Published online Mar 16, 2014. doi: 10.12998/wjcc.v2.i3.57
Revised: January 2, 2014
Accepted: January 17, 2014
Published online: March 16, 2014
Processing time: 141 Days and 1.8 Hours
Chordomas are malignant tumors arising from notochordal remnants. They are the most frequent tumors of the spine after plasmacytomas. Only 6% of chordomas are localized to the cervical level. In young patients, chordomas are rare and unpredictable. Despite this, the treatment of choice remains the total resection, as much as possible, followed by proton beam radiation. This case was managed using a precarotid and retrocarotid approach at the same time. The tumor was completely resected with the edges free from disease. The cervical spine was stabilized with an anterior plating C2-C4. Eighteen months after surgery the patient is still free from illness. Multilevel oblique corpectomies are an available and safe option for the treatment of upper cervical chordomas.
Core tip: In young patients, chordomas are rare and unpredictable. Despite this, the treatment of choice remains the total resection, as much as possible, followed by proton beam radiation. When there is a precarotid and retrocarotid extension, the removal by a multilevel oblique corpectomy seems to be a feasible and safe surgical technique.
- Citation: Delfini R, Marruzzo D, Tarantino R, Marotta N, Landi A. Multilevel oblique corpectomies as an effective surgical option to treat cervical chordoma in a young girl. World J Clin Cases 2014; 2(3): 57-61
- URL: https://www.wjgnet.com/2307-8960/full/v2/i3/57.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i3.57
Chordomas are malignant tumors arising from notochordal remnants and are the most frequent tumors of the spine after plasmacytomas. Only 6% of chordomas are localized at cervical level[1,2]. The treatment of choice is total resection, or removing as much as possible of the tumor, followed by proton beam radiation. As emphasized in previous studies, total resection and, in particular, en bloc removal are not always possible, especially in the upper cervical localization and when the tumor englobes the epidural space (as in our case). This is a consequence both of the fact that the cervical chordoma infiltrates the nearby structures and that the margins of the total resection include unresectable structures. In young patients, chordomas are rare and unpredictable. We describe a rare case of an extensive cervical chordoma in a 14-year-old girl treated simultaneously by a precarotid and retrocarotid approach.
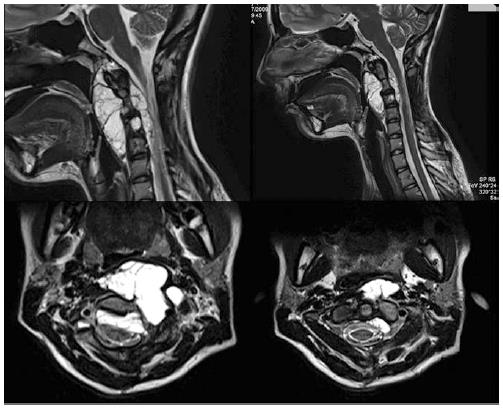
A 14-year-old girl was referred to our institution with cervical pain, dysphagia, hyperreflexia and weakness of the four limbs for 8 mo. The preoperative magnetic resonance imaging (MRI) showed a lesion of C2-C3-C4 with marked retropharyngeal and epidural space involvement (Figure 1). The tumor extended from the C1 anterior tuberculum as far as the C5 superior plate. Since biopsy had been performed in another institute via C2-C3-C4 interhemilaminectomy, the definitive result of the biopsy was not available.
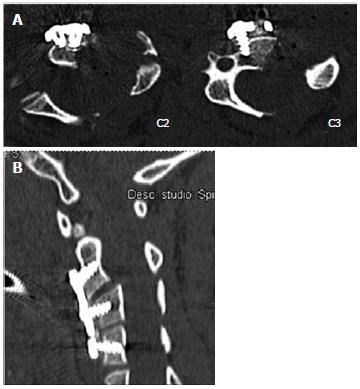
A pre-operative CT showed erosion of the C2-C3-C4 vertebral bodies (Figure 2). An angio-MRI with gadolinium administration pointed out that the left vertebral artery (VA) was encapsulated and displaced without reduction of the vessel diameter. The tumor showed a spare contrast enhancement with gadolinium and in DWI was hyperintense in DWI sequences. Relating to the clinical and radiological features, there were two diagnostic hypotheses, either an epidermoid cyst or chordoma. The tumor was classified IB according to the Enneking classification[3]. It was distributed to layers A-F and sectors 4-7 according to the Weinstein Boriani Biagini Classification[4].
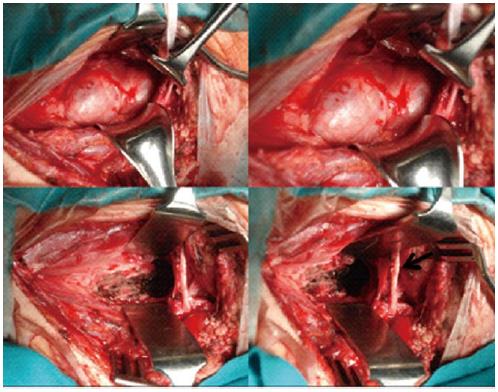
Surgical strategy consisted of a precarotid and retrocarotid approach during a single operation. The patient was positioned in the supine position with her head rotated 30° to the right. A presternocleidomastoid longitudinal skin incision was performed starting from left mastoid process. Firstly, the precarotid approach was performed through which the retropharyngeal portion was removed (Figure 3). Infiltrated bone, the portion around VA and the epidural space component were removed via the second approach, via multilevel oblique corpectomies. During surgery we employed ecodoppler monitoring to control the vertebral artery, as well as the operative microscope and the cavitron ultrasonic surgical aspirator, to remove the epidural component of the tumor. The retropharyngeal component was removed by an en bloc excision, while an intralesional excision was performed to remove the residual tumor. The tumor was completely resected together with the disease-free borders. A C2-C3 and C3-C4 discectomy with apposition of synthetic bone was performed to improve and speed up fusion and the cervical spine was stabilized by means of C2-C4 anterior plating.
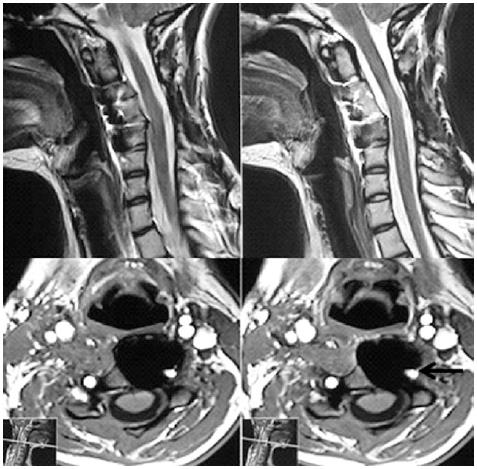
A post-operative computed tomography (CT)-scan confirmed the correct position of the plate and the screws (Figure 4). The second day after surgery, the patient was free of any neurological deficit and was able to stand up and started to walk. The patient was discharged from hospital the seventh day after surgery. Twenty days after surgery, a post-operative MRI showed total resection of the tumor. A Shantz cervical collar was fitted for 45 d. Forty days after surgery, the patient received postoperative proton beam radiation therapy. A clinical and radiological control, consisting of cervical MRI with gadolinium, was performed every 6 mo. Twenty days after surgery, the patient returned to school and at present leads a normal life. Fusion was documented at 40 d. No recurrence or metastasis was observed 48 mo after the operation (Figure 5).
Chordoma is a low-grade malignant tumor which is rare (incidence of 0.51 cases/million), and is generally slow-growing, radioresistant and has a high tendency of recurrence[4]. Chordomas arise from remnants of the notochord, especially at the two end portions. 32% of chordomas arise from the clivus, 33% from the spinal cord, 29% from the sacrococcygeal region and just 6% from the cervical spine[1]. The treatment of choice is en bloc total resection followed by radiation therapy. The chordoma is sensitive to a high dose of “standard” radiation. However, the Bragg peak effect of a proton beam is useful for delivering a high radiation dose without damaging the tissue around the tumor and the spinal cord[1,5]. Total resection and, above all, en bloc removal are not always possible, especially in the upper cervical localization and when the tumor englobes the epidural space (as in our case). This is a consequence of the fact that the cervical chordoma infiltrates the nearby structures; moreover, the margins of the total resection include non-resectable structures like the vertebral artery. However, as pointed out by Boriani et al[6], “en bloc removal of a bone tumor is possible for a tumor arising in the scapula (scapulectomy) and tibia (above knee amputation), but it is absolutely impossible for a spinal tumor. In this sense, even if the spinal cord is sectioned above and below, the epidural space represents a compartment extending from the skull to the coccyx. A trial of aggressive chemotherapy is warranted in patients with metastatic chordomas. In the literature[7-9], two protocols were primarily used, consisting of ifosfamide or imatinib mesylate. Several approaches for treating upper cervical chordoma have been described in the literature: the anterior precarotid cervical approach (bilateral or not); the anterolateral retrocarotid approach; the transoral approach[10]; and anterior fixation or anterior and posterior fixation[11].
In the case described here, an anterior precarotid and an anterolateral retrocarotid (presternocleidomastoid) approach were performed at the same time. The advantages of this technique were good control of the left vertebral artery, multilevel oblique corpectomies, removal of the epidural space component of the chordoma and the possibility of anterior plating. It was impossible to perform an en bloc excision for the epidural space component because the tumor enclosed the left VA[1]. The procedure that we performed avoided binding of the VA and injuring the cervical roots, with a better outcome in comparison to some recent works[10,12]. Moreover, only anterior fixation was necessary because we performed multilevel oblique corpectomies, thus sparing the posterior structures of the cervical spine. This procedure made it possible to avoid occipitocervical fixation in a 14-year-old girl and the consequent limitations in movement.
In our opinion, a more aggressive strategy (multiple spondylectomy), which has a high morbidity, is justified for the treatment of cervical chordoma because chordomas are tumors whose biological behavior is difficult to predict. Despite this, the most recent publications[1,10-19] have shown that there are no important differences between patients operated on using an aggressive strategy (spondylectomy) and those submitted to corpectomies. So in our opinion, multilevel oblique corpectomies seem to be a feasible and safe surgical technique to treat a cervical chordoma.
A 14-year-old girl was referred to our institution with cervical pain, dysphagia, hyperreflexia and weakness of the four limbs for 8 mo.
The preoperative magnetic resonance imaging showed a lesion of C2-C3-C4 with marked retropharyngeal and epidural space involvement.
Surgical strategy consisted of a precarotid and retrocarotid approach during a single operation.
Multilevel oblique corpectomies seems to be a feasible and safe surgical technique to treat a cervical chordoma.
This is well written case report presenting a rare condition which is explained well.
P- Reviewers: Dereci O, Huang JP, Maharaj D, Muluk NB, Shipman A S- Editor: Song XX L- Editor: Roemmele A E- Editor: Wu HL
| 1. | Barrenechea IJ, Perin NI, Triana A, Lesser J, Costantino P, Sen C. Surgical management of chordomas of the cervical spine. J Neurosurg Spine. 2007;6:398-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 74] [Article Influence: 4.1] [Reference Citation Analysis (0)] |
| 2. | Currier BL, Papagelopoulos PJ, Krauss WE, Unni KK, Yaszemski MJ. Total en bloc spondylectomy of C5 vertebra for chordoma. Spine (Phila Pa 1976). 2007;32:E294-E299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Enneking WF, Spanier SS, Goodman MA. A system for the surgical staging of musculoskeletal sarcoma. Clin Orthop Relat Res. 1980;106-120. [PubMed] |
| 4. | Greenberg MS. Handbook of Neurosurgery. New York: Thieme Medical Publishers 2006; . |
| 5. | Noël G, Feuvret L, Ferrand R, Boisserie G, Mazeron JJ, Habrand JL. Radiotherapeutic factors in the management of cervical-basal chordomas and chondrosarcomas. Neurosurgery. 2004;55:1252-1260; discussion 1260-1262. [PubMed] |
| 6. | Boriani S, Weinstein JN, Biagini R. Primary bone tumors of the spine. Terminology and surgical staging. Spine (Phila Pa 1976). 1997;22:1036-1044. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 469] [Cited by in RCA: 425] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 7. | Chambers PW, Schwinn CP. Chordoma. A clinicopathologic study of metastasis. Am J Clin Pathol. 1979;72:765-776. [PubMed] |
| 8. | Fleming GF, Heimann PS, Stephens JK, Simon MA, Ferguson MK, Benjamin RS, Samuels BL. Dedifferentiated chordoma. Response to aggressive chemotherapy in two cases. Cancer. 1993;72:714-718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 9. | Casali PG, Stacchiotti S, Sangalli C, Olmi P, Gronchi A. Chordoma. Curr Opin Oncol. 2007;19:367-370. [PubMed] |
| 10. | Jiang L, Liu ZJ, Liu XG, Ma QJ, Wei F, Lv Y, Dang GT. Upper cervical spine chordoma of C2-C3. Eur Spine J. 2009;18:293-298; discussion 298-300. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 39] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 11. | Leitner Y, Shabat S, Boriani L, Boriani S. En bloc resection of a C4 chordoma: surgical technique. Eur Spine J. 2007;16:2238-2242. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 25] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Suchomel P, Buchvald P, Barsa P, Froehlich R, Choutka O, Krejzar Z, Sourkova P, Endrych L, Dzan L. Single-stage total C-2 intralesional spondylectomy for chordoma with three-column reconstruction. Technical note. J Neurosurg Spine. 2007;6:611-618. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 37] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 13. | Fujita T, Kawahara N, Matsumoto T, Tomita K. Chordoma in the cervical spine managed with en bloc excision. Spine (Phila Pa 1976). 1999;24:1848-1851. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 60] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 14. | George B, Zerah M, Lot G, Hurth M. Oblique transcorporeal approach to anteriorly located lesions in the cervical spinal canal. Acta Neurochir (Wien). 1993;121:187-190. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 64] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Chibbaro S, Mirone G, Bresson D, George B. Cervical spine lateral approach for myeloradiculopathy: technique and pitfalls. Surg Neurol. 2009;72:318-324; discussion 324. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 16. | Lim JJ, Kim SH, Cho KH, Yoon DH, Kim SH. Chordomas involving multiple neuraxial bones. J Korean Neurosurg Soc. 2009;45:35-38. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 17. | Bruneau M, Cornelius JF, George B. Microsurgical cervical nerve root decompression by anterolateral approach. Neurosurgery. 2006;58:ONS108-ONS13; discussion ONS108-ONS13. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 18. | Bruneau M, Cornelius JF, George B. Multilevel oblique corpectomies: surgical indications and technique. Neurosurgery. 2007;61:106-112; discussion 112. [PubMed] |
| 19. | Kelley SP, Ashford RU, Rao AS, Dickson RA. Primary bone tumours of the spine: a 42-year survey from the Leeds Regional Bone Tumour Registry. Eur Spine J. 2007;16:405-409. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 116] [Article Influence: 6.4] [Reference Citation Analysis (0)] |