Published online Dec 16, 2014. doi: 10.12998/wjcc.v2.i12.934
Revised: September 20, 2014
Accepted: October 14, 2014
Published online: December 16, 2014
Processing time: 208 Days and 19.9 Hours
We report a case of an 11-year-old boy with diagnosed but uncorrected tetralogy of Fallot presented to us for brain abscess drainage. The child was managed successfully with scalp block with sedation.
Core tip: We present a case report describing the use of scalp block combined with sedation for brain abscess drainage in a child with uncorrected tetralogy of Fallot. The goal should be to maintain hemodynamic stability and avoid any increase of a right to left shunt. Therefore, we decided to perform scalp block combined with sedation in this child. We used O2 inhalation, analgesia and sedation with fentanyl, midazolam and ketamine to alleviate anxiety and increase systemic vascular resistance, pulmonary perfusion and oxygenation.
- Citation: Sethi S, Kapil S. Scalp block for brain abscess drainage in a patient with uncorrected tetralogy of Fallot. World J Clin Cases 2014; 2(12): 934-937
- URL: https://www.wjgnet.com/2307-8960/full/v2/i12/934.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i12.934
Tetralogy of Fallot (TOF), with an incidence of 10% of all congenital heart diseases[1], is the commonest cyanotic congenital heart disease[1] and has a dilated aorta which overrides the large ventricular septal defect along with right ventricular outflow tract (RVOT) obstruction and hypertrophy of right ventricle. RVOT can be valvular, infundibular or both[2]. There have been several case reports of successful management of TOF presenting for brain abscess drainage, cesarean section and major abdominal surgeries[3-5]. We present a case report describing the use of scalp block combined with sedation for brain abscess drainage in a child with uncorrected TOF.
An 11-year-old male child weighing 44 kg presented to us in the emergency department with a history of fever up to 102 ºF, headache and vomiting for 10 d. The child was a known case of TOF but had not undergone any surgical repair. His effort tolerance was poor. He had a history of cyanotic spells since childhood but was not on any medication. On examination, the child was conscious, irritable and crying. The child did not show any signs of raised intracranial pressure. Central cyanosis and clubbing were present. He had a pulse rate of 76 per minute with a blood pressure of 110/60 mmHg. On examination of the cardiovascular system, the apex beat was found in the left 5th intercostal space in the midclavicular line and was associated with a left parasternal heave. 1st and 2nd heart sounds and a loud pulmonary component of the 2nd heart sound were audible, along with a pansystolic murmur (Grade 4/6) at the left lower sternal border. No focal deficit was found on neurological examination. The respiratory and gastrointestinal systems were normal on examination.
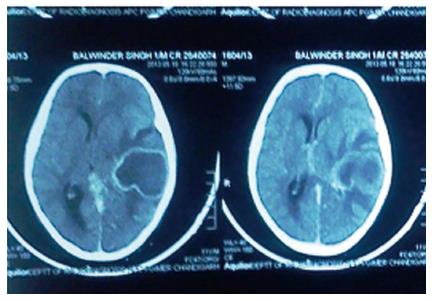
Chest X-ray (Figure 1) showed an enlarged cardiac shadow with left ventricular hypertrophy and dilated pulmonary arteries. Electrocardiogram (ECG) revealed sinus rhythm with right ventricular hypertrophy. Echocardiography (ECHO) showed a large ventricular septal defect (VSD) of 13 mm, 60% overriding of the aorta, right ventricular hypertrophy and right ventricular tract outflow obstruction and ejection fraction of 0.6. Cardiac catheterization was not done. Contrast-enhanced computed tomography (Figure 2) showed a left temporoparietal abscess with no uncal herniation, along with a midline shift of 2 mm. His hematocrit was 58% with a platelet count of 105 × 109/L. The child’s serum electrolytes, coagulation studies and renal function tests were within normal limits. The baseline Arterial Blood Gas analysis revealed pH 7.419, Po2 35.5 mmHg, Pco2 31.8 mmHg, HCO3 20.1 mEq/L, SPO2 68.7% and base excess -3.3. The child received infective endocarditis prophylaxis prior to the surgery, was allowed oral intake of fluids up to 2 h before surgery and normal saline was used as the maintenance fluid thereafter in the ward. In the operation theater, standard monitoring was done with noninvasive blood pressure, pulse oximetry, ECG and temperature. A NeoStar™ triple lumen central venous catheter was in situ as it was inserted when the child presented to us in the emergency department. A 20 G arterial cannula (Becton Dickinson Critical Care Systems, Singapore) was inserted into the radial artery under local anesthesia. The baseline heart rate was 70 beats per minute with an invasive blood pressure of 116/68 mmHg and a central venous pressure (CVP) of 10 cm of H2O. The child had 64% SPO2 with 50% O2 with a Venturi face mask. Normal saline was used as maintenance fluid with the dose of 4 mL/kg per hour.
The scalp block was given with 20 mL of 0.75% ropivacaine without adrenaline (3-4 mL for each nerve) to block the supratrochlear, supraorbital, zygomaticotemporal, auriculotemporal, greater and lesser occipital nerve. The block was supplemented with fentanyl 20 μg iv, followed by ketamine 20 mg iv and midazolam 0.2 mg iv at the time of the burr hole. The child was kept on spontaneous respiration throughout the procedure with a 50% oxygen and air mixture. At the time of dural opening, intravenous ketamine 20 mg was repeated. Normal saline was administered to keep CVP in range of 14-16 cm of H2O. The procedure lasted for 30 min and the intraoperative course was uneventful, with maintenance of hemodynamic parameters and acid base status within normal limits and a SPO2 of 69.5%.
For the anesthetic management of these patients, one should be careful about the drugs and events that may increase the R-L shunt[6]. The severity of the disease directly correlates with the size of VSD, severity of pulmonary stenosis and functional status of the right ventricle[7]. Complications of right to left shunts include chronic hypoxia leading to pulmonary vasoconstriction, altered acid base status, polycythemia, coagulopathy, infective endocarditis and cerebral abscess due to increased risk of paradoxical emboli. The reported incidence of brain abscess in patients with cyanotic heart disease is between 5% and 18.7%[8].
Anesthetic management of these patients is always a challenge for the anesthetists because of the cardiopulmonary and coagulation abnormalities, dehydration and electrolyte imbalance, along with abscess-induced complications of seizures, meningitis and raised intracranial pressure[4].
General anesthesia with controlled ventilation has the advantage of better oxygenation but can be associated with the risk of hemodynamic instability, along with compression of pulmonary vessels, impaired gas exchange and academia[9].
Most of the agents used for induction and maintenance of general anesthesia may also lead to myocardial depression, along with reduction of SVR.
The goal should be to maintain hemodynamic stability and avoid the changes that would increase the right to left shunt. Therefore, we decided to perform scalp block combined with sedation in this child.
Factors such as thorough preoperative examination, ECHO, treatment of any chest infections, cardiologist consultation, documentation of preoperative cardiac and neurological status and correction of any coagulopathy were necessary and taken care of in our child.
Prolonged fasting is better avoided in these patients and intake of clear fluids up to two hours prior to the surgery should be allowed. We followed the same guidelines in our patient with normal saline as a maintenance fluid in the ward. Prevention of dehydration is also important as these patients have an increased hematocrit. Patients with a hematocrit ≥ 60% are susceptible to develop coagulopathy and preoperative phlebotomy is beneficial in such cases. Our child had a hematocrit of 58% and preoperative phlebotomy was not performed as it was an emergency procedure, but adequate precautions to prevent dehydration and liberal fluid administration were done to keep the CVP in the range of 14-16 cm of H2O. Fluid boluses of 20 mL/kg may be required to increase the blood pressure and RV preload[10].
Air bubbles are also a preventable cause of perioperative morbidity in patients with shunting as air or particulate matter may be shunted directly into the arterial bed[11,12] and we took measures to prevent this.
We used O2 inhalation, analgesia and sedation with fentanyl, midazolam and ketamine to alleviate anxiety and increase SVR, pulmonary perfusion and oxygenation. Although O2 inhalation, fentanyl and midazolam cannot increase SVR, they avoid increasing PVR. Ketamine may increase SVR at some level or more importantly can prevent lowering of SVR and it helped our patient by decreasing the left to right shunt.
Ketamine has also been shown to be better in children with pulmonary hypertension[13,14] although this is not the cause of cyanosis in these patients but it is the fall in SVR leading to left-right shunt which causes hypoxia. In one study of 18 neonates who had complex cardiac defects, ketamine was used most commonly when intubation was not required for surgery[15]. Anesthetic agents like sevoflurane, isoflurane and fentanyl/midazolam infusions have no effect on the shunt fraction of children with shunts[16-18].
Scalp block is a well-established technique for craniotomy, increasingly being used for epilepsy surgery, temporal lobectomy where the excision encroaches on eloquent cortex areas[19].
Scalp block may be given preoperatively to reduce the hemodynamic response to pin holder application and postoperatively before the emergence to decrease the severity of postoperative pain. They also decrease intra and postoperative opioid requirement[20,21].
We used 0.75% ropivacaine without adrenaline for administering scalp block as the addition of adrenaline may cause tachycardia which is very dangerous in patients with uncorrected TOF because it may cause infundibular spasm and a cyanotic spell.
Scalp block along with sedation is being used successfully in our institute for patients with chronic subdural hemorrhage. Since the patient we encountered had to undergo an emergency procedure with no time for cardiac catheterization and medical optimization of the patient, we decided to proceed with regional anesthesia with sedation and invasive monitoring in the patient.
The avoidance of general anesthesia due to medical reasons in selected patients and with the thorough anatomical knowledge of nerve blocks, this underestimated regional technique of scalp block with sedation may be considered as an alternative technique in selective patients with unrepaired TOF and has proved to be an extremely rewarding procedure for the neuroanesthetist whilst offering the best possible outcome for the patient.
An 11-year-old male, a known case of tetralogy of Fallot (TOF), presented with fever (up to 102 ºF), headache and vomiting for the past 10 d.
On examination, the child had central cyanosis, clubbing, loud P2 and grade IV pansystolic murmur but there were no signs of raised intracranial pressure and no neurological focal deficit.
A known case of TOF who had not undergone any surgical repair and presented with brain abscess.
The patient had a high hematocrit with a normal coagulation profile. The baseline Arterial Blood Gas analysis revealed pH 7.419, Po2 35.5 mmHg, Pco2 31.8 mmHg, HCO3 20.1 mEq/L, SPO2 68.7% and BE -3.3.
Echocardiography revealed a large ventricular septal defect of 13 mm, 60% overriding of aorta, right ventricular tract outflow obstruction and ejection fraction of 0.6, while contrast-enhanced computed tomography (Figure 2) showed a left temporoparietal abscess with no uncal herniation and a midline shift of 2 mm.
The patient was diagnosed as a brain abscess with uncorrected TOF.
Child was not on any medication and presented to us in the emergency department. The child received infective endocarditis prophylaxis prior to the surgery.
Uncorrected TOF presents as a challenge to anesthetists and a thorough knowledge about the physiological and pathological changes occurring with the disease is essential for the safe management of the patient in the perioperative period. Regional anaesthesia should be considered as an alternative to general anesthesia when feasible.
A good paper that can be accepted.
P- Reviewer: Ong HT, Ozcengiz D, Nagashima G S- Editor: Ji FF L- Editor: Roemmele A E- Editor: Wu HL
| 1. | Moller JH, Neal WA. Fetal, neonatal and infant cardiac disease. Norwalk: Appleton and Lange 1990; Available from: http://www.amazon.com/Fetal-Neonatal-Infant-Cardiac-Disease/dp/083852575X. |
| 2. | Behram RE, Kleigman RM, Nelson WE, Vaughan VC. Congenital cardiac disease with cyanosis. Philadelphia: WB Saunders 1992; 1149-1153. |
| 3. | Katsetos CP, Kontoyannis MB, Koumousidis A, Petropoulou O, Delos C, Katsoulis M. Uncorrected tetralogy of Fallot and pregnancy: a case report. Clin Exp Obstet Gynecol. 2012;39:382-383. [PubMed] |
| 4. | Raha A, Ganjoo P, Singh A, Tandon MS, Singh D. Surgery for brain abscess in children with cyanotic heart disease: An anesthetic challenge. J Pediatr Neurosci. 2012;7:23-26. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Haack M, Machotta A, Boemke W, Höhne C. Anesthesia in an infant with uncorrected tetralogy of Fallot for transanal pull-through for Hirschsprung’s disease. Paediatr Anaesth. 2006;16:95-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 6. | Stoelting Robert K; Congenital heart disease. In: Anaesthesia and coexisting disease. 3rd ed. Churchill livingstone: 42-45. . |
| 7. | Webb GD, Smallhorn JF, Therrien J, Redington AN. Congenital heart disease. Braunwald’s heart disease: a textbook of cardiovascular medicine. 7th ed. Philadelphia: W. B. Saunders 2005; 1489-1552. |
| 8. | Fischbein CA, Rosenthal A, Fischer EG, Nadas AS, Welch K. Risk factors of brain abscess in patients with congenital heart disease. Am J Cardiol. 1974;34:97-102. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 60] [Cited by in RCA: 61] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 10. | Twite MD, Ing RJ. Tetralogy of Fallot: perioperative anesthetic management of children and adults. Semin Cardiothorac Vasc Anesth. 2012;16:97-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 16] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 11. | Hickey PR. Anaesthesia for treatment of congenital heart disease. Principles and Practice of Anaesthesiology. St. Louis, Missouri: Mosby Year Book 1993; 1681-1718. |
| 12. | Moore RA. Anaesthetizing the child with congenital heart disease for non-cardiac surgery. Philadelphia: Lippincott Williams & Wilkins 1994; 211-226. |
| 13. | Williams GD, Maan H, Ramamoorthy C, Kamra K, Bratton SL, Bair E, Kuan CC, Hammer GB, Feinstein JA. Perioperative complications in children with pulmonary hypertension undergoing general anesthesia with ketamine. Paediatr Anaesth. 2010;20:28-37. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 48] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Williams GD, Philip BM, Chu LF, Boltz MG, Kamra K, Terwey H, Hammer GB, Perry SB, Feinstein JA, Ramamoorthy C. Ketamine does not increase pulmonary vascular resistance in children with pulmonary hypertension undergoing sevoflurane anesthesia and spontaneous ventilation. Anesth Analg. 2007;105:1578-1584, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 58] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 15. | Walker A, Stokes M, Moriarty A. Anesthesia for major general surgery in neonates with complex cardiac defects. Paediatr Anaesth. 2009;19:119-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 27] [Cited by in RCA: 25] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 16. | Ikemba CM, Su JT, Stayer SA, Miller-Hance WC, Eidem BW, Bezold LI, Hall SR, Havemann LM, Andropoulos DB. Myocardial performance index with sevoflurane-pancuronium versus fentanyl-midazolam-pancuronium in infants with a functional single ventricle. Anesthesiology. 2004;101:1298-1305. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 17. | Laird TH, Stayer SA, Rivenes SM, Lewin MB, McKenzie ED, Fraser CD, Andropoulos DB. Pulmonary-to-systemic blood flow ratio effects of sevoflurane, isoflurane, halothane, and fentanyl/midazolam with 100% oxygen in children with congenital heart disease. Anesth Analg. 2002;95:1200-1206, table of contents. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 56] [Cited by in RCA: 58] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 18. | Rivenes SM, Lewin MB, Stayer SA, Bent ST, Schoenig HM, McKenzie ED, Fraser CD, Andropoulos DB. Cardiovascular effects of sevoflurane, isoflurane, halothane, and fentanyl-midazolam in children with congenital heart disease: an echocardiographic study of myocardial contractility and hemodynamics. Anesthesiology. 2001;94:223-229. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 70] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 19. | Herrick IA, Gelb AW. Anesthesia for temporal lobe epilepsy surgery. Can J Neurol Sci. 2000;27 Suppl 1:S64-S67; discussion S92-S97. [PubMed] |
| 20. | Nguyen A, Girard F, Boudreault D, Fugère F, Ruel M, Moumdjian R, Bouthilier A, Caron JL, Bojanowski MW, Girard DC. Scalp nerve blocks decrease the severity of pain after craniotomy. Anesth Analg. 2001;93:1272-1276. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 111] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 21. | Pinosky ML, Fishman RL, Reeves ST, Harvey SC, Patel S, Palesch Y, Dorman BH. The effect of bupivacaine skull block on the hemodynamic response to craniotomy. Anesth Analg. 1996;83:1256-1261. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 88] [Article Influence: 3.0] [Reference Citation Analysis (0)] |