cut-offs of simple anthropometric measurements, which can be calculated by people themselves, for screening of hypertension. Given the risk of CVD associated with high blood pressure, hypertension screening and health education programs regarding weight reduction may be considered as a cost-effective public health approach in dealing with the morbidity attributed to CVDs. This study is only a prelude to the upcoming research in the field of non-communicable diseases especially in the Asian population which is more vulnerable to adverse effects of obesity.
Cardiovascular diseases (CVDs) are the most common cause of mortality in the world; around 30% of all global deaths in 2008 were attributed CVDs. High blood pressure is the entry point to CVDs and other non-communicable diseases. The magnitude of hypertension in adults aged 25 and over was around 40% in the world in 2008. A meta-analysis in 2013 estimated the prevalence of hypertension as 40.8% in the urban and 17.9% in the rural Indian population. Body mass index (BMI) and waist circumference are simple tools in predicting hypertension, which can be calculated by the people themselves. The findings in this study provide cut-off levels of BMI and waist circumference for screening of hypertension in the Indian population. Given the risk of CVDs associated with high blood pressure, hypertension screening and health education programs regarding weight reduction may be considered as a cost-effective public health approach in dealing with the morbidity attributed to CVDs. Therefore, a precise estimate of the cut-offs of BMI and waist circumference specific to the indigenous population of the country is required to assess the magnitude of the problem that has to be addressed and to design programs and policies for prevention and control.
In India, very few studies are available on the cut-offs of BMI and waist circumference for predicting hypertension. Given the variation in anthropometry due to ethnic differences and discrepancies in the nutritional status of different populations, an estimate of the cut-offs for screening of hypertension in the Indian population is required which can help in the development of preventive strategies.
BMI and waist circumference have good discriminatory power for predicting hypertension in the Indian population and this knowledge will help in shaping primordial and primary level preventive programs for the country.
Very few studies on cut-off levels of BMI and waist circumference for screening of hypertension are available in India; therefore, the main application of this study is to provide cut-offs levels for our indigenous population to help develop a strategy for control and prevention of hypertension appropriate for the country.
The ROC curve is a fundamental tool for diagnostic test evaluation using a graphical plot. In a ROC curve the true positive rate (Sensitivity) is plotted as a function of the false positive rate (100-Specificity) for different cut-off points of a parameter. Each point on the ROC curve represents a sensitivity/specificity pair corresponding to a particular decision threshold. The ROC curve estimates and reports all of the combinations of sensitivity and specificity that a diagnostic test is able to provide.The area under the ROC curve (AUC) is a measure of how well a parameter can distinguish between two diagnostic groups (diseased/normal). Accuracy of a diagnostic test is measured by the area under the ROC curve. An area of 1 represents a perfect test; an area of 0.5 represents a worthless test. The associated criterion value corresponding with the Youden index J is the optimal criterion value when disease prevalence is 50% and equal weight is given to sensitivity and specificity.
The study titled “Optimal Cut-off values of BMI and waist circumference to predict hypertension in adults: A cross-sectional study in a north Indian population” has been well thought out. It may be an incremental contribution of the manuscript to the field. Design of the manuscript is also good. It is well-marked that this paper would have a few literature errors formally.
P- Reviewers: Puddu PE, Talas ZS, Undela K, Xu XH S- Editor: Wen LL L- Editor: A E- Editor: Wu HL
| 1. | World Health Organization. Global Health Repository. Available from: http://www.who.int/gho/ncd/risk_factors/blood_pressure_prevalence_text/en/index.html. |
| 2. | World Health Report. Reducing Risks, Promoting Healthy Life (2002; Chapter 4; p-12). Available from: http://www.who.int/whr/2002/en/whr02_ch4.pdf.. |
| 3. | Midha T, Nath B, Kumari R, Rao YK, Pandey U. Prevalence of hypertension in India: A meta-analysis. World J Meta-Anal. 2013;1:83-89. [RCA] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (4)] |
| 4. | World Development Report 2006. Equity and Development. Washington D. C: A co-publication of the World Bank and Oxford University Press 2006; . |
| 5. | Rodgers A, Lawes C, MacMahon S. Reducing the global burden of blood pressure-related cardiovascular disease. J Hypertens Suppl. 2000;18:S3-S6. [PubMed] |
| 6. | Miall WE. Heredity and hypertension. Practitioner. 1971;207:20-27. [PubMed] |
| 7. | Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA. 2003;289:2560-2572. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13416] [Cited by in RCA: 13292] [Article Influence: 604.2] [Reference Citation Analysis (0)] |
| 8. | Joshi SR, Saboo B, Vadivale M, Dani SI, Mithal A, Kaul U, Badgandi M, Iyengar SS, Viswanathan V, Sivakadaksham N. Prevalence of diagnosed and undiagnosed diabetes and hypertension in India--results from the Screening India’s Twin Epidemic (SITE) study. Diabetes Technol Ther. 2012;14:8-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 81] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 9. | McPherson K, Marsh T, Brown M. Tackling obesities: future choices-modelling future trends in obesity and the impact on health: report for Foresight (Government Office for Science, 2007). Available from: http://www.gov.uk/government/uploads/system/uploads/attachment_data/file/287937/07-1184x-tackling-obesities-future-choices-report.pdf(last accessed 3-7-14). |
| 10. | Friedemann C, Heneghan C, Mahtani K, Thompson M, Perera R, Ward AM. Cardiovascular disease risk in healthy children and its association with body mass index: systematic review and meta-analysis. BMJ. 2012;345:e4759. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 457] [Cited by in RCA: 430] [Article Influence: 33.1] [Reference Citation Analysis (0)] |
| 11. | Singh RB, Pella D, Mechirova V, Kartikey K, Demeester F, Tomar RS, Beegom R, Mehta AS, Gupta SB, De Amit K. Prevalence of obesity, physical inactivity and undernutrition, a triple burden of diseases during transition in a developing economy. The Five City Study Group. Acta Cardiol. 2007;62:119-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 50] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 12. | Government of India. Census of India 2001, Population Totals, Paper - 1; 2001. Available from: http://www.censusindia.gov.in/pca/SearchDetails.aspx?Id=163690 (last accessed 3-7-14). |
| 13. | Nagar Nigam: Kanpur District, 2002: 3. . |
| 14. | Kanpur District: Office of Chief Development Office, 2002: 10. . |
| 15. | Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8787] [Cited by in RCA: 8989] [Article Influence: 408.6] [Reference Citation Analysis (0)] |
| 16. | Zaher ZM, Zambari R, Pheng CS, Muruga V, Ng B, Appannah G, Onn LT. Optimal cut-off levels to define obesity: body mass index and waist circumference, and their relationship to cardiovascular disease, dyslipidaemia, hypertension and diabetes in Malaysia. Asia Pac J Clin Nutr. 2009;18:209-216. [PubMed] |
| 17. | Deurenberg-Yap M, Yian TB, Kai CS, Deurenberg P, VAN Staveren WA. Manifestation of cardiovascular risk factors at low levels of body mass index and waist-to-hip ratio in Singaporean Chinese. Asia Pac J Clin Nutr. 1999;8:177-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 67] [Cited by in RCA: 75] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 18. | Hsieh SD, Yoshinaga H, Muto T, Sakurai Y, Kosaka K. Health risks among Japanese men with moderate body mass index. Int J Obes Relat Metab Disord. 2000;24:358-362. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 73] [Cited by in RCA: 69] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 19. | Wang J, Russell-Aulet M, Mazariegos M, Burastero S, Thornton J, Lichtman S, Heymsfield SB, Pierson Jr NP. Body fat by dual photon absorptiometry (DPA): comparisons with traditional methods in Asians, Blacks and Caucasians. Am J Hum Biol. 1992;4:501–510. [RCA] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 20. | World Health Organization. The Asia-Pacific perspective: redefining obesity and its treatment (WHO: Geneva, 2000). Available from: http://www.wpro.who.int/nutrition/documents/Redefining_obesity/en/ (last accessed 3-7-14). |
| 21. | Available from: http://www.world-heart-federation.org/cardiovascular-health/cardiovascular-disease-risk-factors/obesity/. |
| 22. | Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, Halsey J, Qizilbash N, Collins R, Peto R. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083-1096. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3582] [Cited by in RCA: 3261] [Article Influence: 203.8] [Reference Citation Analysis (0)] |
| 23. | Snehalatha C, Viswanathan V, Ramachandran A. Cutoff values for normal anthropometric variables in asian Indian adults. Diabetes Care. 2003;26:1380-1384. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 273] [Cited by in RCA: 290] [Article Influence: 13.2] [Reference Citation Analysis (0)] |
| 24. | Rao S, Waingankar PP. Performance of waist circumference relative to BMI in predicting risk of obesity and hypertension among affluent Indian adults. Health. 2013;5:16-22. [RCA] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 25. | Misra A, Vikram NK, Gupta R, Pandey RM, Wasir JS, Gupta VP. Waist circumference cutoff points and action levels for Asian Indians for identification of abdominal obesity. Int J Obes (Lond). 2006;30:106-111. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 172] [Cited by in RCA: 194] [Article Influence: 10.2] [Reference Citation Analysis (0)] |
| 26. | Wildman RP, Gu D, Reynolds K, Duan X, He J. Appropriate body mass index and waist circumference cutoffs for categorization of overweight and central adiposity among Chinese adults. Am J Clin Nutr. 2004;80:1129-1136. [PubMed] |
| 27. | Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, Lin RS, Shau WY, Huang KC. Optimal cut-off values for obesity: using simple anthropometric indices to predict cardiovascular risk factors in Taiwan. Int J Obes Relat Metab Disord. 2002;26:1232-1238. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 243] [Cited by in RCA: 244] [Article Influence: 10.6] [Reference Citation Analysis (0)] |
| 28. | Cheung YB, Low L, Osmond C, Barker D, Karlberg J. Fetal growth and early postnatal growth are related to blood pressure in adults. Hypertension. 2000;36:795-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 58] [Article Influence: 2.3] [Reference Citation Analysis (0)] |