Published online Feb 26, 2025. doi: 10.12998/wjcc.v13.i6.100263
Revised: September 25, 2024
Accepted: November 5, 2024
Published online: February 26, 2025
Processing time: 105 Days and 15.7 Hours
Optimal health during pregnancy is crucial for ensuring the well-being of the mother and the developing fetus. This article is focused on the impact of oral health and the role of personalized oral hygiene management in addressing prevalent dental issues among pregnant women, with particular emphasis on periodontal disease and dental caries. Despite the high prevalence of these dental problems and their association with obstetric complications such as pre-term birth and low birth weight, many pregnant women do not receive adequate dental care. This gap in care is often due to misconceptions about the safety of dental treat
Core Tip: In this article, we reviewed a recent study on the effects of personalized oral hygiene management on the oral health of pregnant women, as discussed in the article by Men et al. The study demonstrated that personalized oral hygiene interventions significantly improved oral health outcomes during pregnancy by reducing the prevalence of dental caries and periodontal disease. We emphasized the importance of individualized oral care programs that integrate education and tailored support, and we highlighted their significance in enhancing maternal and fetal health. This approach underscores the need for incorporating personalized oral hygiene management into routine prenatal care in order to optimize health outcomes.
- Citation: Martínez Nieto M, De León Rodríguez ML, Alcaraz Baturoni FJ, Soto Chávez AA, Lomelí Martínez SM. Link between caries, periodontitis, and pregnancy: The role of personalized oral hygiene. World J Clin Cases 2025; 13(6): 100263
- URL: https://www.wjgnet.com/2307-8960/full/v13/i6/100263.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i6.100263
Oral health during pregnancy is a topic of growing interest in medical and dental research, due to the significant relationship between oral conditions and maternal and fetal health. Oral lesions such as periodontal disease and dental caries are common conditions during pregnancy, and they are associated with local and systemic effects. Dental caries is a primary health problem worldwide. Indeed, the World Health Organization has estimated dental carries incidence of 60%-90% in the global population, with a higher prevalence in adults. Dental carries is a chronic disease with a multi
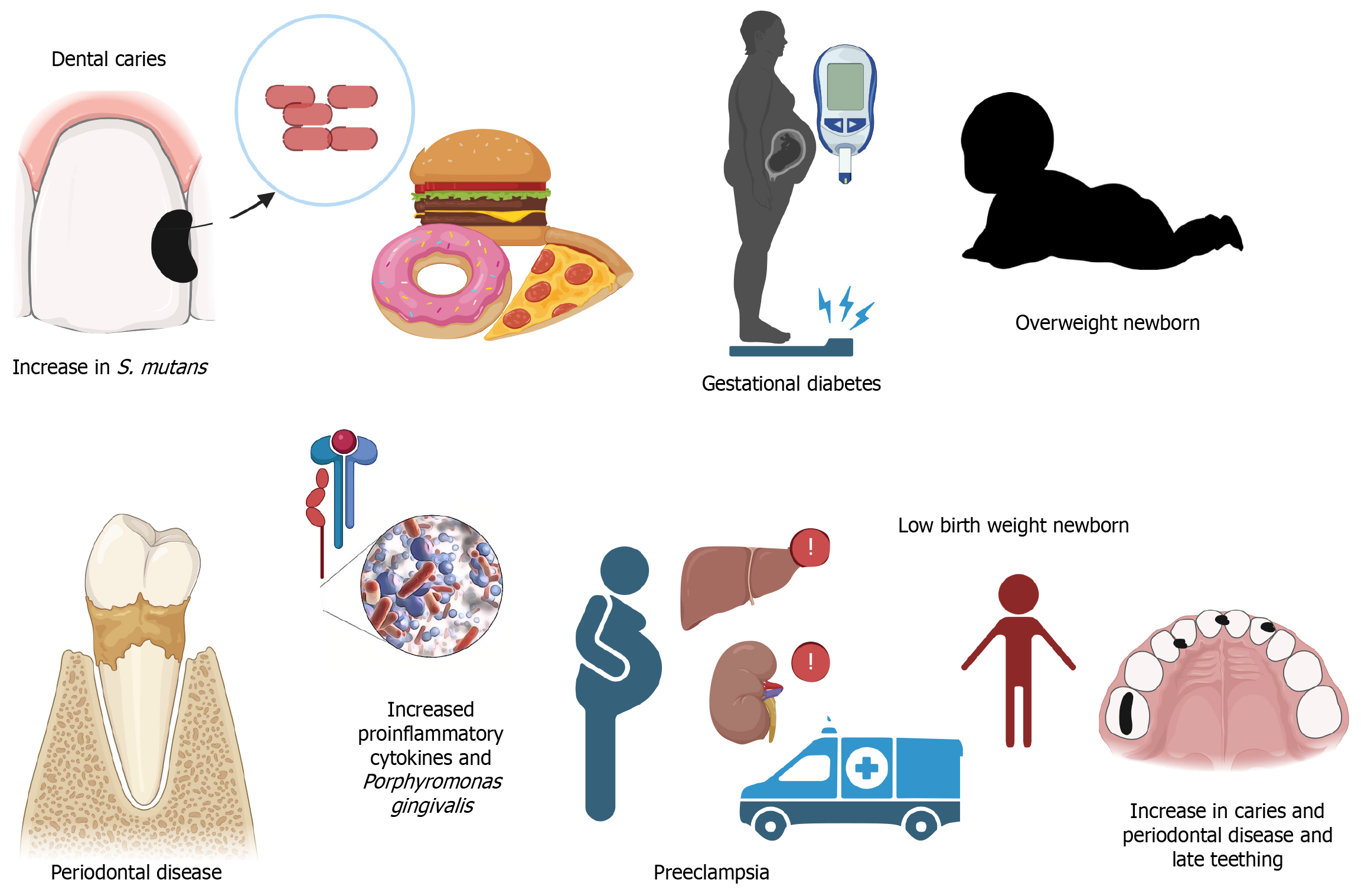
On the other hand, periodontal diseases, particularly periodontitis which is the sixth most important dental disease globally[3], are characterized by inflammation of the supporting dental structures and alveolar bone due to local and systemic elevations in the levels of pro-inflammatory cytokines[4,5]. These conditions, in turn, have been associated with gestational complications such as pre-term birth, preeclampsia, hemodynamic alterations, hypertension during pregnancy, and low neonatal birth weight[1,6]. Additionally, poor oral health negatively impacts the quality of life of pregnant women, by causing pain, difficulty in eating, and psychological stress.
However, despite the importance of these issues, many pregnant women do not receive adequate dental care, partly due to the misconception that dental diseases are not treated during pregnancy. On the contrary, it is recognized that oral cavity diseases are related to complications that may be serious, thereby endangering maternal and fetal health. However, it has been observed that a significant number of oral health professionals avoid performing procedures during pregnancy[7,8]. On the other hand, other healthcare professionals are unaware of the relationship between oral and systemic diseases. In the United States, a study has revealed that 49% of obstetricians never provided dental health recommendations to their patients, while only 9% performed oral examinations regularly. From these studies, it was concluded that it is essential to reinforce information in this field of health, with emphasis on pregnancy[9].
Whatever the scenario, it is indisputable that attention to oral health during pregnancy should not be underestimated. Without a doubt, part of the problem we face lies in the lack of information about the implications and possible complications that may arise or be exacerbated during pregnancy in women with oral cavity diseases[4]. Oral hygiene education must be a global health priority, in addition to monitoring and referral to specialists whenever necessary. It has been shown that medical care should be individualized in order to achieve better outcomes. Some researchers have pointed out that the treatment of dental disease is possible at any stage of pregnancy, if necessary precautions and advice by the obstetrician/gynecologist are taken seriously. In this respect, the second trimester is considered the most appropriate period for performing dental treatment procedures. In a 2019 declaration by the American Dental Association, it was clearly stated care should not be avoided in any situation[7].
In all cases, dental evaluation should be considered as an important part of pregnancy follow-up, as well as education in this area so as to improve hygiene and dietary habits which significantly benefit the mother and the fetus. It has been estimated that with proper management and care of dental diseases, preterm births may be reduced by up to 6%, thereby improving quality of life of children and reducing the incidence of caries in early childhood[10]. It is known that preterm and low birth weight newborns have high incidence of dental caries at this stage of life, in addition to delayed dentition[11].
The objective of this study was to investigate the importance of advice and treatment for oral pathologies during pregnancy, and their impact on maternal and fetal health.
Pregnancy is a physiological state in women which involves series of changes at all levels which are aimed at adaptation to meet the increased metabolic demand during gestation. These changes occur gradually throughout the pregnancy period, and they involve mechanical, biochemical, and structural processes. Biochemically, hormones such as relaxin, human chorionic gonadotropin, estrogens, progestogens, prolactin, oxytocin, cortisol, and the thyroid axis, play predo
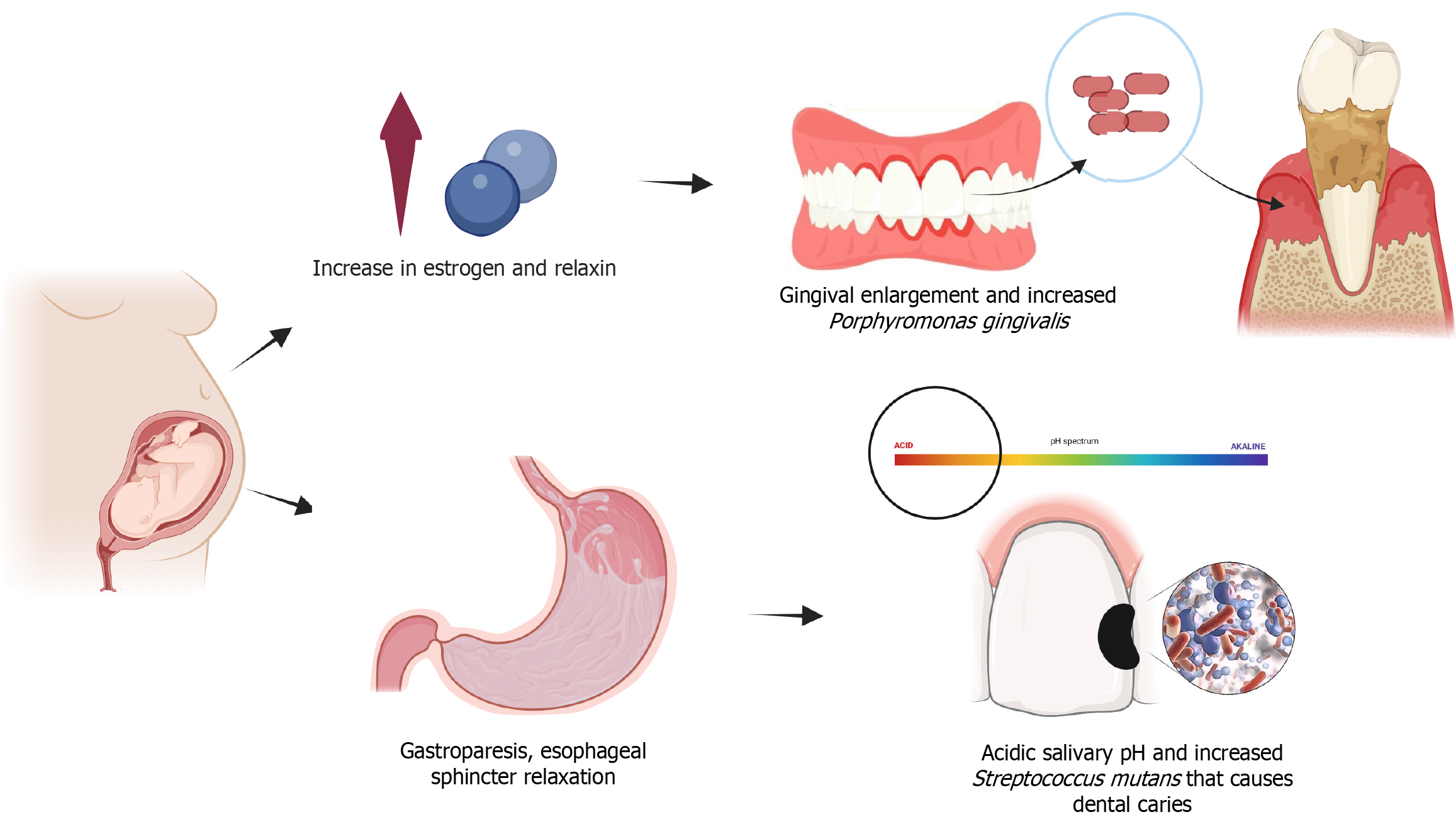
Pregnant women have a higher susceptibility to oral diseases due to the changes that occur during pregnancy. One of the most recognized changes is enlargement of the gingiva, which enhances gingivitis and is associated with increased estrogen levels, while a decrease in estrogen level is linked to the presence of periodontitis[13]. Although the association with caries is not well studied, it has been related to changes in salivary pH due to gastroesophageal reflux and vomiting, thereby favoring the growth of cariogenic bacteria[14]. This leads to an increase in prevalence of caries. Moreover, due to hormonal changes, pregnancy may lead to a condition known as dry mouth (xerostomia) which diminishes the natural cleansing action of saliva. Since saliva naturally contains antimicrobial properties, a reduction in its production exacer
Several researchers have studied the modifications in oral microbiome during pregnancy. These studies indicate that a significant presence of Porphyromonas gingivalis (P. gingivalis) increases the risk of preterm birth. Changes in placental microbiota have been identified in pregnant women with glycemic alterations. These changes alter the course of pregnancy and increase the risk of oral diseases in newborns at an earlier age. Studies have demonstrated that children of mothers with high concentrations of Streptococcus mutans are at great risk of developing dental caries at an earlier age (Figure 1)[10,15].
Preterm birth is a complication associated with infectious processes during pregnancy. Numerous studies have shown that elevated pro-inflammatory cytokines play an important role in development of preterm birth, as does increase in population of oral cavity bacterial species such as P. gingivalis[10]. It is important to note that globally, prematurity accounts for 60%-80% of neonatal mortality unrelated to malformations, and up to 50% of these children have some neurological problems throughout their lives[7]. Additionally, studies suggest that dental caries and high consumption of non-natural sweeteners, in addition to low or zero intake of vegetables and poor oral hygiene practices, contribute to the birth of large-for-gestational-age infants, thereby increasing the risk of obstetric trauma. Some risk factors for caries during pregnancy may be associated with bad habits such as poor diet, consumption of sugary beverages, and sedentary lifestyle. Pregnant women may experience cravings for sugary or acidic foods, which may contribute to the development of caries[1]. Preeclampsia is a pregnancy complication that has been associated with periodontal diseases, while glycemic alterations are strongly influenced by increased sugar consumption during this period (Figure 2).
Personalized oral hygiene management is a strategy characterized by comprehensive and tailored approach aimed at optimizing the oral health of the patient through methods adapted to their specific conditions[16-18]. This type of management involves a thorough assessment of the patient's oral health by taking into account risk factors such as predisposition to dental conditions, physiological changes that may alter the oral microbiota, and individual characteristics such as hygiene habits, diet, and preexisting systemic conditions[17-20].This approach contrasts with routine oral care which is based on standard procedures and general recommendations that may not always address the specific needs of each individual.
Routine oral care refers to conventional oral care practices which involve procedures such as dental prophylaxis, i.e., the use of general hygiene tools (conventional toothbrushes, dental floss, and interdental brushes), and fluoride application[21]. However, these common practices do not always account for individual patient needs. They tend to be more generalized and uniform approaches based on standard recommendations applied similarly to all cases. These conventional practices may be less effective for patients with specific needs, such as pregnant women, individuals with chronic diseases, and those at higher risk of oral diseases[21-24].
On the other hand, personalized oral hygiene management not only provides education on oral hygiene but also incorporates tailored interventions such as dental prophylaxis adapted to the risk conditions of the patient, regular monitoring and individualized follow-up, and continuous advice based on specific challenges identified through questionnaires and personalized consultations. Personalized approach utilizes various methods such as online and in-person courses, educational models, and case discussions, all of which are adjusted to meet the individual needs and concerns of patients.
Men et al[25] published an article titled "Effects of personalized oral hygiene management on the oral health status of pregnant women". The study evaluated the impact of personalized oral hygiene management on the oral health of pregnant women, and it involved 120 pregnant women from the Dalian Women and Children’s Medical Center in China. Based on the caries activity test (CAT), the subjects were divided into two groups: High-risk (CAT ≥ 2; n = 60) and low-risk (CAT ≤ 1; n = 60). Each group was further sub-divided into experimental and control groups, each with 30 subjects (n = 30). The high-risk experimental group received personalized oral hygiene management which entailed education on oral health focused on the etiology and consequences of dental caries and periodontal diseases, as well as education on oral care practices during pregnancy. The education was delivered through online and in-person courses, educational models, and case discussions, and it was supplemented with individualized counseling and online Question & Answer sessions available at all times.
The results of the study[25] revealed significant reductions in CAT scores after 3 months (1.74 ± 0.47 vs 2.50 ± 0.38, P < 0.0001) and 6 months (0.53 ± 0.50 vs 2.45 ± 0.42, P < 0.0001) of personalized intervention in the high-risk experimental group, when compared to the control group. However, the reduction in score produced by oral health education alone was not significant. Within the groups, the decrease in score was significant only in the high-risk experimental group (2.43 ± 0.44 vs 1.74 ± 0.47 vs 0.53 ± 0.50, P < 0.0001). This study[25] demonstrates that personalized oral hygiene management is effective in improving the oral health of pregnant women. This may lead to better pregnancy outcomes and an overall improvement in oral health in this population. These findings are comparable to those obtained by George et al[26]. Reduction in early childhood caries was evaluated in a systematic review focused on assessment of the effectiveness of maternal oral health programs implemented during the prenatal and/or postnatal periods by non-dental healthcare professionals. The review included nine studies in which interventions were conducted by various non-dental professionals during prenatal (n = 1), postnatal (n = 6), and perinatal (n = 2) periods. The intervention methods were varied, ranging from oral health education and evaluations to dental services referrals. Educational approaches involved verbal counseling, motivational interviews, home visits, telephone follow-ups, and written promotional materials such as brochures, postcards, and educational kits.
Although educational programs significantly improved oral hygiene practices and increased the frequency of dental visits, not all studies reported significant reductions in the incidence of caries among the children of participants. Both studies underscore the importance of oral health during pregnancy, through the implementation of educational interventions, although they differ in approach and methodology. While the study by Men et al[25], which focused on direct and personalized interventions such as professional dental prophylaxis and education, showed significant reductions in caries, the study by George et al[26] emphasized the training of non-dental healthcare professionals in order to improve the oral health of pregnant women, and it highlighted the importance of continuous education and follow-up, albeit with variability in caries outcomes.
It is undeniable that improving dental health education for pregnant women and healthcare professionals in other disciplines is crucial for enhancing pregnancy outcomes and reducing the risks of complications previously mentioned[8]. Numerous studies have specifically highlighted the association between periodontitis and pregnancy complications, as well as the benefits of treating this condition. However, there is limited knowledge about the impact of dental caries during pregnancy and its harmful effects on pregnant women and newborns. Additionally, it is important to emphasize the considerable fear and lack of knowledge among healthcare professionals regarding the treatment of oral conditions in pregnant women, especially those with concomitant diseases. This situation presents significant opportunities for improvement.
The findings presented in the study by Men et al[25] on the effects of personalized oral hygiene management in pregnant women pave the way for several important directions for future research on oral care management in expectant mothers[16].
Although it has been established that personalized oral hygiene management has a significantly positive impact on the oral health of pregnant women, future research should consider integrating a larger and more diverse sample that represents different regions and cultures, in order to validate and generalize the findings. It would be interesting to investigate the impact of oral care intervention during different trimesters of pregnancy so as to determine if there are significant differences in effectiveness. It would also be valuable to implement longitudinal studies aimed at identifying the long-term effects of personalized oral hygiene management on the oral health of mothers and their children. Additionally, studying the association between improved oral health during pregnancy and the reduction of oral pathogen transmission to newborns may provide further insights.
Some authors assert that pregnant women with oral diseases, particularly periodontal diseases, e.g., periodontitis, are more prone to preterm births and low birth weight than those without these conditions. However, the exact mechanisms by which these relationships occur remain unknown[27,28]. Future research should focus on how enhanced oral health during pregnancy might influence outcomes such as birth weight, pregnancy duration, and neonatal health. Furthermore, it would be valuable to study whether personalized oral hygiene management has the potential to reduce the incidence of complications such as preeclampsia, preterm birth, and low birth weight.
Integration of oral hygiene into maternal and child health programs may enhance overall health outcomes. Continuous educational programs for pregnant women and healthcare professionals on the importance of oral health should be incorporated. These multidisciplinary programs would enhance the evaluation of the integration and effectiveness of personalized oral hygiene management in pregnant women.
These research areas will expand the current understanding of oral hygiene management in pregnant women and also contribute to improving clinical practices and public health policies aimed at expectant women.
This article emphasizes the critical role of personalized oral hygiene management in improving oral health during pregnancy. By tailoring oral care strategies to individual needs, significant improvements in dental health may be achieved, as evidenced by the reduced CAT scores observed in the experimental group in the study by Men et al[25]. This personalized approach not only addresses common oral issues such as dental caries and periodontal disease but also underscores the broader implications for maternal and fetal health. Despite the positive results, there remains a gap in consistency in the application of oral health practices during pregnancy, partly due to misconceptions and lack of awareness among patients and healthcare providers. Future research should aim at validating these findings across diverse populations, investigating the impact of oral hygiene interventions at various stages of pregnancy, and evaluating their long-term effects on maternal and fetal health. Integrating personalized oral hygiene management into maternal health programs and promoting continuous education for pregnant women and healthcare professionals are essential steps toward enhancing overall health outcomes. By proactively managing oral health, the risks associated with pregnancy may be reduced while improving maternal and neonatal well-being.
| 1. | Cho GJ, Kim SY, Lee HC, Kim HY, Lee KM, Han SW, Oh MJ. Association between dental caries and adverse pregnancy outcomes. Sci Rep. 2020;10:5309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 2. | Saikia S, Mathur S, Malik M, Gulati N. Correlation of caries occurrence in primary teeth using human leukocyte antigen typing and maternal and physiochemical factors. J Indian Soc Pedod Prev Dent. 2022;40:124-131. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 3. | Chatzopoulos GS, Jiang Z, Marka N, Wolff LF. Periodontal Disease, Tooth Loss, and Systemic Conditions: An Exploratory Study. Int Dent J. 2024;74:207-215. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 16] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 4. | Almabadi ES, Seymour GJ, Akhter R, Bauman A, Cullinan MP, Eberhard J. Reduction of hsCRP levels following an Oral Health Education Program combined with routine dental treatment. J Dent. 2021;110:103686. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Nazir M, Al-Ansari A, Al-Khalifa K, Alhareky M, Gaffar B, Almas K. Global Prevalence of Periodontal Disease and Lack of Its Surveillance. ScientificWorldJournal. 2020;2020:2146160. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 238] [Cited by in RCA: 293] [Article Influence: 58.6] [Reference Citation Analysis (1)] |
| 6. | Kapila YL. Oral health's inextricable connection to systemic health: Special populations bring to bear multimodal relationships and factors connecting periodontal disease to systemic diseases and conditions. Periodontol 2000. 2021;87:11-16. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 77] [Cited by in RCA: 188] [Article Influence: 47.0] [Reference Citation Analysis (0)] |
| 7. | Aliabadi T, Saberi EA, Motameni Tabatabaei A, Tahmasebi E. Antibiotic use in endodontic treatment during pregnancy: A narrative review. Eur J Transl Myol. 2022;32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 8. | Bashirian S, Barati M, Barati M, Shirahmadi S, Khazaei S, Jenabi E, Gholami L. Promoting Oral Health Behavior During Pregnancy: A Randomized Controlled Trial. J Res Health Sci. 2023;23:e00584. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Faden AA, Alsalhani AB, Idrees MM, Alshehri MA, Nassani MZ, Kujan OB. Knowledge, attitudes, and practice behavior of dental hygienists regarding the impact of systemic diseases on oral health. Saudi Med J. 2018;39:1139-1147. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 10. | Jang H, Patoine A, Wu TT, Castillo DA, Xiao J. Oral microflora and pregnancy: a systematic review and meta-analysis. Sci Rep. 2021;11:16870. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 50] [Cited by in RCA: 68] [Article Influence: 17.0] [Reference Citation Analysis (0)] |
| 11. | Koberova R, Radochova V, Zemankova J, Ryskova L, Broukal Z, Merglova V. Evaluation of the risk factors of dental caries in children with very low birth weight and normal birth weight. BMC Oral Health. 2021;21:11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 12. | Carrillo-mora P, García-franco A, Soto-lara M, Rodríguez-vásquez G, Pérez-villalobos J, Martínez-torres D. Cambios fisiológicos durante el embarazo normal. Rev Fac Med. 2021;64:39-48. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Robinson JL, Johnson PM, Kister K, Yin MT, Chen J, Wadhwa S. Estrogen signaling impacts temporomandibular joint and periodontal disease pathology. Odontology. 2020;108:153-165. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 53] [Article Influence: 8.8] [Reference Citation Analysis (0)] |
| 14. | Napso T, Yong HEJ, Lopez-Tello J, Sferruzzi-Perri AN. The Role of Placental Hormones in Mediating Maternal Adaptations to Support Pregnancy and Lactation. Front Physiol. 2018;9:1091. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 194] [Cited by in RCA: 282] [Article Influence: 40.3] [Reference Citation Analysis (0)] |
| 15. | Lassi ZS, Imam AM, Dean SV, Bhutta ZA. Preconception care: caffeine, smoking, alcohol, drugs and other environmental chemical/radiation exposure. Reprod Health. 2014;11 Suppl 3:S6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 95] [Cited by in RCA: 85] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 16. | Girestam Croonquist C, Dalum J, Skott P, Sjögren P, Wårdh I, Morén E. Effects of Domiciliary Professional Oral Care for Care-Dependent Elderly in Nursing Homes - Oral Hygiene, Gingival Bleeding, Root Caries and Nursing Staff's Oral Health Knowledge and Attitudes. Clin Interv Aging. 2020;15:1305-1315. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (1)] |
| 17. | Rigo L, Dalazen J, Garbin RR. Impact of dental orientation given to mothers during pregnancy on oral health of their children. Einstein (Sao Paulo). 2016;14:219-225. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 12] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 18. | Walsh T, Worthington HV, Glenny AM, Marinho VC, Jeroncic A. Fluoride toothpastes of different concentrations for preventing dental caries. Cochrane Database Syst Rev. 2019;3:CD007868. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 165] [Cited by in RCA: 220] [Article Influence: 36.7] [Reference Citation Analysis (0)] |
| 19. | Fonseca EOS, Pedreira LC, Silva RSD, Santana RF, Tavares J, Martins MM, Góes RP. (Lack of) oral hygiene care for hospitalized elderly patients. Rev Bras Enferm. 2021;74:e20200415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Nicolae FM, Bennardo F, Barone S, Șurlin P, Gheorghe DN, Burtea D, Pătrascu Ș, Râmboiu S, Radu AP, Ungureanu BS, Turcu-Știolica A, Didilescu AC, Strâmbu VDE, Șurlin VM, Gheonea DI. The Need for Oral Hygiene Care and Periodontal Status among Hospitalized Gastric Cancer Patients. J Pers Med. 2022;12:684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 21. | Worthington HV, MacDonald L, Poklepovic Pericic T, Sambunjak D, Johnson TM, Imai P, Clarkson JE. Home use of interdental cleaning devices, in addition to toothbrushing, for preventing and controlling periodontal diseases and dental caries. Cochrane Database Syst Rev. 2019;4:CD012018. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 78] [Cited by in RCA: 118] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 22. | Waldron C, Nunn J, Mac Giolla Phadraig C, Comiskey C, Guerin S, van Harten MT, Donnelly-Swift E, Clarke MJ. Oral hygiene interventions for people with intellectual disabilities. Cochrane Database Syst Rev. 2019;5:CD012628. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 43] [Article Influence: 7.2] [Reference Citation Analysis (0)] |
| 23. | Hua F, Xie H, Worthington HV, Furness S, Zhang Q, Li C. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev. 2016;10:CD008367. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 87] [Cited by in RCA: 129] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 24. | Shi Z, Xie H, Wang P, Zhang Q, Wu Y, Chen E, Ng L, Worthington HV, Needleman I, Furness S. Oral hygiene care for critically ill patients to prevent ventilator-associated pneumonia. Cochrane Database Syst Rev. 2013;CD008367. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 25. | Men XC, Du XP, Ji Y. Effects of personalized oral hygiene management on oral health status of pregnant women. World J Clin Cases. 2024;12:4566-4573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 26. | George A, Sousa MS, Kong AC, Blinkhorn A, Patterson Norrie T, Foster J, Dahlen HG, Ajwani S, Johnson M. Effectiveness of preventive dental programs offered to mothers by non-dental professionals to control early childhood dental caries: a review. BMC Oral Health. 2019;19:172. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 46] [Cited by in RCA: 57] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 27. | Moliner-Sánchez CA, Iranzo-Cortés JE, Almerich-Silla JM, Bellot-Arcís C, Ortolá-Siscar JC, Montiel-Company JM, Almerich-Torres T. Effect of per Capita Income on the Relationship between Periodontal Disease during Pregnancy and the Risk of Preterm Birth and Low Birth Weight Newborn. Systematic Review and Meta-Analysis. Int J Environ Res Public Health. 2020;17:8015. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 13] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 28. | Teshome A, Yitayeh A. Relationship between periodontal disease and preterm low birth weight: systematic review. Pan Afr Med J. 2016;24:215. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 71] [Cited by in RCA: 69] [Article Influence: 7.7] [Reference Citation Analysis (0)] |