Published online Dec 16, 2014. doi: 10.12998/wjcc.v2.i12.903
Revised: August 17, 2014
Accepted: September 29, 2014
Published online: December 16, 2014
Processing time: 68 Days and 5.2 Hours
Cecal bascule is a rare cause of bowel obstruction in which a mobile cecum folds anteriorly and superiorly over the ascending colon. Herein, we present the first case of internal herniation of a cecal bascule into the lesser sac through the foramen of winslow, aiming at discussing radiological findings, differential diagnosis, and surgical management of this uncommon condition. A 75-year-old female presented to the emergency room with an 18-h history of sudden onset sharp, progressively worsening abdominal pain associated with vomiting. Physical exam revealed abdominal distention and epigastric tenderness while initial laboratory tests were unremarkable. Computed tomography of her abdomen and pelvis showed a loop of distended colon within lesser sac without signs of bowel ischemia or perforation. On exploratory laparotomy, a cecal bascule was found herniating into lesser sac via foramen of winslow. Upon reduction, the cecum appeared viable therefore a cecopexy was performed without bowel resection. Unlike cecal volvulus, cecal bascule consists of no axial rotation of the bowel with no mesenteric vascular compromise and therefore ischemia would only occur from intraluminal tension or extraluminal compression from the borders of foramen of winslow. The management of internal herniation of a cecal bascule is always surgical including anatomic resection or cecopexy.
Core tip: Cecal bascule is a rare and overlooked cause of large bowel obstruction in which a mobile cecum folds anteriorly and superiorly leading to obstruction of ascending colon. Although cecal bascule has been described in association with mechanical bowel obstruction in the literature, its association with this type of internal hernia has never been described before. The management of internal herniation of a cecal bascule is always surgical even in the absence of peritonitis, either cecopexy or right hemicolectomy depending on the viability of the bowel segment involved.
- Citation: Makarawo T, Macedo FI, Jacobs MJ. Cecal bascule herniation into the lesser sac. World J Clin Cases 2014; 2(12): 903-906
- URL: https://www.wjgnet.com/2307-8960/full/v2/i12/903.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i12.903
Cecal bascule is an extremely rare condition in which the bowel folds anteriorly and superiorly over the ascending colon[1]. Its similarity with cecal volvulus has led to misdiagnosis, although the absence of axial rotation of the bowel in cecal bascule is an importance difference that influences presentation. In cecal bascule, patients usually present with less critical illness than those with cecal volvulus as there is no torsion of the mesenteric vasculature[2]. Symptoms are therefore mostly related to bowel obstruction, particularly in the presence of a functional ileocecal valve causing a closed-loop obstruction. Diagnosis is often challenging because of equivocal image findings in addition to its rare occurrence. We, herein, present a rare case of cecal bascule herniating into the lesser sac in a patient with obstructive signs, and discuss the diagnosis, and operative management of this rare condition.
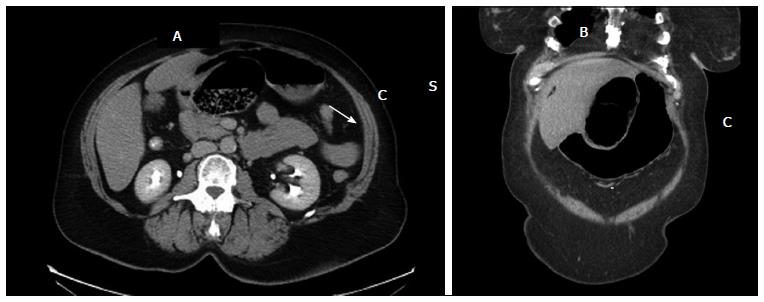
A 75-year-old female presented to the emergency room with an 18-h history of sudden onset, progressively worsening abdominal pain associated with vomiting. The patient had a previous history of hiatal hernia with gastroesophageal reflux symptoms and previous hysterectomy and tonsillectomy. The patient presented with abdominal distention and epigastric tenderness without diffuse peritoneal signs. Laboratory tests were unremarkable, with no leukocytosis but computed tomography (CT) of the abdomen and pelvis showed a loop of distended colon within lesser sac with no signs of bowel ischemia or perforation (Figure 1).
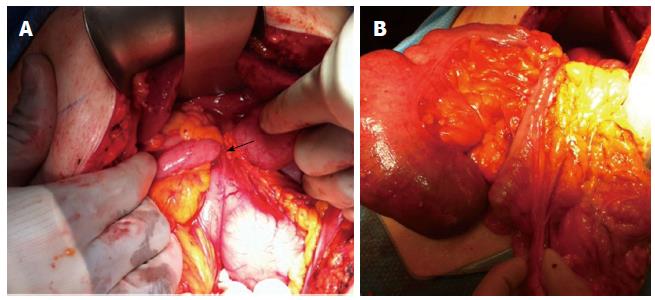
The patient underwent exploratory laparotomy during which the cecum was noted to be folded anteriorly over the ascending colon and herniating into lesser sac via the foramen of winslow (Figure 2A) resulting in colonic obstruction. To reduce the internal hernia, the lesser omentum was incised revealing the absence of underlying adhesive bands tethering the cecum in place, hence allowing the gentle withdrawal of the bowel back through foramen of winslow. Upon reduction, the cecum and terminal ileum appeared viable (Figure 2B). Therefore, lysis of a single adhesive band to the terminal ileum was performed prior to cecopexy with fixation of the cecum inferolaterally to the right lateral abdominal wall, negating the need for bowel resection.
The patient made an uneventful post-operative recovery, tolerating full oral intake within 48 h of the surgery and being discharged on post-operative day four. The patient has had no further episodes of bowel obstruction, remaining symptom-free after almost a year of follow-up.
Cecal bascule is a rare and overlooked cause of large bowel obstruction in which a mobile cecum folds anteriorly and superiorly leading to obstruction of ascending colon. It has been estimated that approximately 10% to 15% of labeled “cecal volvulus” episodes were actually cecal bascules[3]. The formation of a cecal bascule is secondary to hypermobility of the cecum and intestinal distention[4,5]. This excessive mobility can occur as a result of defective retroperitoneal fixation of the cecum due to incomplete intestinal rotation during embryogenesis, or the persistence of ascending mesocolon. It may also occur postoperatively after dissection of peritoneal attachments[6]. The formation of adhesions may also play a role by creating a point of fixation, allowing the formation of the bascule.
The clinical presentation of cecal bascule is usually similar to postoperative ileus including nausea, vomiting and abdominal distention and pain. However, unlike in cecal volvulus, the patients are not as critically ill because there is no axial torsion of the mesenteric vasculature, which leads to bowel ischemia. However, it must be noted that delay in diagnosis with unrelieved bowel obstruction causing increased intraluminal tension or extraluminal compression from an internal hernia would ultimately result in bowel ischemia and eventual perforation. Diagnosis is often challenging due to its rare nature. Plain abdominal X-rays may show a dilated cecum in the right upper quadrant with or without small bowel obstruction. CT scan of the abdomen, which is more helpful, may demonstrate a dilated cecum anterior to the ascending colon and an ileocecal valve located in the right upper quadrant[4]. In our case, the CT scan did show an internal hernia containing a loop of distended colon within lesser sac, although it was unclear whether it was transverse colon or ascending colon that had herniated through the foramen of winslow.
Herniation of abdominal viscera through the foramen of winslow into the lesser sac occurs rarely, accounting for 8% of all internal hernias[7]. Hernias through this foramen have been described as containing small bowel, right colon, and rarely, gallbladder or transverse colon. Potential predisposing factors include hypermobile mesentery, enlargement of the foramen of winslow, or absence of fusion of the ascending colon to the posterior abdominal wall[7,8]. Although cecal bascule has been described in association with mechanical bowel obstruction in literature, its association with this type of internal hernia has never been described before[8-14]. Indeed, it is possible that the term ‘bascule’ which is derived from a French word meaning “a bridge with a movable section hinged about a horizontal axis”, is not widely applied, and therefore underdiagnosed as a cause for cecal herniation.
The management of bowel obstruction secondary to cecal bascule should be surgical. In this case, simple reduction and cecopexy was technically feasible, safe, and had a satisfactory outcome. Although right hemicolectomy has also been advocated even with the cecum being viable to prevent recurrence[9], there are no reported cases of recurrence of cecal bascule following cecopexy only[10-12]. Therefore, we would recommend that segmental resection be reserved for cases with associated ischemia or perforation. Closure of the foramen has also not been advocated due increased risk of portal vein thrombosis or hepatic artery and/or bile ducts injury[13,14].
In conclusion, we presented a rare case of an internal hernia containing a cecal bascule into the lesser sac through the foramen of winslow. Despite its rare occurrence, cecal bascule should be in the differential diagnosis armamentarium of bowel obstruction, especially in patients with a markedly distended cecum in the absence of peritoneal signs. The management of internal herniation of a cecal bascule is always surgical even in the absence of peritonitis, and includes either cecopexy if the cecum is viable or right hemicolectomy if it appears ischemic or non-viable.
A 75-year-old female presented to the emergency room with an 18-h history of sudden onset, progressively worsening abdominal pain associated with vomiting.
On physical examination, she had abdominal distention and epigastric tenderness without diffuse peritoneal signs.
Mechanical obstruction due to adhesions, ileus, cecal volvulus, cecal bascule.
Computed tomography of abdomen and pelvis showing a loop of distended colon within lesser sac without bowel ischemia or perforation.
The patient underwent exploratory laparotomy, reduction of cecal herniation into the lesser omentum and cecopexy.
Cecal bascule occurs when a mobile cecum folds anteriorly and superiorly leading to obstruction of ascending colon. The term “bascule” is derived from a French word meaning “a bridge with a movable section hinged about a horizontal axis”, is not widely applied, and therefore may be underdiagnosed.
This is the first case in the literature describing a hernia into the lesser sac from a cecal bascule. The management of bowel obstruction secondary to cecal bascule should be surgical.
This manuscript highlights the clinical presentation of a rare cause of large bowel obstruction and provides insights into the management of cecal bascule.
P- Reviewer: Bjornsson B, Dhiman RK, Fabozzi M S- Editor: Ma YJ L- Editor: A E- Editor: Wu HL
| 1. | Bobroff LM, Messinger NH, Subbarao K, Beneventano TC. The cecal bascule. Am J Roentgenol Radium Ther Nucl Med. 1972;115:249-252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 34] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 2. | Consorti ET, Liu TH. Diagnosis and treatment of caecal volvulus. Postgrad Med J. 2005;81:772-776. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 109] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Madiba TE, Thomson SR. The management of cecal volvulus. Dis Colon Rectum. 2002;45:264-267. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 120] [Cited by in RCA: 114] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 4. | Lazar DA, Cohen SA, Evora DK, Losasso BE, Bickler SW. Cecal bascule in a child: an unusual cause of postoperative bowel obstruction. J Pediatr Surg. 2012;47:609-611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 14] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Rozycki GS. Special feature: Image of the month. Cecal bascule. Arch Surg. 2001;136:835-836. [PubMed] |
| 6. | Kim J, Nguyen S, Leung P, Divino C. Cecal bascule after laparoscopic ventral hernia repair. JSLS. 2013;17:484-486. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 10] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 7. | Da Costa G, Ng B, Kociumbas I, Wong S. Herniation of caecum through the foramen of Winslow. Australas Radiol. 2007;51 Spec No:B152-B154. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Erskine JM. Hernia through the foramen of Winslow. Surg Gynecol Obstet. 1967;125:1093-1109. [PubMed] |
| 9. | Samson TD, Tercero FM, Sato K, Awad ZT, Filipi CJ. Cecal herniation through the foramen of Winslow after laparoscopic Nissen fundoplication. Surg Endosc. 2001;15:1490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 10. | Cohen DJ, Schoolnik ML. Herniation through the foramen of Winslow. Dis Colon Rectum. 1982;25:820-822. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 14] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 11. | Evrard V, Vielle G, Buyck A, Merchez M. Herniation through the foramen of Winslow. Report of two cases. Dis Colon Rectum. 1996;39:1055-1057. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Puig CA, Lillegard JB, Fisher JE, Schiller HJ. Hernia of cecum and ascending colon through the foramen of Winslow. Int J Surg Case Rep. 2013;4:879-881. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 26] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 13. | Tjandra JJ, Collier N. Obstructive jaundice due to foramen of Winslow hernia: a case report. Aust N Z J Surg. 1991;61:467-469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 15] [Article Influence: 0.4] [Reference Citation Analysis (0)] |