Published online Oct 16, 2014. doi: 10.12998/wjcc.v2.i10.604
Revised: June 14, 2014
Accepted: July 25, 2014
Published online: October 16, 2014
Processing time: 240 Days and 17.6 Hours
Pyogenic liver abscess is a common entity in Indian subcontinent and is mostly caused by gram negative bacteria. Melioidosis is not commonly seen in India and only a few cases are reported. It can give rise to multiple abscesses at different sites including liver. We report a case of isolated liver abscess caused by Burkholderia pseudomallei (B. pseudomallei) in a 29-year-old recently diagnosed diabetic, immunocompetent male. Diagnosis was made by imaging and culture of pus aspirated from the abscess and he was treated with percutaneous pigtail catheter drainage followed by antibiotics (meropenem and trimethoprim-sulphmethoxazole). Melioidosis is an emerging infection in India and has high mortality rate, so early diagnosis and prompt management is warranted which requires clinical vigilance and an intensive microbiological workup. Clinicians should be aware of isolated liver abscess caused by B. pseudomallei in appropriate clinical settings.
Core tip: Liver abscess due to Burkholderia pseudomallei (B. pseudomallei) is extremely rare and is mostly reported from Taiwan. In India, most of the reports of are from southern coastal India and this entity is exceedingly rare in eastern India. The actual magnitude of this emerging infection may be under reported due to non-availability of confirmatory tests. Accurate diagnosis is necessary as outcome is fatal with ineffective treatment. We report a case of multiple liver abscesses caused by B. pseudomallei in a 29-year-old diabetic male, who was referred as a case of recurrence of pyogenic liver abscess which was previously caused by pseudomonas not responding to antibiotic therapy and aspiration. Diagnosis was made by imaging and culture of aspirated pus revealed B. pseudomallei and he was treated successfully with surgical drainage and prolonged course of intravenous and oral antibiotics. So, in a case of pyogenic liver abscess not responding to conventional antibiotics, B. pseudomallei should always be thought as a possibility which can be identified by its characteristic appearance on culture and microscopy or direct immunofluorescence testing as well as unique imaging features.
-
Citation: Pal P, Ray S, Moulick A, Dey S, Jana A, Banerjee K. Liver abscess caused by
Burkholderia pseudomallei in a young man: A case report and review of literature. World J Clin Cases 2014; 2(10): 604-607 - URL: https://www.wjgnet.com/2307-8960/full/v2/i10/604.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v2.i10.604
Liver abscess is the commonest intra-abdominal abscess, which may be of biliary tract origin (commonest) or hematogenous spread from a distant site, and rarely traumatic. Pyogenic liver abscess is a rare but potentially lethal condition, with a reported incidence of 20 per 100000 hospital admissions in a western population[1]. Both gram positive and gram negative aerobes and anaerobes have been found on culture of aspirated pus, among them Escherichia coli (E. coli) is cultured most frequently in Western countries[2] and Klebsiella in Asian countries[3].
Burkholderia pseudomallei (B. pseudomallei), a category II bioterrorism agent, is the causative organism melioidosis and is endemic in Southeast Asia and northern Australia[4]. B. pseudomallei is found in soil and water and infection occurs by inoculation, inhalation, or ingestion[4]. Melioidosis is most commonly known to present as pneumonia followed by abscesses in the skin. Abscesses in internal organs like spleen, kidney, prostate and liver have also been reported as part of disseminated disease. Isolated liver abscess in melioidosis is a rare clinical condition.
Cases of melioidosis have been reported from southern coastal part of India, but melioidosis causing liver abscess is rare. In cases of liver abscess not responding to conventional anti-microbial the possibility of melioidosis should always be kept in mind. Because of high relapse and mortality rate, early diagnosis and prolonged treatment is a must in this case.
A 29-year-old male was referred to us with high grade fever for 20 d and cough for 2 wk. He had no history of tuberculosis, foreign travel or animal exposure and is farmer by occupation. He had a pyogenic liver abscess by Pseudomonas aeruginosa along with pancytopenia about one year back. On admission patient was toxic with high grade fever (37.7 °C-39.4 °C) with a pulse rate of 126/min and blood pressure of 100/76 mmHg. Liver was enlarged, tender with a liver span of 15 cm and spleen was just palpable. There was no free fluid in abdomen clinically.
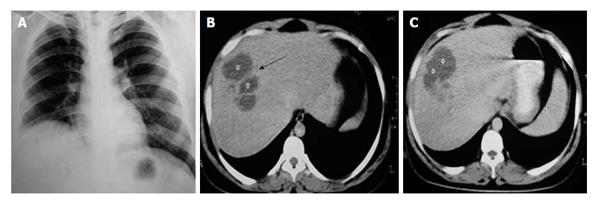
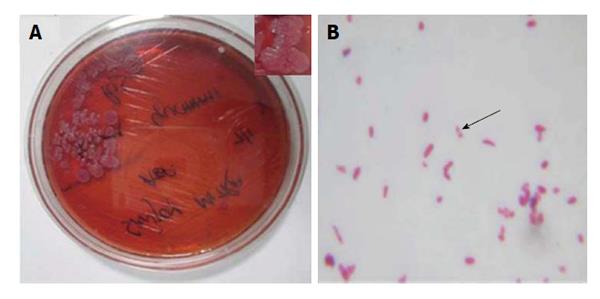
Investigations revealed hemoglobin 10.3 gm/dL, total leucocyte count of 9400/μL, neutrophil 88%, lymphocyte 10%, eosinophil 2% and platelet count of 175 × 109/μL. Fasting plasma glucose was 164 mg/dL and HbA1c was 8.1%. So he was newly diagnosed of having diabetes mellitus and started on treatment with insulin. Renal function and liver function tests were within normal limits. Human immunodeficiency virus serology was negative. Acid fast bacilli were not found in sputum and sputum culture showed no growth of any pathogenic organism. Chest radiograph showed elevation of right dome of diaphragm (Figure 1A). Abdominal ultrasound revealed hepatomegaly with a large hypoechoic space occupying lesion (88 mm × 91 mm) in right lobe of liver with splenomegaly. Contrast enhanced computed tomography of abdomen showed hepatomegaly with loculated hypodense lesion (8.5 cm × 7.4 cm) in the anterior part of right lobe (Figure 1B), and multiple small hypodense lesions with confluence in the posterior part of right lobe (Figure 1C). Pus was aspirated from the abscess which on culture showed dry, wrinkled colonies (Figure 2A) on 5% sheep blood agar and McConkey’s agar after 48 h of incubation at 37 °C. Gram-negative, oxidase-positive, motile, aerobic bacilli with typical bipolar “Safety pin” appearance (Figure 2B) was seen on gram stain suggestive of B. pseudomallei, which was identified by Vitek 2 compact system. Culture sensitivity was done, which was sensitive to ceftazidime, piperacillin-tazobactum, meropenem, trimethoprim-sulphmethoxazole and minocycline.
Patient was treated with percutaneous catheter drainage, antibiotics and strict glycemic control. Intravenous meropenem was continued for two weeks followed by trimethoprim-sulphmethoxazole for 20 wk after which follow up computed tomography (CT) scan showed complete resolution of the liver abscess.
Liver abscess is a common entity in India; among which pyogenic liver abscess is a rare variety. Ascending infection from biliary tract is the most common cause, followed by hematogenous spread[4]. E. coli, is the most often cultured bacteria, accounting for about 33% of the cases followed by streptococcal group[5].
Melioidosis varies from asymptomatic infections and localized skin abscess without systemic illness to fulminant diseases with abscesses involving lungs and other internal organs especially when the host immunity is compromised. Cases of isolated liver abscess are not very common and rarely reported. It is an environmental saprophyte and is endemic in Southeast Asia and northern Australia. In India it is found in southern parts in the states of Karnataka, Tamil Nadu, Kerala and Maharastra[6]. Twenty eight cases of septicemic melioidosis were reported from a tertiary care hospital in south India between 1993 and 2002[7] and it is an emerging infection in India. Liver abscess caused by B. pseudomallei is rare and only 9 cases have been reported in India[6,8-10] till now, and few cases have been reported in Taiwan[11-13]. Gopalakrishnan et al[14], in a series of 32 cases of culture proven Melioidosis found localized infections in 14 patients but did not encounter even a single case of liver abscess.
The most important risk factors are diabetes, renal disease, liver cirrhosis, thalassemia, alcoholism, use of immunosuppressive agents, cystic fibrosis and kava (a Hawaiian drink) consumption[15]. The presenting symptoms may vary from fever, dry cough due to irritation of diaphragm by abscess, abdominal pain, localized swelling to septicemia shock. Lung is most commonly involved in melioidosis. Abscess in other internal organs such as liver and spleen may be a presenting feature in an immunocompromised host. The risk factor for our patient was diabetes but isolated liver abscess without any other organ involvement has seldom been reported previously.
A positive culture of B. pseudomallei from the aspirated pus from liver abscess is the definitive diagnosis. It is difficult to differentiate B. pseudomallei from other gram negative bacilli. Direct immunofluorescence microscopy is 98% specific and 70% sensitive compared to culture[7]. Chest radiograph may show elevation of right dome of diaphragm as in our case. CT scan findings will include liver abscesses with a “honeycomb” pattern of multiseptate, multiloculated lesions and a “necklace sign” with multiple peripheral radial loculations contained within the larger hypodense honeycomb lesions[16]. These findings were shown in a retrospective study in a small number of cases of liver abscess with melioidosis.
B. pseudomallei is characteristically resistant to penicillin other than ureidopenicillins, ampicillin, first- and second-generation cephalosporins, gentamicin, tobramycin, streptomycin and macrolides. It is only susceptible to chloramphenicol, tetracyclines, trimethoprim-sulfamethoxazole, ureidopenicillins, third-generation cephalosporins, carbapenems and amoxicillin-clavulanate[14]. The antibiotic of choice for melioidosis is ceftazidime (40 mg/kg every 8 h)[17]. Imipenem or intravenous amoxicillin-clavulanate is the alternative choices[18]. Parenteral antibiotics should be continued for at least 10-14 d, or until patient is able to take oral medications. Oral maintenance therapy for at least 20 wk with amoxicillin-clavulanate (amoxicillin 27 mg/kg per day divided into three doses) or trimethoprim-sulfamethoxazole (trimethoprim 8 mg/kg per day and sulfamethoxazole 40 mg/kg per day) should be given in patients with abscess for complete resolution[14]. Patients need to be followed up for at least 6 mo after complete resolution of abscess.
In conclusion, E. coli is the commonest cause of pyogenic liver abscess in India, but B. pseudomallei should also be kept in mind because of its rising incidence and misdiagnosis can lead to treatment failure and high mortality rate. Diabetes and immunosuppressed state are the important risk factors. Prolonged treatment with antibiotic is necessary for complete resolution in B. pseudomallei liver abscess. Liver abscess in a diabetic not responding to aminoglycosides and penicillins should be dealt with rigorous attention or otherwise the outcome will be fatal.
A 29-year-old farmer presented with high grade fever and cough for 3 wk.
High grade pyrexia, tachycardia, just palpable splenomegaly and tender hepatomegaly.
An infectious etiology common in tropical countries such as pyogenic liver abscess, malaria, tuberculosis and an immunocompromised state [e.g., human immunodeficiency virus (HIV)] have been considered.
Mild anemia, neutrophilia, fasting hyperglycemia, raised glycosylated hemoglobin was present whereas sputum for Acid-fast bacilli, HIV serology, blood for malaria parasite were negative.
Chest X-ray, abdominal ultrasound and abdominal contrast enhanced computed tomography were done which showed elevated hemidiaphragm on X-ray and hypodense loculated lesion in right lobe of liver on ultrasound and tomography.
Aspirated pus from the abscess inoculated on 5% sheep blood agar and McConkey’s agar showed gram-negative, oxidase-positive, motile, aerobic bacilli with typical bipolar “Safety pin” appearance on gram stain suggestive of Burkholderia pseudomallei (B. Pseudomallei), later confirmed via automated Vitek-2 compact system and was sensitive to ceftazidime, piperacillin-tazobactum, meropenem, trimethoprim-sulphmethoxazole and minocycline.
Patient was treated with percutaneous catheter drainage, strict glycemic control with insulin, intravenous meropenem for 2 wk followed by trimethoprim-sulphmethoxazole for 20 wk which led to resolution of abscess.
“Safety Pin” appearance: bipolar staining of B. Pseudomallei on gram stain as if the organism resembles a “Safety Pin”, “Necklace sign” on computed tomography scan: multiple peripheral radial loculations contained within the larger hypodense honeycomb lesions of liver abscess.
Isolated liver abscess due to B. Pseudomallei can occur specially in immunosuppressed and diabetic patients who need prolonged treatment with antibiotics for resolution and misdiagnosis may lead to treatment failure and high mortality rates.
This paper is interesting and it could be accepted pending review.
P- Reviewer: Ferraioli G S- Editor: Song XX L- Editor: A E- Editor: Liu SQ
| 1. | Huang CJ, Pitt HA, Lipsett PA, Osterman FA, Lillemoe KD, Cameron JL, Zuidema GD. Pyogenic hepatic abscess. Changing trends over 42 years. Ann Surg. 1996;223:600-607; discussion 607-609. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 369] [Cited by in RCA: 326] [Article Influence: 11.2] [Reference Citation Analysis (1)] |
| 2. | Alvarez Pérez JA, González JJ, Baldonedo RF, Sanz L, Carreño G, Junco A, Rodríguez JI, Martínez MD, Jorge JI. Clinical course, treatment, and multivariate analysis of risk factors for pyogenic liver abscess. Am J Surg. 2001;181:177-186. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 159] [Cited by in RCA: 136] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 3. | Chou FF, Sheen-Chen SM, Chen YS, Chen MC. Single and multiple pyogenic liver abscesses: clinical course, etiology, and results of treatment. World J Surg. 1997;21:384-388; discussion 388-389. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 109] [Cited by in RCA: 78] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 4. | Ramphal R. Chapter 152. Infections Due to Pseudomonas Species and Related Organisms. Harrison’s Principles of Internal Medicine. 18th ed. New York: McGraw-Hill 2012; . |
| 5. | Branum GD, Tyson GS, Branum MA, Meyers WC. Hepatic abscess. Changes in etiology, diagnosis, and management. Ann Surg. 1990;212:655-662. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 149] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 6. | Mukhopadhya A, Balaji V, Jesudason MV, Amte A, Jeyamani R, Kurian G. Isolated liver abscesses in melioidosis. Indian J Med Microbiol. 2007;25:150-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 7. | Jesudason MV, Anbarasu A, John TJ. Septicaemic melioidosis in a tertiary care hospital in south India. Indian J Med Res. 2003;117:119-121. [PubMed] |
| 8. | Banerjee S. Liver abscess due to unusual gram negative bacilli; Burkholderia pseudomallei? IJM. 2009;6. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 9. | Sengupta S, Murthy R, Kumari GR, Rahana K, Vidhyasagar S, Bhat BKS, Shivananda PG. Burkholderia pseudomallei in a case of hepatic abscess. Indian J Med Microbiol. 1998;16:88-89. |
| 10. | Saravu K, Mukhopadhyay C, Vishwanath S, Valsalan R, Docherla M, Vandana KE, Shastry BA, Bairy I, Rao SP. Melioidosis in southern India: epidemiological and clinical profile. Southeast Asian J Trop Med Public Health. 2010;41:401-409. [PubMed] |
| 11. | Lee YL, Lee SS, Tsai HC, Chen YS, Wann SR, Kao CH, Liu YC. Pyogenic liver abscess caused by Burkholderia pseudomallei in Taiwan. J Formos Med Assoc. 2006;105:689-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Wang CZ, Hung MZ. [Liver melioidosis: case report and literature review]. Taiwan Med J. 2004;47:32-34. |
| 13. | Ben RJ, Tsai YY, Chen JC, Feng NH. Non-septicemic Burkholderia pseudomallei liver abscess in a young man. J Microbiol Immunol Infect. 2004;37:254-257. |
| 14. | Gopalakrishnan R, Sureshkumar D, Thirunarayan MA, Ramasubramanian M. Melioidosis: An Emerging Infection in India. J Assoc Physicians India. 2013;61:612-14. |
| 15. | White NJ. Melioidosis. Lancet. 2003;361:1715-1722. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 657] [Cited by in RCA: 642] [Article Influence: 29.2] [Reference Citation Analysis (0)] |
| 16. | Apisarnthanarak A, Apisarnthanarak P, Mundy LM. Computed tomography characteristics of Burkholderia pseudomallei liver abscess. Clin Infect Dis. 2006;42:989-993. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 17] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 17. | White NJ, Dance DA, Chaowagul W, Wattanagoon Y, Wuthiekanun V, Pitakwatchara N. Halving of mortality of severe melioidosis by ceftazidime. Lancet. 1989;2:697-701. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 230] [Article Influence: 6.4] [Reference Citation Analysis (0)] |
| 18. | Smith MD, Wuthiekanun V, Walsh AL, White NJ. Susceptibility of Pseudomonas pseudomallei to some newer beta-lactam antibiotics and antibiotic combinations using time-kill studies. J Antimicrob Chemother. 1994;33:145-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 29] [Article Influence: 0.9] [Reference Citation Analysis (0)] |