Published online Dec 16, 2014. doi: 10.12998/wjcc.v2.i12.907
Revised: August 10, 2014
Accepted: September 23, 2014
Published online: December 16, 2014
Processing time: 181 Days and 1.4 Hours
Dural arteriovenous fistula (DAVF) is a rare type of cerebral arteriovenous malformation. Common presenting symptoms are related to hemorrhage. However, rarely these patients may present with myelopathy. We present two cases of DAVF presenting as rapidly progressive myelopathy. Two treatment options are available: microsurgical interruption of the fistula and endovascular embolization. These treatment options of DAVFs have improved significantly in the last decade. The optimal treatment of DAVFs remains controversial, and there is an ongoing debate as to whether primary endovascular or primary microsurgical treatment is the optimal management for these lesions. However, despite treatment a high percentage of patients are still left with severe disability. The potential for functional ambulation in patients with DAVF is related to the time of intervention. This emphasizes the important of early diagnosis and early intervention in DAVF. The eventual outcome may depend on several factors, such as the duration of symptoms, the degree of disability before treatment, and the success of the initial procedure to close the fistula. The usage of magnetic resonance imaging and selective angiography has significantly improved the ability to characterize DAVFs, however, these lesions remain inefficiently diagnosed. If intervention is delayed even prolonged time in rehabilitation does not change the grave prognosis. This review outlines the presentation, classication and management of DAVF as well as discussing patient outcomes.
Core tip: Tentorial dural arteriovenous fistulas (DAVF) are an uncommon entity, and myelopathy as a result of these AV fistulas is even more uncommon. We present two cases of myelopathy as a result of dural AV fistulas. This review highlights the classification of dural AV fistulas, the various diagnostic modalities available for diagnosis and management strategies employed for the treatment of DAVF. We also stress the importance of a timely diagnosis and its impact on patient outcomes and recovery.
- Citation: Gross R, Ali R, Kole M, Dorbeistein C, Jayaraman MV, Khan M. Tentorial dural arteriovenous fistula presenting as myelopathy: Case series and review of literature. World J Clin Cases 2014; 2(12): 907-911
- URL: https://www.wjgnet.com/2307-8960/full/v2/i12/907.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i12.907
Dural arteriovenous fistulas (DAVF) constitute 10% to 15% of all intracranial vascular malformations[1,2]. Tentorial DAVFs account for 8.4% of intracranial DAVFs[3]. Cranial dural arteriovenous fistulas may give rise to myelopathy due to spinal perimedullary venous drainage causing intramedullary venous hypertension[4]. However, this is very uncommon, with only 38 cases reported in the literature[5]. We describe two cases of tentorial dural AV fistulas causing significant myelopathy.
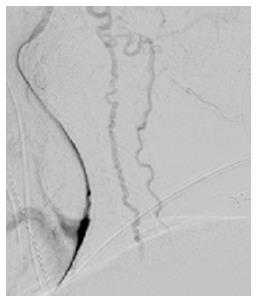
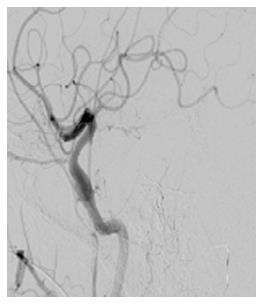
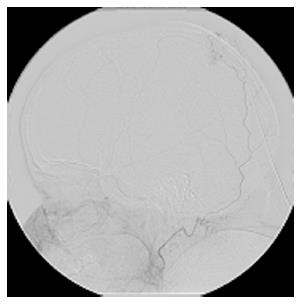
A 69-year-old male presented to our institution with 3 d of progressively worsening bilateral lower extremity weakness and urinary retention. These symptoms had been preceded by bilateral hand and forearm pain that lasted for 2 d. The patient was presumptively diagnosed with Guillian-Barre Syndrome and treatment started. Magnetic resonance imaging of the brain and of the cervical, thoracic, and lumbar spine showed increased T2/STIR signal intensity in the pons, medulla, and upper cervical spine and multiple small flow voids in the dorsal cervicothoracic spine suggestive of dural arteriovenous malformation (Figure 1). Neurological exam revealed significant weakness in bilateral lower extremities, most pronounced in bilateral hamstrings and in the left tibialis anterior. The upper extremity strength testing was normal. There were no sensory abnormalities. Deep tendon reflexes were increased in the lower extremities. This presentation was thought to be consistent with myelopathy from venous congestion related to a dAVF. He underwent angiography, which confirmed a Cognard V tentorial dAVF fed by the left middle meningeal, tentorial branch of the left ICA, and dural branches of the occipital and posterior auricular arteries, with drainage into cervical spinal veins (Figure 2). The AVF was successfully embolized with Onyx (Covidien Inc., Mansfield, MA) without any residual filling seen following embolization (Figure 3). The patient was discharged to rehab on hospital day 5. He was seen in follow-up 10 wk later, at which point he was noted to be walking independently, without urinary symptoms and only mild proximal lower extremity weakness bilaterally with manual muscle testing grade of 4 out of 5 in bilateral iliopsoas and hamstrings. The Aminoff-logue scale changed from 6 preintervention, to 1 after embolization of dural AV fistula.
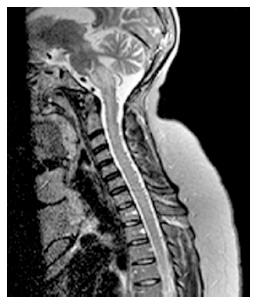
A 34-year old woman presented with progressively worsening bilateral upper and lower extremity weakness over 1 wk. Past medical history was significant for temporal pilocytic astrocytoma resection with subsequent whole brain radiation at age 12. Examination revealed quadriparesis and hyperreflexia in all 4 extremities. Initial presumptive diagnosis made was transverse myelitis with high cervical cord involvement, and the patient was started on steroid therapy. MRI Brain revealed dilated tortuous vessels posterior to the spinal cord between the foramen magnum and the upper thoracic spine. It also showed asymmetric expansion and T2/FLAIR signal abnormality of the left side of the brainstem at the cervicomedullary junction, as well as diffuse expansion and mild diffuse T2 signal abnormality within the cervical and upper thoracic spinal cord (Figure 4).
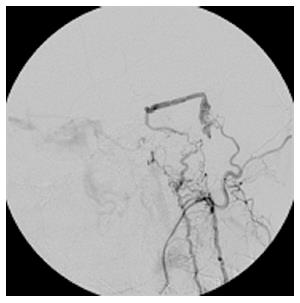
Cerebral angiogram showed a left transverse sigmoid junction dAVF fed by the left occipital artery (Figure 5). This fistula drained into the superior petrosal sinus, going to the tributaries of the petrosal vein and to the anterior medullary vein. From the anterior medullary vein it then drained down to the anterior spinal and cervicomedullary veins. This venous drainage was thought to be responsible for venous hypertension and the subsequent quadriparesis that the patient was experiencing. This DAVF was successfully embolized with Onyx (Covidien Inc., Mansfield, MA). Three month follow-up angiogram revealed no opacification of the fistula with left occipital artery injection (Figure 6). Clinically the patient had regained complete strength in all 4 extremities and was back at work performing manual labor. The Aminoff-logue scale changed from 7 preintervention, to 0 after embolization of dural AV fistula.
dAVFs are rare vascular lesions that can come to clinical attention as either intracranial hemorrhage (intraparenchymal, subarachnoid, subdural) or as a consequence of venous hypertension. In the latter situation, presenting symptoms are varied and can include pulsatile tinnitus, dementia, seizures, encephalopathy, parkinsonism, intracranial hypertension, and myelopathy[4]. Here we have presented two cases of rapidly progressive myelopathy related to dAVFs. All fistulas have one or more feeding arteries, derived from the dural arteries or meningeal branches of cerebral arteries, with venous drainage into a venous sinus, leptomeningeal, or spinal veins.
The classification of intracranial DAVFs has evolved over time, based on venous drainage, natural history, and arterial feeders. Cognard classification divides DAVFs in 5 types (I-V). This classification is based on the direction of dural sinus drainage (antegrade or retrograde), the presence or absence of cortical venous drainage, and venous outflow architecture (nonectactic cortical vein, ectactic cortical vein, or spinal perimedullary vein)[6,7]. The higher the type, the more likely the DAVF is to be symptomatic as a result of increased venous congestion. Both our cases were classified as Cognard Type V lesions. Type V DAVF usually have aggressive symptoms with progressive myelopathy due to spinal cord venous hypertension. The perimedullary venous drainage can extend down to the thoracic or lumbar levels.
The etiology of DAVFs is not entirely clear. It is generally accepted that DAVFs in adults are acquired. Trauma, prior surgery, sinus thrombosis, and stenosis have been proposed as possible etiologies[3,4,8,9]. An atypical presentation can lead to delays in accurate diagnosis, as clinicians may first think of other causes of rapidly progressive weakness, such as Guillian Barre syndrome and transverse myelitis. Both the cases we have presented were suspected to be suffering from similar neurological ailments. Only after failure to improve with standard therapy were further investigations conducted and the dAVF discovered on MRI imaging. This goes to underscore the importance of an accurate and timely diagnosis and the value of MRI in the acute setting since delayed diagnosis leads to grave neurologic and functional prognosis[10].
MRI findings can be subtle and difficult to interpret. These include prominent perimedullary flow voids as well as T2 signal intensity in the brainstem and spinal cord indicating the presence of venous congestion and edema. Diffuse signal change in the brainstem and spinal cord, with dilated perimedullary veins combined with a presentation of progressive myelopathy should always raise the suspicion of a DAVF[8]. Cerebral angiography is the gold standard for diagnosis. Arterial feeders to DAVFs can originate from branches of the external carotid artery such as the occipital artery, posterior meningeal artery, middle meningeal artery, as well as meningeal branches of pial arteries[9,11,12]. When the arterial phase of spinal angiography is negative, an extended observation of the venous phase should be performed looking for venous stagnation which is a sign of venous hypertension.
The optimal management strategy for DAVF is still controversial. It is recommended that DAVF be managed at a center with multidisciplinary experience in endovascular therapy, microsurgery and radiosurgery. Although both of our patients were successfully treated endovascularly, there is still a major role of conventional microsurgery in selected patients. Surgical therapy involves ligation and disruption of the arterio-venous fistulous connection, with success rates of 87.5% to 100% reported in literature[1-3,12]. Embolization with Onyx can be used as a first line therapy in many patients, with reportedly high rates of durable cure and low rates of complications[13,14]. There is some evidence to suggest that surgical ligation may offer permanent cure without any recurrence compared to endovascular therapy where recurrence may occur[15].
Endovascular and surgical therapies are associated with significantly improved symptoms once the definitive diagnosis of SDAVF is made, with studies showing significant improvement in patient outcomes measured on the Aminoff-Logue scale. The Aminoff-Logue scale is a disability scale comprising of three subcategories which score the patient on their gait, micturition and bowel control. Literature supports post-treatment improvement particularly in the subcategories of micturition and gait[16].
In conclusion, DAVFs are rare but aggressive and potentially fatal vascular malformations. Atypical presentation can mimic other more common neurologic disorders delaying diagnosis. Early diagnosis is important in these cases as a prompt intervention can result in great functional outcomes as evidenced by our cases.
The authors present two cases of dural arteriovenous fistula presenting as rapidly progressive myelopathy.
In one instance the patient demonstrated bilateral lower extremity weakness, whereas the second patient had quadparesis with significant weakness of all 4 extremities.
Differential diagnosis includes Guillian Barre syndrome, transverse myelitis and various other demyelinating illnesses.
MRI showed T2 signal change in the spinal cord as well as prominent dorsal flow voids. Cerebral angiogram showed the presence of a dural arteriovenous fistula in both cases.
Both patients were treated with Onyx embolization that resulted in complete resolution of the dural AV fistula.
This is an unusual presentation of tentorial dural AV fistulas which normally present as hemorrhage and not many cases have been reported in the literature.
Dural arteriovenous fistulas are abnormal connection between arteries within the dura mater and veins that normally drain brain tissue.
Dural AV fistulas are rare vascular lesions and can be classified using the Cognard classification. This case report highlights two cases of tentorial dural AV fistulas presenting as progressive myelopathy and discusses treatment options available.
Very interesting case reports. It is worth to publish.
P- Reviewer: Paholpak P S- Editor: Ji FF L- Editor: A E- Editor: Wu HL
| 1. | Kim MS, Han DH, Kwon OK, Oh CW, Han MH. Clinical characteristics of dural arteriovenous fistula. J Clin Neurosci. 2002;9:147-155. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 111] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Zhou LF, Chen L, Song DL, Gu YX, Leng B. Tentorial dural arteriovenous fistulas. Surg Neurol. 2007;67:472-481; discussion 481-482. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 47] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 3. | Awad EW, Anctil M. Positive coupling of beta-like adrenergic receptors with adenylate cyclase in the cnidarian Renilla koellikeri. J Exp Biol. 1993;182:131-146. [PubMed] |
| 4. | Khan S, Polston DW, Shields RW, Rasmussen P, Gupta R. Tentorial dural arteriovenous fistula presenting with quadriparesis: case report and review of the literature. J Stroke Cerebrovasc Dis. 2009;18:428-434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 12] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 5. | Renner C, Helm J, Roth H, Meixensberger J. Intracranial dural arteriovenous fistula associated with progressive cervical myelopathy and normal venous drainage of the thoracolumbar cord: case report and review of the literature. Surg Neurol. 2006;65:506-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 6. | Zipfel GJ, Shah MN, Refai D, Dacey RG, Derdeyn CP. Cranial dural arteriovenous fistulas: modification of angiographic classification scales based on new natural history data. Neurosurg Focus. 2009;26:E14. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 132] [Cited by in RCA: 126] [Article Influence: 7.9] [Reference Citation Analysis (0)] |
| 7. | Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, Chiras J, Merland JJ. Cerebral dural arteriovenous fistulas: clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995;194:671-680. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1138] [Cited by in RCA: 1044] [Article Influence: 34.8] [Reference Citation Analysis (0)] |
| 8. | Versari PP, D’Aliberti G, Talamonti G, Branca V, Boccardi E, Collice M. Progressive myelopathy caused by intracranial dural arteriovenous fistula: report of two cases and review of the literature. Neurosurgery. 1993;33:914-918; discussion 918-919. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Lewis AI, Tomsick TA, Tew JM. Management of tentorial dural arteriovenous malformations: transarterial embolization combined with stereotactic radiation or surgery. J Neurosurg. 1994;81:851-859. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 107] [Article Influence: 3.5] [Reference Citation Analysis (0)] |
| 10. | Iovtchev I, Hiller N, Ofran Y, Schwartz I, Cohen J, Rubin SA, Meiner Z. Late diagnosis of spinal dural arteriovenous fistulas resulting in severe lower-extremity weakness: a case series. Spine J. 2013;Oct 2; Epub ahead of print. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 32] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Gobin YP, Rogopoulos A, Aymard A, Khayata M, Reizine D, Chiras J, Merland JJ. Endovascular treatment of intracranial dural arteriovenous fistulas with spinal perimedullary venous drainage. J Neurosurg. 1992;77:718-723. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 71] [Cited by in RCA: 58] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Lawton MT, Sanchez-Mejia RO, Pham D, Tan J, Halbach VV. Tentorial dural arteriovenous fistulae: operative strategies and microsurgical results for six types. Neurosurgery. 2008;62:110-124; discussion 124-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 79] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 13. | Rangel-Castilla L, Barber SM, Klucznik R, Diaz O. Mid and long term outcomes of dural arteriovenous fistula endovascular management with Onyx. Experience of a single tertiary center. J Neurointerv Surg. 2014;6:607-613. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 38] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Natarajan SK, Ghodke B, Kim LJ, Hallam DK, Britz GW, Sekhar LN. Multimodality treatment of intracranial dural arteriovenous fistulas in the Onyx era: a single center experience. World Neurosurg. 2010;73:365-379. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 97] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 15. | Gokhale S, Khan SA, McDonagh DL, Britz G. Comparison of surgical and endovascular approach in management of spinal dural arteriovenous fistulas: A single center experience of 27 patients. Surg Neurol Int. 2014;5:7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 48] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 16. | Narvid J, Hetts SW, Larsen D, Neuhaus J, Singh TP, McSwain H, Lawton MT, Dowd CF, Higashida RT, Halbach VV. Spinal dural arteriovenous fistulae: clinical features and long-term results. Neurosurgery. 2008;62:159-166; discussion 166-167. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 136] [Cited by in RCA: 144] [Article Influence: 8.5] [Reference Citation Analysis (0)] |