Published online Mar 26, 2025. doi: 10.12998/wjcc.v13.i9.99964
Revised: October 18, 2024
Accepted: December 2, 2024
Published online: March 26, 2025
Processing time: 130 Days and 1.9 Hours
Acinic cell carcinoma (ACC) is a malignant epithelial neoplasm that commonly occurs in the parotid gland. It is known to have a high recurrence rate and the potential to metastasize to the lung or cervical lymph nodes. However, few cases of ACC with bone metastasis have been reported in the medical literature.
The clinical significance of this case report lies in the unique site of occurrence of the metastasis: To the best of our knowledge, this report is the only literature documenting ACC arising in a shoulder mass.
Unusual presentations of uncommon malignancies can present diagnostic challenges for both surgeons and histopathologists. It is important to be aware of these rare occurrences in order to provide the best possible treatment for patients.
Core Tip: Metastatic acinic cell carcinoma of the parotid gland spreading to the scapular region is an exceedingly rare occurrence, and the mechanisms and clinical implications of such metastasis remain unclear. This case stands out for its uniqueness and provides a valuable opportunity for further research, offering insights into the metastatic pathways and prognostic factors associated with acinic cell carcinoma of the parotid gland.
- Citation: Sun DQ, Chen CC, Zheng DA, Xing HY, Peng X. Scapular metastasis from acinic cell carcinoma of parotid gland: A case report. World J Clin Cases 2025; 13(9): 99964
- URL: https://www.wjgnet.com/2307-8960/full/v13/i9/99964.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i9.99964
The majority of minor salivary glands are found in the oral cavity. According to Spiro[1], the oral cavity is the most common site, accounting for 70.1%, followed by the nose and paranasal sinuses, accounting for 26.8%. Acinic cell carcinoma (ACC), a type of malignant epithelial neoplasm, tends to occur in the parotid gland and typically presents in the 5th decade of life, showing a predilection for women[2]. The appearance of a shoulder mass is often considered as lymph node enlargement, and a small proportion may consider malignant tumor bone metastasis[3]. However, salivary gland tumors often experience lymph node metastasis and rarely bone metastasis[4]. Therefore, they are clinically unsuspected in the initial evaluation of a patient presenting with a shoulder mass. The clinical data concerning ACC of the tract is very limited compared to other more common histological types. Consequently, the clinical course, optimal treatment, and prognosis have not been extensively studied. Among the few reported cases of scapular metastases arising from the salivary glands, the scapular region is an extremely rare malignant neoplasm, and to the best of our knowledge, an unknown cause of scapular metastases.
This case report presents the diagnostic and treatment process of a patient with a lump in the scapular region. Initially, the patient underwent ultrasound and magnetic resonance imaging, which revealed a mass in the scapular region. As a result, there was a suspicion of giant cell tumor of bone. However, subsequent histopathological examination of the mass indicated an epithelial origin. Further pathological analysis confirmed the diagnosis of metastatic ACC originating from the parotid gland. Upon reviewing the patient’s medical history, it was discovered that the patient had previously undergone surgical excision of a facial mass five years ago, providing a clue to the metastasis of the ACC[5]. Through a comprehensive description of the clinical features, diagnostic process, and treatment plan of this case, we aim to underscore the significance of thorough patient history taking, early diagnosis, and comprehensive treatment for individuals with ACC of the parotid gland. Furthermore, we propose further research endeavors to explore similar cases, deepening our understanding of the metastasis of ACC from the parotid gland to the scapular region. This research can help in developing more effective strategies for prevention and treatment, ultimately leading to improved patient prognosis and survival rates.
A 51-year-old male presented with a one-year history of localized slow-growing mass in the left scapular region, without a previous history of lesion at the same site.
The mass had recently increased in size, causing severe pain, worse with shoulder abduction.
No history of shoulder trauma, or lipomyoma was given.
The patient’s medical and family history were non-contributory.
On physical examination, the patient was afebrile and a large, tough, soft tissue mass was present.
The patient had no laboratory tests done.
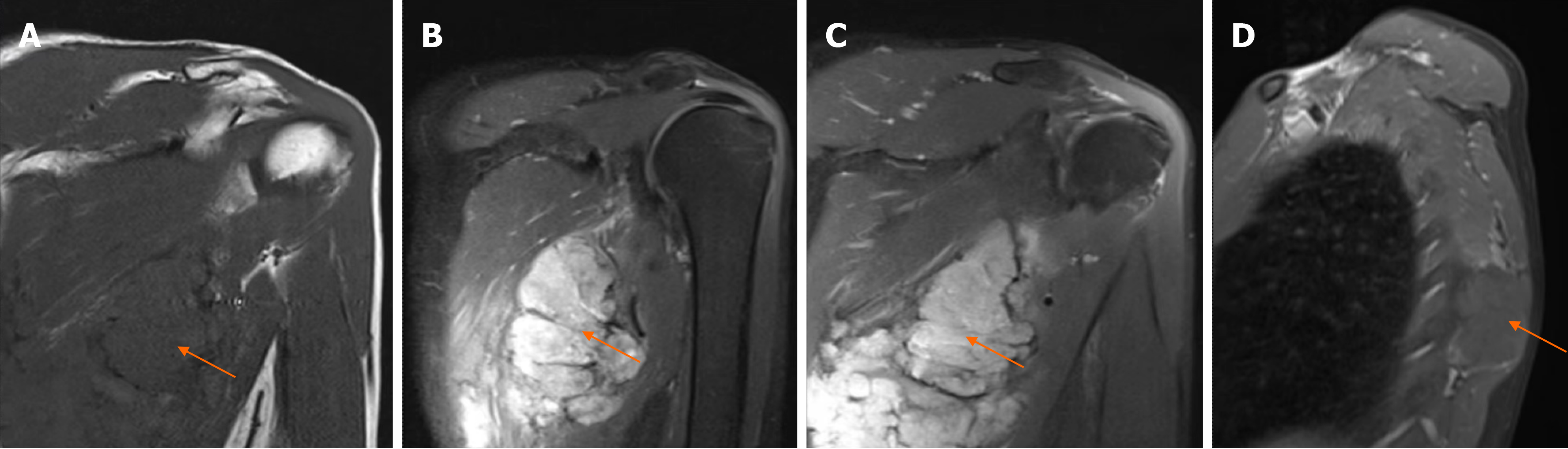
Ultrasonography was initially performed, sonogram of the left shoulder mass with Doppler, demonstrating numerous large soft tissue structures. Subsequently the patient was investigated with a left scapular and chest computed tomography scan. The results showed abnormal bone morphology and density, but there was no evidence of erosion of the adjacent bone or any lymph node enlargement. The magnetic resonance examination results consider the high possibility of bone giant cell tumor (Figure 1).
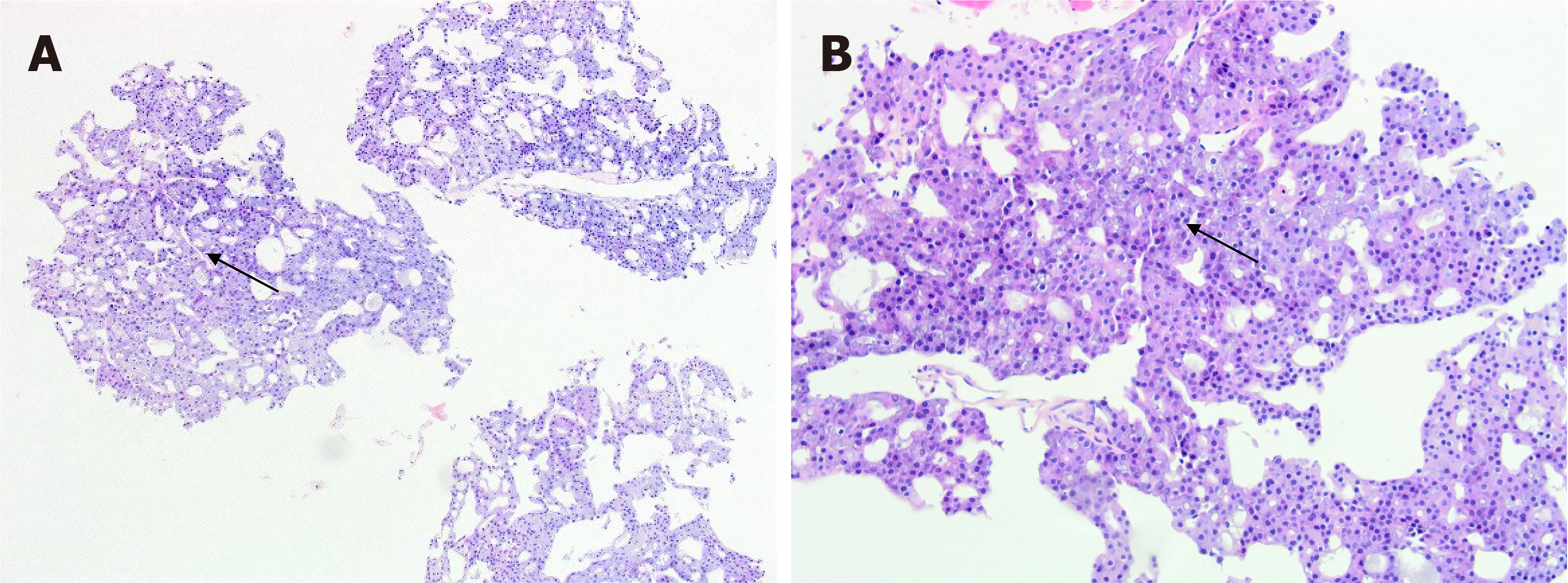
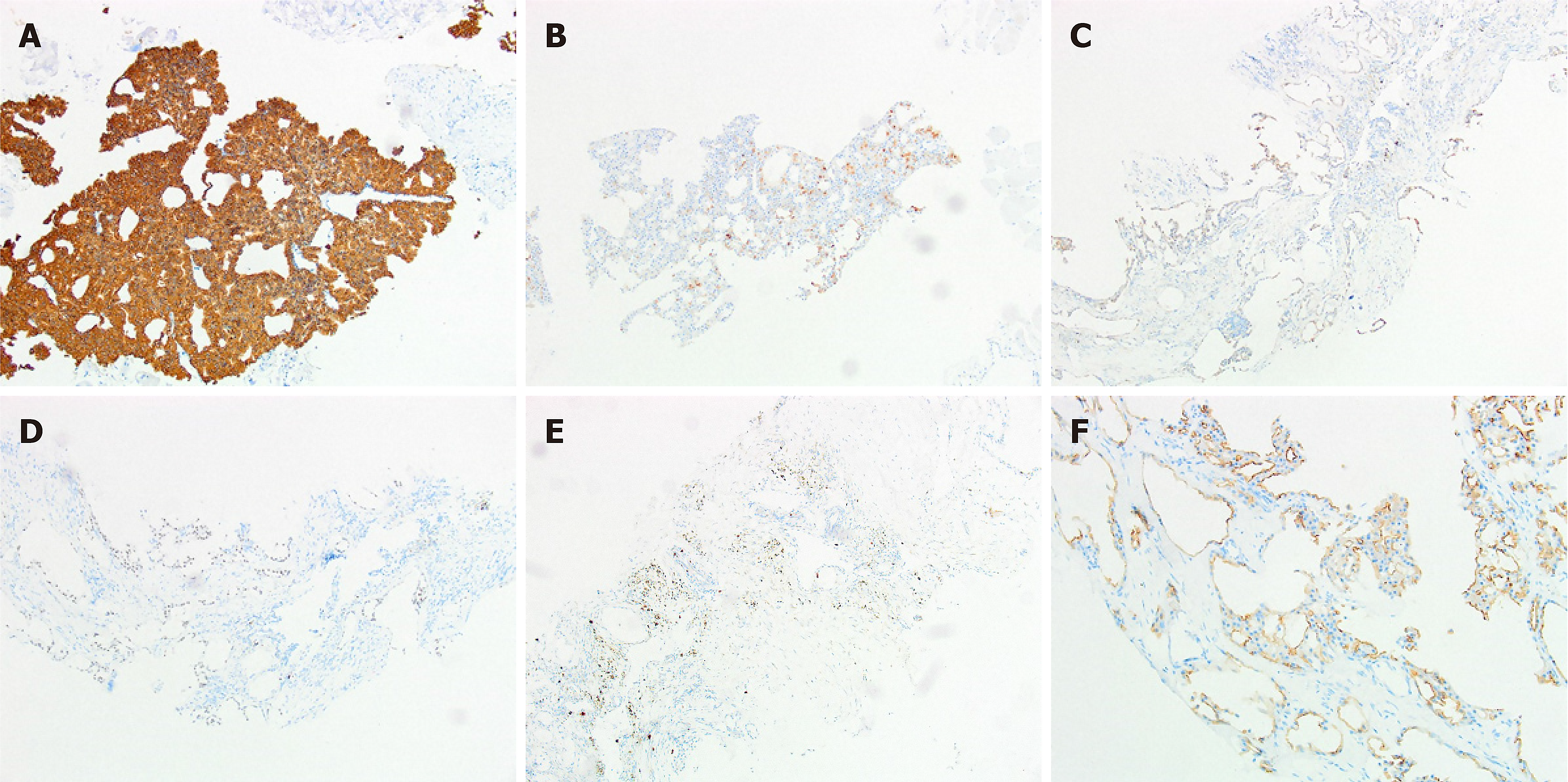
The patient underwent excision of the lesion with a surgical approach. A tumor appeared as solid clusters of cytoplasmic cells with granules similar to those found in serous acinar cells that were obviously acinus under the microscope. Based on histopathological examination, there was a preliminary suspicion of a tumor of epithelial origin, with the possibility of metastatic adenocarcinoma (Figure 2). However, through immune histochemical analysis, sex-determining region Y-related high-mobility group-box gene 10 (nucleus: +), DOG-1 (cell margin membrane: +) (Figure 3 and Table 1).
| Antibody | Results |
| CK-pan | + |
| EMA | Minority + |
| TTF-1 | - |
| CK7 | + |
| CK19 | + |
| CK20 | - |
| PSA | - |
| P63 | - |
| TG | - |
| S-100 | Minority + |
| Cg A | - |
| Syn | - |
| Ki-67 | Positive in 10% cells |
| SOX-10 | Nucleus: + |
| DOG-1 | Cell margin membrane: + |
Tracing the medical history, the patient underwent focal resection of facial tumors 5 years ago without regular follow-up and treatment after the surgery. Consideration of the patient’s medical history, the final diagnosis was confirmed as ACC of the parotid gland.
The patient received chemotherapy consisting of carboplatin and paclitaxel. After completing the computed tomography for radiotherapy positioning, the patient received continuous radiotherapy for the lesion in the left scapula.
According to the follow-up, the patient received comprehensive treatment including surgical resection and radiotherapy, and underwent regular imaging and clinical examinations after treatment. Currently, the mass in the scapular region has disappeared, and no new metastatic lesions have been found (Figure 1D). The patient’s physical condition is good.
ACC of the salivary gland is a rare malignant tumor that poses challenges in diagnosis due to its similarity to benign tumors on imaging studies[6]. However, computed tomography scan can be used to assess the size of the tumor, extent of involvement, proximity to facial nerve and other tissues, and the presence of distant metastases. Microscopically, ACC can present as solid, microcystic, tubular, cribriform, or follicular growth patterns, with solid growth variant being the most common, sharing similar histopathological characteristics with the case in question. The prognosis of salivary gland ACC depends on several factors, including tumor size, grade, lymph node involvement, completeness of surgical resection, and treatment response. Early diagnosis and comprehensive treatment are crucial for improving patient outcomes. Salivary gland ACC is known for its aggressive nature, frequent recurrences, and distant metastases, including rare cases of metastasis to the scapula[7]. ACC primarily metastasizes through the blood and lymphatic system, but its metastatic efficiency is low compared to other tumors. This may be due to the relatively weak aggressiveness and migration ability of ACC cells. The exact mechanism of metastasis from salivary gland ACC to the scapula remains unclear, highlighting the importance of monitoring bone metastasis in these patients.
Currently, the main treatment approach for ACC is surgical resection. In cases of extensive disease or suspected residual lesions, adjuvant therapies such as radiation and chemotherapy may be considered. Radiation therapy is commonly used as the preferred treatment for metastatic shoulder lesions[8]. In our patient case, a combination of systemic chemotherapy and external beam radiation therapy led to tumor regression. Further research is needed to understand the mechanisms and clinical significance of ACC metastasis. Enhanced postoperative follow-up, regular assessments, and ensuring early diagnosis are essential for reducing the occurrence of ACC metastasis and improving patient management and prognosis. In conclusion, for patients with salivary gland ACC, a comprehensive treatment approach, close monitoring, and individualized management are key to improving survival rates and quality of life.
ACC is a rare tumor that primarily affects the salivary glands. The preferred treatment approach for ACC is complete surgical excision. However, in cases with a poor prognosis or a risk of metastasis, regular follow-up and thorough examinations should be considered. It is crucial to conduct further studies to enhance our understanding of the treatment options and potential mechanisms of metastasis in this tumor.
| 1. | Spiro RH. Distant metastasis in adenoid cystic carcinoma of salivary origin. Am J Surg. 1997;174:495-498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 300] [Cited by in RCA: 295] [Article Influence: 10.5] [Reference Citation Analysis (0)] |
| 2. | De Luca P, Di Stadio A, de Campora L, De Bonis E, Fermi M, Petruzzi G, Atturo F, Colangeli R, Scarpa A, Lo Manto A, Colizza A, Cintoli G, Togo G, Salzano G, Crescenzi D, Ralli M, Abbate V, Ricciardiello F, Magaldi L, D'Ecclesia A, di Massa G, Costarelli L, Merenda E, Corsi A, Covello R, Di Crescenzo RM, Duda L, Dimitri LM, Caputo A, Ferrara G, Lucante T, Longo F, Tassone D, Iemma M, Cassano M, Salzano FA, Califano L, Marchioni D, Pellini R, de Vincentiis M, Presutti L, Ionna F, de Campora E, Radici M, Camaioni A. A Retrospective Multicenter Italian Analysis of Epidemiological, Clinical and Histopathological Features in a Sample of Patients with Acinic Cell Carcinoma of the Parotid Gland. Cancers (Basel). 2023;15:5456. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 3. | Hung YP, Jo VY, Hornick JL. Immunohistochemistry with a pan-TRK antibody distinguishes secretory carcinoma of the salivary gland from acinic cell carcinoma. Histopathology. 2019;75:54-62. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 8.3] [Reference Citation Analysis (0)] |
| 4. | Moon P, Tusty M, Divi V, Megwalu UC. Significance of Nodal Metastasis in Parotid Gland Acinar Cell Carcinoma. Laryngoscope. 2021;131:E1125-E1129. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | van Weert S, Valstar M, Lissenberg-Witte B, Bloemena E, Smit L, van der Wal J, Vergeer M, Smeele L, Leemans CR. Prognostic factors in acinic cell carcinoma of the head and neck: The Amsterdam experience. Oral Oncol. 2022;125:105698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 10] [Article Influence: 2.5] [Reference Citation Analysis (0)] |
| 6. | Sun Y, Di G, Jiang X. Primary salivary acinar cell carcinoma of the parotid gland with parietal skull metastasis: A case report. Asian J Surg. 2022;45:926-927. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Grasl S, Janik S, Grasl MC, Pammer J, Formanek M, Weinreb I, Perez-Ordonez B, Hope A, Hosni A, de Almeida JR, Irish J, Gilbert R, Goldstein DP, Erovic BM. Nodal Metastases in Acinic Cell Carcinoma of the Parotid Gland. J Clin Med. 2019;8:1315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 20] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | De Luca P, de Campora L, Tassone D, Atturo F, Colangeli R, Petruzzi G, Fermi M, Molinari G, Abeshi A, Cintoli G, Lo Manto A, Togo G, Ricciardiello F, Condorelli P, Raso F, Di Stadio A, Salzano G, Esposito E, D'Ecclesia A, Radici M, Iemma M, Vigili MG, Salzano FA, Magaldi L, Cassano M, Dallan I, Pellini R, Presutti L, Ionna F, de Campora E, Camaioni A. Acinic cell carcinoma of the parotid gland: Timeo Danaos et dona ferentes? A multicenter retrospective analysis focusing on survival outcome. Eur Arch Otorhinolaryngol. 2022;279:5821-5829. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |