Published online Jun 16, 2014. doi: 10.12998/wjcc.v2.i6.209
Revised: January 27, 2014
Accepted: May 8, 2014
Published online: June 16, 2014
Processing time: 187 Days and 23.9 Hours
Jejunal diverticula are rare and subsequent complications even more so. The usual small bowel diverticulum encountered by general surgeons is a Meckel’s. These are embryological remnants of the vitello-intestinal duct and are on the anti-mesenteric surface of the terminal ileum. They may contain heterotopic gastric or pancreatic mucosa. Herein we explore the case of a young girl who presented with features of peritonitis secondary to a complication from a jejunal diverticulum. The case, pathology, complications and treatment of jejunal diverticulosis and heterotopic gastric mucosa in the jejunum are explored.
Core tip: Herein we describe a rare but important cause of peritonitis in children. We feel it will be of interest to surgeons and pathologists alike and is an important reminder of the basic anatomy and pathology of surgical disease.
- Citation: Bunni J, Barrett HL, Cook TA. Perforated jejunal ulcer associated with gastric mucosa in a jejunal diverticulum. World J Clin Cases 2014; 2(6): 209-210
- URL: https://www.wjgnet.com/2307-8960/full/v2/i6/209.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i6.209
Jejunal diverticula are rare and subsequent complications even more so[1]. The usual small bowel diverticulum encountered by general surgeons is a Meckel’s. These are embryological remnants of the vitello-intestinal duct and are on the anti-mesenteric surface of the terminal ileum. They may contain heterotopic gastric or pancreatic mucosa.
Complications of true jejunal diverticula are rare particularly in young children. Herein we explore the case of a young girl who presented with features of peritonitis secondary to a complication from a jejunal diverticulum. Following surgery she made an excellent recovery. We explore the case, pathology, complications and treatment of jejunal diverticulosis and heterotopic gastric mucosa in the jejunum.
A previously fit and well 5 years old girl presented to the pediatricians with a two day history of worsening abdominal pain, anorexia and vomiting.
Clinical findings were of pyrexia and generalised peritonitis. Bloods tests showed a lymphocytosis of 29.2 × 109/L.
A working differential diagnosis was of acute perforated appendicitis or perforated Meckel’s diverticulum and she was taken immediately to the operating theatre.
A 1 cm proximal jejunal perforation was identified on the antimesenteric border, directly opposite a mesenteric diverticulum, with a normal appendix. Small bowel resection was performed with peritoneal toilet. She made a steady recovery and was discharged home on day four post-operatively.
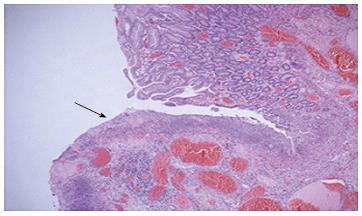
Histology of the small bowel showed features of a true diverticulum with gastric mucosa lining the diverticulum. Helicobacter-like organisms were not identified. The adjacent small bowel showed transmural inflammation and degeneration of the wall at the site of perforation with an adjacent serosal exudate (Figure 1). There was no evidence of malignancy. Sections of the appendix showed a mild serosal exudate but no evidence of mucosal acute inflammation.
Jejunal diverticula, like all diverticula can be true, involving all three layers of the bowel wall or false - a herniation of mucosa and submucosa through the muscularis propria. True diverticula are usually congenital and false are acquired. The latter are more common and are pulsion diverticula which arise at the weak point on the jejunal mesenteric surface (the point where the mural vessels penetrate the bowel wall). They are more common in middle aged males.
Rarer are the true diverticula which are congenital in nature. These can be on either the mesenteric or antimesenteric surface. The mesenteric diverticula are thought to be primarily related to the neurenteric remnants and duplications, and can be lined by gastric; intestinal or respiratory type epithelium or contain heterotopic pancreatic tissue.
Complications from jejunal diverticula are varied. Though the majority are silent, they can present with chronic abdominal pain, malabsorption, acute gastrointestinal haemorrhage, occult bleeding, diverticulitis, perforation, bacterial overgrowth or small bowel obstruction due to jejunal volvulus. Complications warranting surgical intervention occur in 8% to 30% of patients[2].
In the elective setting, if suspicious of jejunal diverticulosis there are different investigations that can be performed. These include small bowel follow through, small bowel enteroclysis, capsule endoscopy, computed tomography scanning as well as in the case of bleeding, radionuclide scans and mesenteric angiography.
Jejunal heterotopic gastric mucosa is a very rare entity, and literature review revealed the usual presenting age to be 14 years[3]. A common presentation is that of intermittent intussusception secondary to a small bowel (usually) polypoidal mass. This mass is predominantly located only a few centimetres distal to ligament of Treitz.
Management of jejunal diverticula depends on whether or not patients experience symptoms. Asymptomatic jejunal diverticula found incidentally rarely warrant treatment. In symptomatic cases small bowel resection and end-to-end anastomosis is advised.
Jejunal diverticula are rare and their complications even more so. There are subtle pathological differences and once responsible for complications the authors advise small bowel resection and end-to-end anastomosis so as to achieve a pathological diagnosis; cure the problem and ensure no remaining potential heterotopic mucosa of other organs remains.
This young patient presented with an acute abdomen and shock.
Diagnose with peritonitis. Lab tests showed a lymphocytosis.
Acute appendicitis or perforated Meckel’s diverticulum.
She was taken to the operating room whereby a small bowel perforation was identified and resected.
Histopathological analysis revealed this to be a perforation secondary to heterotopic gastric mucosa.
Small bowel resection was performed with peritoneal toilet and making a steady recovery.
To rapidly identify the sick patient and not waste time on investigations that will not alter management. Awareness of the diversity of small bowel pathology.
This is a short case report showing a pediatric patient with perforating jejunal diverticulum. The case is rare and may be worth publication.
P- Reviewers: Kim BW, Kato J S- Editor: Ma YJ L- Editor: A E- Editor: Wu HL
| 1. | Zager JS, Garbus JE, Shaw JP, Cohen MG, Garber SM. Jejunal diverticulosis: a rare entity with multiple presentations, a series of cases. Dig Surg. 2000;17:643-645. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 34] [Cited by in RCA: 30] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Wilcox RD, Shatney CH. Surgical significance of acquired ileal diverticulosis. Am Surg. 1990;56:222-225. [PubMed] |
| 3. | Boybeyi O, Karnak I, Güçer S, Orhan D, Senocak ME. Common characteristics of jejunal heterotopic gastric tissue in children: a case report with review of the literature. J Pediatr Surg. 2008;43:e19-e22. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |