Published online Apr 16, 2014. doi: 10.12998/wjcc.v2.i4.100
Revised: January 27, 2014
Accepted: February 16, 2014
Published online: April 16, 2014
Processing time: 163 Days and 13.6 Hours
We present a case of a 33-year-old female who sustained multiple injuries of her spine, including spinous process fractures of C5 to C7 and a lamina fracture of C6 and C7. Her thoracic spine showed transverse process fractures of T4 to T10, a compression fracture and lamina fracture of T3, spinous process and transverse process fractures of T4 and T5, a rotation injury of T6, as well as a compression fracture of L1. Thirteen months after posterior thoracic spinal instrumentation, a pedicle screw was suspected to be in contact with the aorta, which was proved by computed tomography angiograms. Consequently, implant removal was planned with direct exposure of the aorta in order to allow for immediate repair if needed. So far, studies that compare different techniques to remove pedicle screws that are suspected to penetrate the aorta are missing. However, different techniques have been described in case reports, mainly minimally invasive endovascular techniques vs open techniques such as thoracotomy.
Core tip: Large vessel damage is described during spinal surgery and can lead to perforation of the aorta by misplaced pedicle screws. However, misplaced pedicle screws are often seen within postoperative computed tomography scans, only resulting in elective pedicle screw removal/exchange. Different techniques are available. We describe the use of a thoracotomy to prevent lethal hemorrhage. The importance of preoperative planning is highlighted, including pondering the advantages and disadvantages.
- Citation: Decker S, Omar M, Krettek C, Müller CW. Elective thoracotomy for pedicle screw removal to prevent severe aortic bleeding. World J Clin Cases 2014; 2(4): 100-103
- URL: https://www.wjgnet.com/2307-8960/full/v2/i4/100.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i4.100
Damage to large vessels like the aorta is a major complication in spinal surgery. This is a rare but life-threatening event. It is not uncommon that pedicle screws can penetrate the anterior cortex, therefore posing a risk of trauma to the aorta[1]. The anterior vertebral body is convex which increases the risk of penetration by the pedicle screws. As there is no biomechanical benefit from penetration of the anterior cortex with a pedicle screw, spinal surgeons generally do not strive for it[2].
Research has shown that the posterior spinal approach poses less risk for severe aortic bleeding than that of anterior surgery. Liljenqvist et al[3] reported 99 patients of whom only one underwent pedicle screw exchange because of its proximity to the aorta[4-6].
Major arterial bleeding has also been reported after lumbar disc surgery[7]. In particular, aortic damage has been reported after pedicle screw instrumentation. Most authors favor minimally invasive endovascular treatment using a femoral artery approach to implant a stent for a misplaced pedicle screw that penetrates the aorta before implant removal[8-11].
In the event of aortic bleeding during the removal of pedicle screws, the patient is at a particularly high risk for exsanguination. Different invasive strategies are available to protect the patient from life-threatening bleeding, of which thoracotomy with direct visualization of the aorta and endovascular approaches with the use of stents are the main strategies.
Whilst there are several reports on endovascular treatment of aortic damage due to spinal instrumentation, reports regarding thoracotomy are rare[12,13]. We present a case of a displaced pedicle screw with a concern of penetration of the aorta. Elective thoracotomy was performed during implant removal for best visualization and to give the opportunity for immediate aortic clamping in case of severe bleeding.
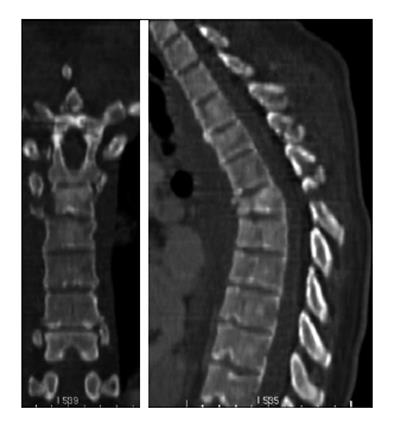
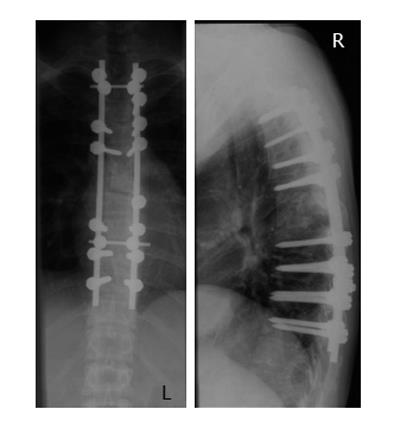
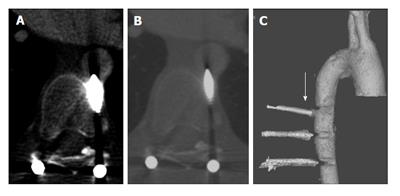
A 33-year-old woman was admitted to our emergency department with multiple injuries during a roll-over accident with her car. Endotracheal intubation was performed at the site of the accident without complications. No neurological deficit was reported. She suffered from severe thoracic trauma with several rib fractures on both sides, lung contusions, a hemopneumothorax, as well as a left forearm fracture. She also suffered from multiple severe spinal injuries. Her cervical spine had spinous process fractures of C5-C7 and a lamina fracture of C6-C7. Her thoracic spine showed transverse process fractures from T4 to T10, a compression fracture and lamina fracture of T3, spinous process and transverse process fractures of T4 and T5, a rotation injury of T6 (Figure 1), as well as a compression fracture of L1. We performed pedicle screw instrumentation from T2 to T10, as well as a laminectomy of T6 and posterior fusion on the day of injury (Figure 2). Three weeks later, an anterior interbody fusion of T5 to T7 was performed with an autologous iliac crest bone graft using a thoracoscopic approach. The postoperative computed tomography (CT) showed correct positioning of all pedicle screws, as well as the bone graft. Wound healing was regular without complications. She was discharged 23 d after admission and directly started rehabilitation. The patient stayed on our intensive care unit during the complete hospital stay. We allowed full weight-bearing. Follow-up care was performed by resident physicians. Thirteen months after anterior fusion, she presented in our outpatient clinic and a CT scan was performed to evaluate fracture healing as well as integration of the bone graft. There was a concern that the left pedicle screw of T7 was in contact with or could potentially perforate the aorta. This was not seen on the previous CT scan (Figure 3). Transesophageal sonography could not exclude an intraaortic position of the tip of the pedicle screw. Consequently, we planned the implant removal which was performed two weeks after the CT scan. This was done with the help of the vascular surgeons.
The patient was placed in the right lateral position. Using a median approach, we first removed the cross connector, the rod as well as all the pedicle screws on the right side. A thoracotomy was then performed through the 6th and 7th intercostal space. Anterior preparation of the T7 left pedicle screw, which penetrated the anterior cortex of the corpus vertebrae, was done for optimal visualization before implant removal; the screw did not penetrate the aorta. The aorta was pulled across using a retractor so that it did not cover the screw of T7. We then removed the left rod as well as all the pedicle screws. No bleeding was observed with removal of the T7 pedicle screw. The incision was closed in layers after irrigation and placement of a chest tube and drains at the back. One month later, the patient needed revision surgery because of a seroma at the back. The seroma had been apparent since discharge from the hospital after implant removal and was punctured in our outpatient clinic three times before revision surgery. Afterwards, to our knowledge no further complication occurred. However, wound healing was monitored by a resident physician between the initial surgery and the implant removal.
When surgeons suspect that a pedicle screw affects the aorta, one should keep in mind that implant removal should not be performed with the patient in a prone position without further precautions. Instead, intensive preoperative planning is needed and vascular surgeons should be contacted in advance if the trauma or orthopedic surgeon is not qualified to manage large vessel damage. Preoperative planning should include good visualization of the spatial relationships of the tip of the screw as well as the involved vessels. Different techniques are available, mainly minimally invasive endovascular techniques as well as a thoracotomy[8-13]. Clear guidelines as to which technique is best are missing so far. In this case, we decided to perform a thoracotomy to directly visualize the left T7 pedicle screw as we were afraid of not being able to control bleeding in case of aortic rupture using an endovascular approach. Although this is a very invasive technique, it provides the best visualization as well as access for a fast intervention like aortic clamping in the event of aortic injury. Nevertheless, alternatives such as preoperative implantation of femoral arterial access for quick endovascular intervention have to be considered and extensively discussed with the patient and the team preoperatively. When pedicle screw removal is planned because of its proximity to the aorta, the patient should be clearly informed about the risk of bleeding, as well as the various options to prevent life-threatening bleeding. We recommend a multi-disciplinary discussion of these surgeries to evaluate which technique is best. Generally, surgeons should decide depending on two main aspects. First, the technique has to be safe to prevent lethal hemorrhage and surgeons have to feel safe. Second, the surgery should be as minimally invasive as possible. E.g., a thoracotomy[12,13] is very invasive and should be avoided whenever possible. In conclusion, this is a very subjective decision. Clear data that help to decide which technique is best in which situation is missing and, in contrast, the decision-making process depends on individual surgical competence and experience.
The patient described did not show any symptoms 13 mo after posterior instrumentation of multiple spinal fractures. However, a computed tomography (CT) scan did raise suspicion that a pedicle screw could perforate the aorta.
Like in the CT, intraaortic positioning of the pedicle screw could not be excluded by transesophageal sonography.
The authors planned implant removal using a thoracotomy for direct visualization of the aorta which did not appear to be perforated.
Thoracotomy is a very invasive technique that provides the best visualization during surgery but there have also been reports that described minimally invasive endovascular treatment.
The authors experienced the importance of intensive preoperative planning, as well as a multidisciplinary approach to discuss all available treatment options to reduce the risk of lethal hemorrhage during surgery.
The strength of this case report is that it describes a rare situation that can, however, be seen by every spine surgeon. Although the authors describe a very invasive technique, other techniques have also been described. Nevertheless, the decision of which technique to use is very subjective as experience with this specific topic is low.
The study reported how a 33-year-old patient underwent a thoracotomy for pedicle screw removal due to suspected contact with the aorta. It is an unusual but not unheard of occurrence which is valuable to review.
P- Reviewers: Camm EJ, Karmy-Jones R, Paraskevas KI S- Editor: Song XX L- Editor: Roemmele A E- Editor: Liu SQ
| 1. | Vaccaro AR, Rizzolo SJ, Balderston RA, Allardyce TJ, Garfin SR, Dolinskas C, An HS. Placement of pedicle screws in the thoracic spine. Part II: An anatomical and radiographic assessment. J Bone Joint Surg Am. 1995;77:1200-1206. [PubMed] |
| 2. | Könings P, Böhmer G. Verletzungen des thorakolumbalen Übergangs. Trauma und Berufskrankheit. 2000;2:162-166. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.0] [Reference Citation Analysis (0)] |
| 3. | Liljenqvist U, Lepsien U, Hackenberg L, Niemeyer T, Halm H. Comparative analysis of pedicle screw and hook instrumentation in posterior correction and fusion of idiopathic thoracic scoliosis. Eur Spine J. 2002;11:336-343. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 220] [Cited by in RCA: 209] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 4. | Ohnishi T, Neo M, Matsushita M, Komeda M, Koyama T, Nakamura T. Delayed aortic rupture caused by an implanted anterior spinal device. Case report. J Neurosurg. 2001;95:253-256. [PubMed] |
| 5. | Woolsey RM. Aortic laceration after anterior spinal fusion. Surg Neurol. 1986;25:267-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 45] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Matsuzaki H, Tokuhashi Y, Wakabayashi K, Kitamura S. Penetration of a screw into the thoracic aorta in anterior spinal instrumentation. A case report. Spine (Phila Pa 1976). 1993;18:2327-2331. [PubMed] |
| 7. | Brewster DC, May AR, Darling RC, Abbott WM, Moncure AC. Variable manifestations of vascular injury during lumbar disk surgery. Arch Surg. 1979;114:1026-1030. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 74] [Cited by in RCA: 74] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 8. | Minor ME, Morrissey NJ, Peress R, Carroccio A, Ellozy S, Agarwal G, Teodorescu V, Hollier LH, Marin ML. Endovascular treatment of an iatrogenic thoracic aortic injury after spinal instrumentation: case report. J Vasc Surg. 2004;39:893-896. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 98] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 9. | Freyrie A, Gasbarrini A, Simoes CE, Gallitto E, Gargiulo M. Delayed presentation of a thoracic aortic injury with a vertebral pedicle screw. Ann Vasc Surg. 2013;27:499.e1-499.e3. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 7] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 10. | Iyer MH, Engoren M, Martin MW. Echo rounds: Transesophageal echocardiography: identification and management of a misplaced pedicle screw in the descending thoracic aorta after posterior spinal fusion. Anesth Analg. 2013;116:303-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Carmignani A, Lentini S, Acri E, Vazzana G, Campello M, Volpe P, Acri IE, Spinelli F. Combined thoracic endovascular aortic repair and neurosurgical intervention for injury due to posterior spine surgery. J Card Surg. 2013;28:163-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 12. | Fukuda W, Aoki C, Daitoku K, Taniguchi S, Fukuda I. Screw in the aorta: minimally invasive graft replacement for chronic aortic erosion by spinal instrument. Ann Thorac Cardiovasc Surg. 2013;19:320-322. [PubMed] |
| 13. | Tschoeke SK, Gahr P, Krug L, Kasper AS, Heyde CE, Ertel W. Late diagnosis of pedicle screw malplacement with perforation of the thoracic aorta after posterior stabilization in a patient with multiple myeloma: case report. Spine (Phila Pa 1976). 2011;36:E886-E890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 24] [Article Influence: 1.7] [Reference Citation Analysis (0)] |