Published online Apr 16, 2014. doi: 10.12998/wjcc.v2.i4.97
Revised: January 14, 2014
Accepted: February 20, 2014
Published online: April 16, 2014
Processing time: 178 Days and 11.7 Hours
We report a case of a 54-year-old patient who was denied surgical replacement for severe aortic stenosis because of complicated acquired immunodeficiency syndrome and who successfully underwent transcatheter aortic valve implantation at our institution.
Core tip: The present case report describes the feasibility and safety of transcatheter aortic valve implantation for patients with acquired immunodeficiency syndrome, evaluated after the heart team decision.
- Citation: Salizzoni S, D’Ascenzo F, Moretti C, Bonora S, Calcagno A, Omedè P, Montrucchio C, Cerrato E, Colaci C, Sheiban I, Marra S, Rinaldi M, Gaita F. Transcatheter aortic valve implantation in a 54-year-old patient with aggressive HIV. World J Clin Cases 2014; 2(4): 97-99
- URL: https://www.wjgnet.com/2307-8960/full/v2/i4/97.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i4.97
The transcatheter aortic valve implantation (TAVI) procedure is currently considered a valid alternative to surgery in patients with severe aortic stenosis not eligible for valve replacement or with high operative risk, as demonstrated by the recent PARTNER[1] trial, which showed similar results between surgery and TAVI. For this reason, it may represent an attractive option for patients whose surgical risk is difficult to assess, like immunocompromised ones.
We report the case of a 54-year-old male (82 kg, 178 cm) with a diagnosis of post-transfusion HIV infection in 1990, who had taken six different antiretroviral drugs because of a virus with several resistances. In October 2009, the patient was hospitalized for Listeria meningitis and he suffered from several episodes of acute heart failure, after which severe aortic stenosis was diagnosed by transthoracic echocardiography (TTE), with a mean gradient of 55 mmHg and an ejection fraction of 50% without coronary disease at the angiography. The patient was consequently referred to cardiac surgeons who refused to do the procedure due to a high operative risk, with a Cd4 cell count of 400 cell/cc and low count of platelets. Nevertheless, from December 2010 he became symptomatic (NYHA III) and had several syncopal episodes, the last of which led to a leg fracture.
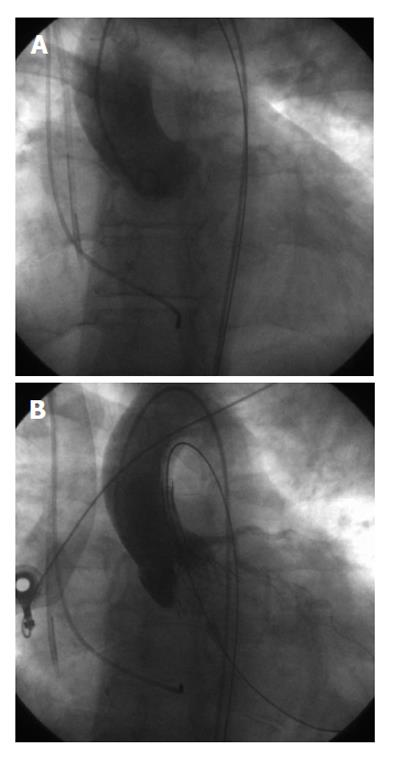
The patient was referred again to our surgeons who considered him for TAVI, despite his age and low risk detected by common scores (Logistic EuroSCORE 1.51%, STS 3%). Multidisciplinary discussion, including the infectious diseases specialist who foresaw at least a 2-year survival and a high risk of potential life threatening peri-intervention infections at the same time, led to the decision of a percutaneous transfemoral approach to minimize all potential sites of infection, both for the patient and the operators. He was successfully treated with a 29 mm CoreValve and discharged uneventfully on post-operative day nine (Figure 1). His TTE showed a mean gradient of 12 mmHg and mild paraprothesic aortic insufficiency. His cardiovascular therapy consisted of aspirin, clopidogrel and furosemide 25 mg.
Two weeks after discharge, he presented to the emergency department because of angina (CCS II) and repeated episodes of gingival bleeding and melena. ECG was unchanged but important anemia (Hb 8 g/dL) was detected, so clopidogrel was stopped.
At the 12 mo follow-up, he was in NYHA I and had no further syncope or angina. Ejection fraction was 51%, with a mean transprothesic gradient of 12 mmHg and still mild paraprothesic aortic insufficiency on echocardiography.
The numbers of immunocompromised patients with aortic stenosis will increase because of longer survival for HIV patients[2-4].
Despite some encouraging reports from patients with uncomplicated HIV[5], their management can be really tricky: for patients, because of a high infective risk, high prevalence of renal disease and consequently a risk of bleeding or thrombosis[4-6], and for surgeons, due to contamination risk[7]. Moreover, accurate tools to correctly assess risk in immunocompromised patients (not appraised by EuroSCORE and only partially by the STS score[8,9]) are lacking and no data are reported about in hospital and midterm follow up complications. This medical issue will become more and more relevant due to the increase in survival of patients with immunodeficiency (both HIV or after transplant). It must be remembered that in some countries, such as the United States, the TAVI procedure is still considered to be in an initial phase and this can affect the lack of data regarding this population. To the best of our knowledge, this is the first HIV patient with severe aortic stenosis treated by TAVI, which was chosen mainly due to the infective risk. TAVI, with an accurate treatment of in-hospital complications, may represent a feasible choice for those with HIV/AIDS.
Aggressive acquired immunodeficiency syndrome (AIDS) in a patient referred for invasive cardiac surgery to improve his life expectancy.
NYHA III: reduced second heart sound with systolic murmur heard. Electrocardiogram (ECG) with left ventricle hypertrophy and echocardiogram confirming severe stenosis.
After syncope, ECG monitoring did not show any atrioventricular block.
The lymphocyte typing detected a significant reduction in the lymphocyte subpopulation of CD3+, CD4+ and CD19+.
Transthoracic echocardiography showed the left ventricle with concentric hypertrophy and FE of 55%; severe aortic stenosis with AVA 0.8 cm² and mean transvalvular gradient of 55 mmHg without coronary disease at angiography.
HIV-positive patient treated with anti-retroviral therapy, suffering from symptomatic severe aortic stenosis.
Transfemoral transcatheter aortic valve implantation (TAVI).
Core Valve is a valve prosthesis, comprised of 3 porcine pericardial tissue leaflets mounted in a self-expanding nitinol frame. This valve has only been used in a retrograde approach, either via transfemoral, subclavian or direct aortic access.
TAVI can be considered a therapeutic option for severe aortic stenosis in a severe immunosuppressed status, as for patients with AIDS treated with antiretroviral therapy.
The argument could be considered a strong point because in the literature, this is not treated; in fact, this was the first TAVI procedure on a patient affected by AIDS at high risk for valve surgical replacement. So, this case report represents an example for an alternative therapeutic option, giving an opportunity for these patients to be cured despite their important comorbidity.
P- Reviewers: Kasai Y, Muluk NB, Simmons RG S- Editor: Ma YJ L- Editor: Roemmele A E- Editor: Liu SQ
| 1. | Smith CR, Leon MB, Mack MJ, Miller DC, Moses JW, Svensson LG, Tuzcu EM, Webb JG, Fontana GP, Makkar RR. Transcatheter versus surgical aortic-valve replacement in high-risk patients. N Engl J Med. 2011;364:2187-2198. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4547] [Cited by in RCA: 4930] [Article Influence: 352.1] [Reference Citation Analysis (0)] |
| 2. | D’Ascenzo F, Cerrato E, Biondi-Zoccai G, Moretti C, Omedè P, Sciuto F, Bollati M, Modena MG, Gaita F, Sheiban I. Acute coronary syndromes in human immunodeficiency virus patients: a meta-analysis investigating adverse event rates and the role of antiretroviral therapy. Eur Heart J. 2012;33:875-880. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 87] [Cited by in RCA: 85] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 3. | Biondi-Zoccai G, D’Ascenzo F, Modena MG. Novel insights on HIV/AIDS and cardiac disease: shedding light on the HAART of Darkness. Eur Heart J. 2012;33:813-815. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 4. | Achouh P, Jemel A, Chaudeurge A, Redheuil A, Zegdi R, Fabiani JN. Aortic biological valve thrombosis in an HIV positive patient. Ann Thorac Surg. 2011;91:e90-e91. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Trachiotis GD, Alexander EP, Benator D, Gharagozloo F. Cardiac surgery in patients infected with the human immunodeficiency virus. Ann Thorac Surg. 2003;76:1114-1118; discussion 1118. [PubMed] |
| 6. | Sims DB, Uriel N, González-Costello J, Deng MC, Restaino SW, Farr MA, Takayama H, Mancini DM, Naka Y, Jorde UP. Human immunodeficiency virus infection and left ventricular assist devices: a case series. J Heart Lung Transplant. 2011;30:1060-1064. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 36] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 7. | van Wagenberg FS, Lehr EJ, Rehman A, Bonatti J. Is there a role for robotic totally endoscopic coronary artery bypass in HIV positive patients? Int J Med Robot. 2010;6:465-467. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Roques F, Michel P, Goldstone AR, Nashef SA. The logistic EuroSCORE. Eur Heart J. 2003;24:881-882. [PubMed] |
| 9. | Available from: http://riskcalc.sts.org/STSWebRiskCalc273/de.aspx. |