Published online Feb 26, 2025. doi: 10.12998/wjcc.v13.i6.94330
Revised: September 28, 2024
Accepted: November 5, 2024
Published online: February 26, 2025
Processing time: 254 Days and 19.4 Hours
Hydroxyurea, an antimetabolite, is frequently prescribed for various hematological disorders, and its common side effects include gastrointestinal problems, cutaneous or mucosal lesions and pyrexia/fever.
This study reports the case of a 67-year-old woman who developed recurrent abdominal pain after 10 years of continuous hydroxyurea therapy for primary thrombocythemia. Colonoscopy revealed an ileocecal ulcer. After discontinuing hydroxyurea therapy for 6 months, follow-up colonoscopy showed a significant reduction in the ulceration.
We consider cecal ulcers as a rare complication of hydroxyurea therapy which typically resolves upon stopping the drug.
Core Tip: Ileocecal ulcers related to hydroxyurea are a rare adverse reaction and may be associated with drug hypersensitivity vasculitis and Behcet's disease. However, its specific pathogenic mechanism remains unknown. To date, only four cases of ileocecal ulcers have been reported worldwide, including three cases of the condition being complicated by pyrexia/fever, oral ulcers, and xerosis cutis. Pathological findings of ileocecal ulcers in these four cases revealed inflammatory changes that improved after hydroxyurea was discontinued. This report aims to raise awareness of the rare complication of hydroxyurea-induced ileocecal ulcers.
- Citation: Yuan WJ, Zheng YJ, Zhang BR, Lin YJ, Li Y, Qiu YY, Yu XP. Hydroxyurea-related ileocecal region ulcers as a rare complication: A case report. World J Clin Cases 2025; 13(6): 94330
- URL: https://www.wjgnet.com/2307-8960/full/v13/i6/94330.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i6.94330
Hydroxyurea is a non-alkylating antimetabolite that primarily functions by inhibiting ribonucleotide reductase, reducing the production of deoxyribonucleotides, and inducing termination of DNA synthesis during cell proliferation. Clinically, hydroxyurea is frequently used to treat myeloproliferative disorders and is generally well tolerated[1,2]. Common side effects associated with hydroxyurea include gastrointestinal symptoms (e.g., nausea, vomiting, diarrhea, mucositis, and anorexia), pyrexia/fever, and cutaneous or mucosal lesions (e.g., cutaneous ulcers, mucosal lesions, keratosis, mucocutaneous pigmentation, and dermatitis)[3,4]. Hydroxyurea-associated ileocecal ulcers have been rarely reported, with only four cases of reported to date in the literature. This study reports the case of recurrent abdominal pain developed after 10 years of continuous hydroxyurea therapy for primary thrombocythemia, aiming to raise awareness of hydroxyurea-associated ileocecal ulcers and provide a reference for diagnosing and treating ileocecal ulcers of unknown causes.
A 67-year-old Chinese woman presented to the infectious disease clinic with a complaint of abdominal-pian for 2 years.
In January 2018, her abdominal pain recurred predominantly in the upper, middle, and lower abdomen, with its episodes being more frequent than before. The patient reported no abdominal distention, constipation, diarrhea, or rectal bleeding, and she did not experience nausea or vomiting.
Eleven years ago, the patient was diagnosed with essential thrombocythemia and had been regularly receiving long-term treatment with hydroxyurea tablets 0.5 g bis in die for 10 years. In May 2016, she started experiencing recurrent abdo
The patient denied any family history of tuberculosis.
On physical examination, the vital signs were as follows: (1) Body temperature, 36.7 °C; (2) Blood pressure, 113 mmHg/73 mmHg; (3) Heart rate, 81 beats per minute; and (4) Respiratory rate, 22 breaths per minute. Furthermore, there are slight pressure pain in the lower and middle abdomen.
The routine blood test at our hospital showed white blood cell (WBC) count of 7.21 × 109/L and C-reactive protein (CRP) level of 29.6 mg/L. No overt abnormalities were noted in cardiac, hepatic, and renal function parameters (e.g., blood lipid and tumor markers).
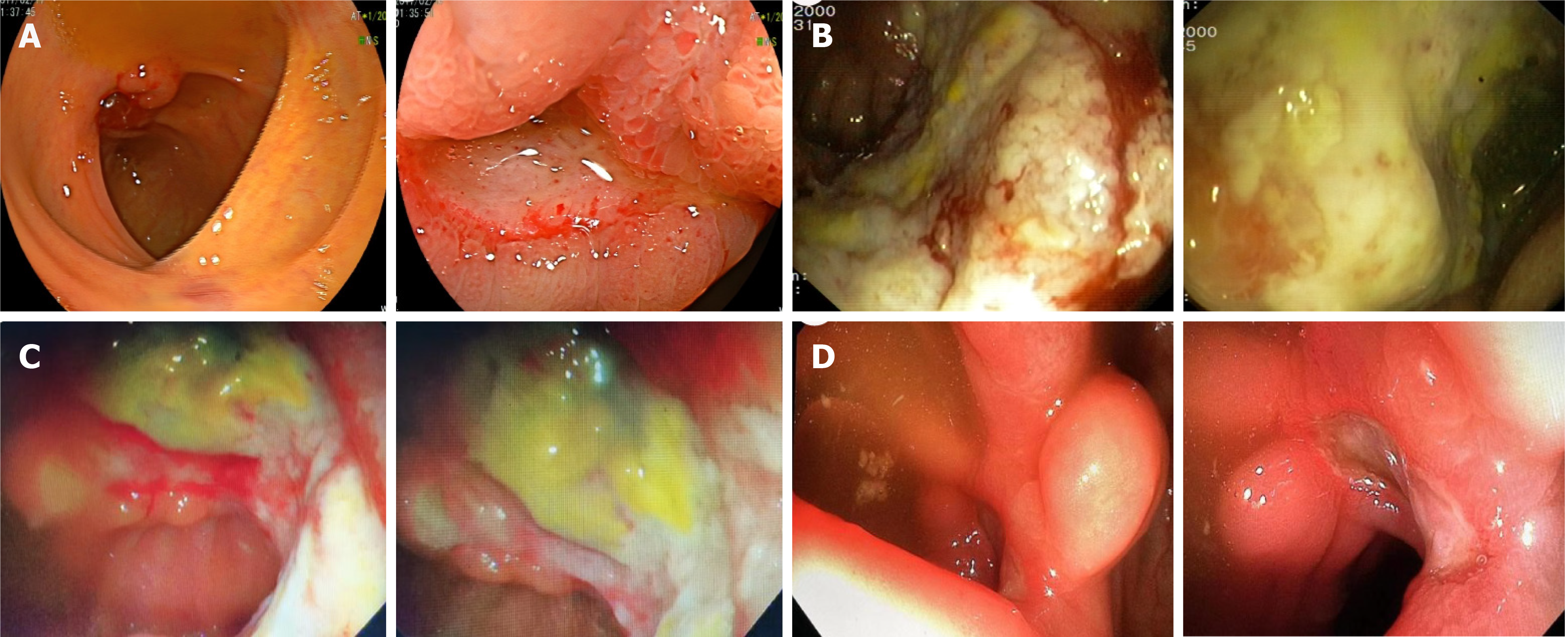
Gastroscopy performed at our hospital suggested chronic inflammation of the gastric mucosa. Colonoscopy revealed a giant, hard, easily bleeding, irregular ulcer on the ileocecal valve with an ill-defined edge and a dirty coating on the surface (Figure 1B). Pathological examination of the ileocecal valve revealed acute and chronic mucosal inflammation accompanied by erosions, inflammatory exudates and tissues, negative acid-fast bacilli stain, and negative polymerase chain reaction for Mycobacterium tuberculosis.
Ileocecal ulcers related to hydroxyurea.
The patient was initially diagnosed with intestinal tuberculosis or Crohn's disease. Her symptoms slightly improved after symptomatic treatments for inhibiting gastric acid secretion and protecting the stomach, regulating gastrointestinal motility, and relaxing the bowels. Then, she was advised to undergo positron emission tomography-computed tomography (PET-CT) and consider diagnostic antituberculosis treatment. The patient and her family denied PET-CT but approved diagnostic therapy with isoniazid, rifampicin, pyrazinamide, and ethambutol. After 1 week of treatment, the patient discontinued antituberculosis treatment by herself but continued receiving 0.5 g of oral hydroxyurea biweekly (biw). In September 2021, the patient started experiencing pyrexia/fever, with temperatures gradually rising up to 39 °C.
In addition, she also reported chills, vomiting of gastric contents, oral ulcers, and xerosis cutis. A computed tomo
On December 8, 2021, an electronic colonoscopy was performed again, revealing a giant irregular ulcer near the ileocecal valve, measuring approximately 3.0 cm × 5.0 cm; the ulcer had an irregular edge, was dirty on the surface, and had a hard texture prone to bleeding. The biopsy of the ulcer near the ileocecal valve showed chronic active mucosal inflammation accompanied by inflammatory exudation, necrosis, and granulation tissue formation, suggestive of ulceration (Figure 1C).
Immunohistochemistry showed negative findings for various markers: (1) Cytomegalovirus (-), human herpesvirus 8
A follow-up PET-CT scan was performed, which showed localized thickening of the intestinal wall with increased glucose metabolism from terminal ileum to ileocecal junction. Based on the patient’s medical history, a diagnosis of inflammatory bowel disease was considered. This patient was advised to undergo reexamination after treatment, and possible repeat pathological examinations were recommended if necessary to rule out lymphoma. Multiple small lymph nodes were observed at the ileocecal junction, with slightly elevated glucose metabolism, suggesting inflammatory hyperplasia. During hospitalization, this patient continued experiencing recurrent episodes of pyrexia and undulant fever, with her body temperature rapidly rising to above 39 °C and then rapidly dropping to normal temperatures after two to three days. After the patient remained afebrile for three to four days, her body temperature rose again and recurrently (changes in the eosinophil count noted at this time), and these fever episodes coincided with her hydroxyurea intake (biw).
During the fever episodes, the patient also presented with oral ulcers and xerosis cutis, further suggesting the possibility of drug-induced fever due to hydroxyurea. Given the confirmed diagnosis of primary thrombocythemia with a JAK2 V617 mutation and maintenance of stable platelet count, hydroxyurea was discontinued. Simultaneously, antibiotic therapy, acid suppression, and interventions to regulate the intestinal microbiota/flora were stopped. Instead, treatments with multivitamins and folic acid was provided. The patient’s body temperature returned to normal, and abdominal pain, oral ulcer, and xerosis cutis were markedly improved. Electronic colonoscopy in June 2022 showed: (1) A soft irregular ulcer near the ileocecal valve, measuring approximately 0.6 cm × 1.8 cm, with an ill-defined edge and some dirty coatings on the surface; and (2) The ulcer was improved (Figure 1D).
Electronic colonoscopy in June 2022 showed: (1) A soft irregular ulcer near the ileocecal valve, measuring approximately 0.6 cm × 1.8 cm, with an ill-defined edge and some dirty coatings on the surface; and (2) The ulcer was improved (Figure 1D).
Hydroxyurea-associated mucosal lesions, which predominate in the oral cavity, are highly prevalent in women. Mucosal lesions have been reported at a rate of 17%, mainly characterized by pain and burning sensation[4]. In this report, our patient developed an oral ulcer during the course of the disease. However, occurrence of this complication (i.e., the ulcer) was unrelated to the therapeutic dose of hydroxyurea and duration of continuous medication use[4-6]. Meanwhile, ileocecal ulcers are associated with the dose and duration of hydroxyurea use. Although symptomatic and supportive treatments for protecting against infections, inhibiting gastric acid secretion, protecting the stomach, and regulating intestinal flora could somewhat improve abdominal pain, the ileocecal ulcer and abdominal pain persisted for a long period. Notably, intestinal tuberculosis and Crohn’s disease have a predilection for the ileocecal region and thus are readily misdiagnosed. However, the PET-CT and ileocecal valve biopsy results are unsupportive of such misdiagnosis.
After symptomatic and supportive treatments (e.g., hydroxyurea and anti-infective treatment) were discontinued, the patient’s body temperature returned to normal, and abdominal pain, oral ulcers, and xerosis cutis resolved. A follow-up examination 6 months later showed significant reduction in the size of the ileocecal ulcer. Consequently, the diagnosis of hydroxyurea-related ileocecal ulcers and fever was established.
Ileocecal ulcers related to hydroxyurea are a rare adverse reaction and may be associated with drug hypersensitivity vasculitis and Behcet's disease[7]. However, its specific pathogenic mechanism remains unknown. To date, only four cases of ileocecal ulcers have been reported worldwide[7], including three cases of the condition being complicated by pyrexia/fever, oral ulcers, and xerosis cutis. Pathological findings of ileocecal ulcers in these four cases revealed inflammatory changes that improved after hydroxyurea was discontinued[7-10].
Given the rarity of hydroxyurea-related non-oral gastrointestinal ulcers, we searched PubMed and screened out 4 valid cases and summarize them in the Table 1[7-10].
| Ref. | Age (years) | Sex | Ulcer site | Diagnosis method | Treatment |
| Yousuf K[9] | 66 | M | Jejunum | Colonoscopy | Discontinue hydroxyurea |
| Kobune M et al[8] | 74 | M | Duodenum and colon | Gastro-intestinal and colon fiberoscopy | Discontinue hydroxyurea |
| Boonyawat K et al[7] | 37 | M | Terminal ileum and colon | Esophago-gastro-duodenoscopy | Discontinue hydroxyurea |
| Jayaraman T et al[10] | 73 | F | ICV | Colonoscopy | Discontinue hydroxyurea |
| Patient presented in this case report | 67 | F | ICV | Colonoscopy | Discontinue hydroxyurea |
This report aims to raise awareness of the rare complication of hydroxyurea-induced ileocecal ulcers. When patients taking hydroxyurea experience symptoms such as loss of appetite, abdominal pain, diarrhea, and oral ulcers, hydroxyurea should be discontinued or replaced with alternative medications in a timely manner, and increased endoscopic surveillance is recommended to detect ulcers.
The authors are grateful to all staff at the Department of Infectious Diseases, Fujian Medical University Affiliated First Quanzhou Hospital.
| 1. | Saban N, Bujak M. Hydroxyurea and hydroxamic acid derivatives as antitumor drugs. Cancer Chemother Pharmacol. 2009;64:213-221. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 84] [Cited by in RCA: 89] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 2. | Tefferi A. Primary myelofibrosis: 2023 update on diagnosis, risk-stratification, and management. Am J Hematol. 2023;98:801-821. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 137] [Reference Citation Analysis (0)] |
| 3. | Mascarenhas J, Kosiorek HE, Prchal JT, Rambaldi A, Berenzon D, Yacoub A, Harrison CN, McMullin MF, Vannucchi AM, Ewing J, O'Connell CL, Kiladjian JJ, Mead AJ, Winton EF, Leibowitz DS, De Stefano V, Arcasoy MO, Kessler CM, Catchatourian R, Rondelli D, Silver RT, Bacigalupo A, Nagler A, Kremyanskaya M, Levine MF, Arango Ossa JE, McGovern E, Sandy L, Salama ME, Najfeld V, Tripodi J, Farnoud N, Penson AV, Weinberg RS, Price L, Goldberg JD, Barbui T, Marchioli R, Tognoni G, Rampal RK, Mesa RA, Dueck AC, Hoffman R. A randomized phase 3 trial of interferon-α vs hydroxyurea in polycythemia vera and essential thrombocythemia. Blood. 2022;139:2931-2941. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 80] [Article Influence: 26.7] [Reference Citation Analysis (0)] |
| 4. | Antonioli E, Guglielmelli P, Pieri L, Finazzi M, Rumi E, Martinelli V, Vianelli N, Luigia Randi M, Bertozzi I, De Stefano V, Za T, Rossi E, Ruggeri M, Elli E, Cacciola R, Cacciola E, Pogliani E, Rodeghiero F, Baccarani M, Passamonti F, Finazzi G, Rambaldi A, Bosi A, Cazzola M, Barbui T, Vannucchi AM; AGIMM Investigators. Hydroxyurea-related toxicity in 3,411 patients with Ph'-negative MPN. Am J Hematol. 2012;87:552-554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 91] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 5. | Mendonça R, Gueiros LA, Capellaro K, Pinheiro VR, Lopes MA. Oral lesions associated with hydroxyurea treatment. Indian J Dent Res. 2011;22:869-870. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Norhaya MR, Cheong SK, Ainoon O, Hamidah NH. Painful oral ulcers with hydroxyurea therapy. Singapore Med J. 1997;38:283-284. [PubMed] |
| 7. | Boonyawat K, Wongwaisayawan S, Nitiyanant P, Atichartakarn V. Hydroxyurea and colonic ulcers: a case report. BMC Gastroenterol. 2014;14:134. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 8. | Kobune M, Kato J, Kuribayashi K, Iyama S, Fujimi A, Murase K, Ueno A, Kikuchi S, Satoh T, Okamoto T, Takimoto R, Matsunaga T, Niitsu Y. [Essential thrombocythemia associated with incomplete type intestinal Behçet disease during hydroxyurea treatment]. Rinsho Ketsueki. 2005;46:1136-1140. [PubMed] |
| 9. | Yousuf K. A case of bleeding jejunal ulcer due to vasculitis from hydroxyurea. Am J Gastroenterol. 2000;95:2616. [DOI] [Full Text] |
| 10. | Jayaraman T, Rajaram RB, Gan GG, Hilmi I. Hydroxyurea associated ileocecal valve ulcer: evidence for causality. Intest Res. 2021;19:468-471. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |