Published online Aug 26, 2025. doi: 10.12998/wjcc.v13.i24.107233
Revised: April 19, 2025
Accepted: May 13, 2025
Published online: August 26, 2025
Processing time: 89 Days and 19 Hours
Traumatic cloacal deformities are a result of major obstetric injury and usually happens after a fourth-degree perineal laceration. This is characterized by com
We present a case of unmarried 15-year female, who developed hematometra and was diagnosed as cervical ostia obstruction at the age of 12 year. She underwent drainage of hematometra, and later some abdominal and perineal procedures elsewhere and subsequently developed fecal discharge from the vagina. Examina
This case report highlights expert management of a case of mismanaged benign gynaecological condition in a young female that resulted in lifelong impairment of the patient's quality of life following hysterectomy and salpingo-oophorectomy, leading to the development of a common cloaca.
Core Tip: This rare and unusual case highlights the mismanagement of hematocolpometra in a child and its subsequent complication in the form of iatrogenic cloaca. Here the authors discuss the management of this patients in details, and review the literature on surgical management of iatrogenic cloaca.
- Citation: Balani L, Kumar A. Iatrogenic cloaca: A case report. World J Clin Cases 2025; 13(24): 107233
- URL: https://www.wjgnet.com/2307-8960/full/v13/i24/107233.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i24.107233
Iatrogenic cloacal deformities represent a severe yet rare clinical challenge. Post intervention formation of cloaca is similar as common cloacal deformity of infancy. It is demonstrated clinically as a common channel incorporating the genitouri
A 15-year-old female patient presented with passage of mucous discharge per vagina for one year duration following drainage of colpohematometra and multiple surgeries elsewhere.
At 12 years of age, a female patient had complaints of lower abdomen pain and amenorrhoea. On evaluation with USG abdomen, she was found to have cervical ostia obstruction and hematometra. She then underwent perineal evacuation of blood clots. A few days later, following surgery, she started passing faeces and flatus per vagina. This was managed by proximal diversion colostomy. For persistent menstrual symptoms, she underwent multiple sessions of drainage of hematometra followed by total abdominal hysterectomy and bilateral salpingo-oopherectomy and attempted repair of perineal deformity elsewhere before being referred to us. The main presenting symptom was passage of mucous discharge per vagina with stoma in situ in left iliac fossa.
No significant history of chronic illness.
Not contributory.
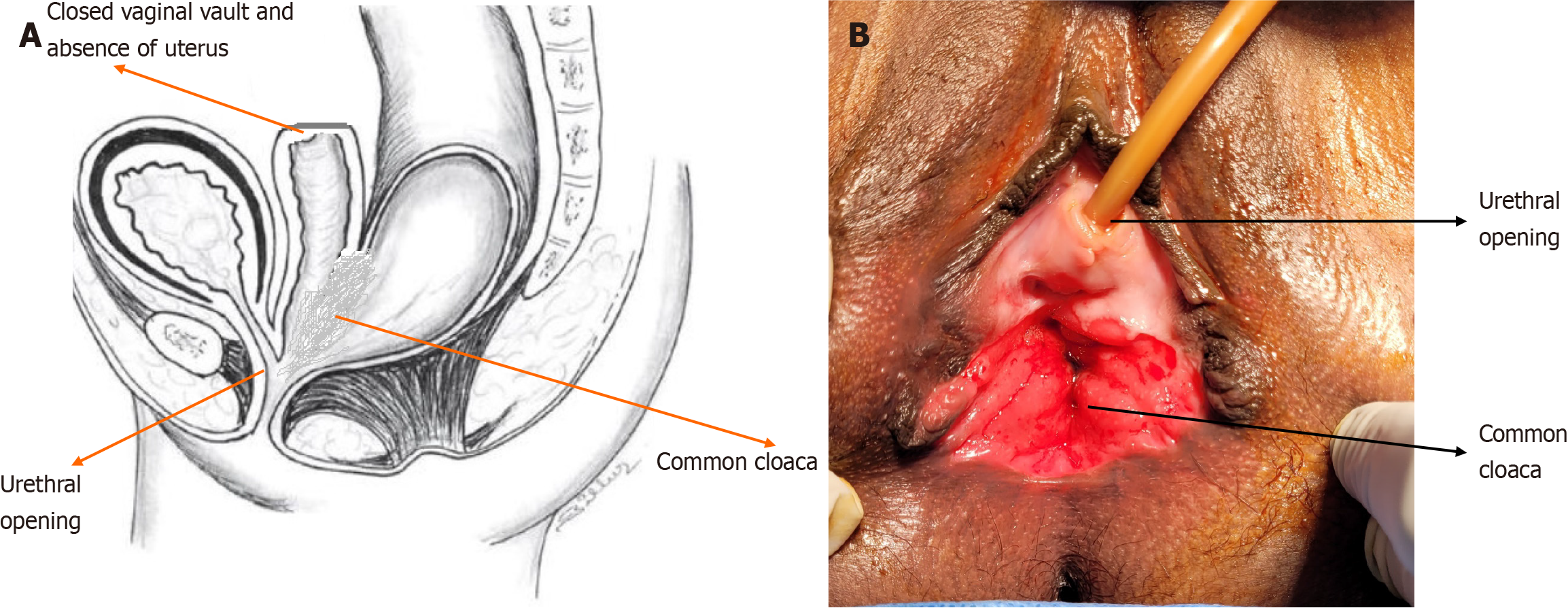
Perineal examination revealed absent anterior wall of anorectum and rectovaginal septum with single cavity of vagina and anal canal (common cloaca, Figure 1). The urethral opening was present anteriorly in the vaginal wall.
All required laboratory investigations done were within normal limits.
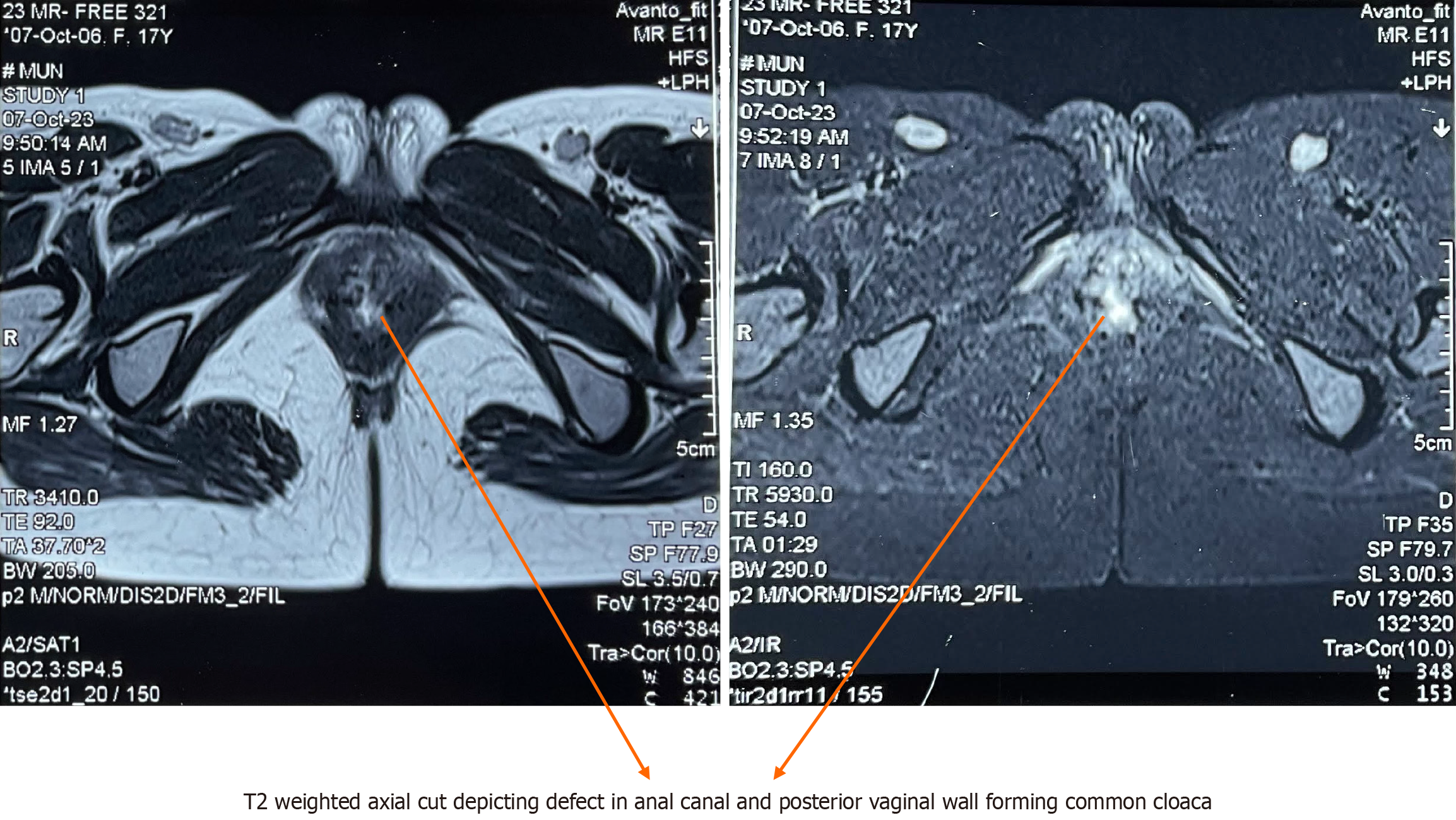
Magnetic resonance imaging (MRI) pelvis revealed absence of uterus and bilateral ovaries with defect in anterior wall of anal canal and lower rectum involving half circumference of the internal and external sphincter anteriorly. Posterior wall of vagina was absent suggestive of common cloaca (Figure 2).
Iatrogenic common cloaca.
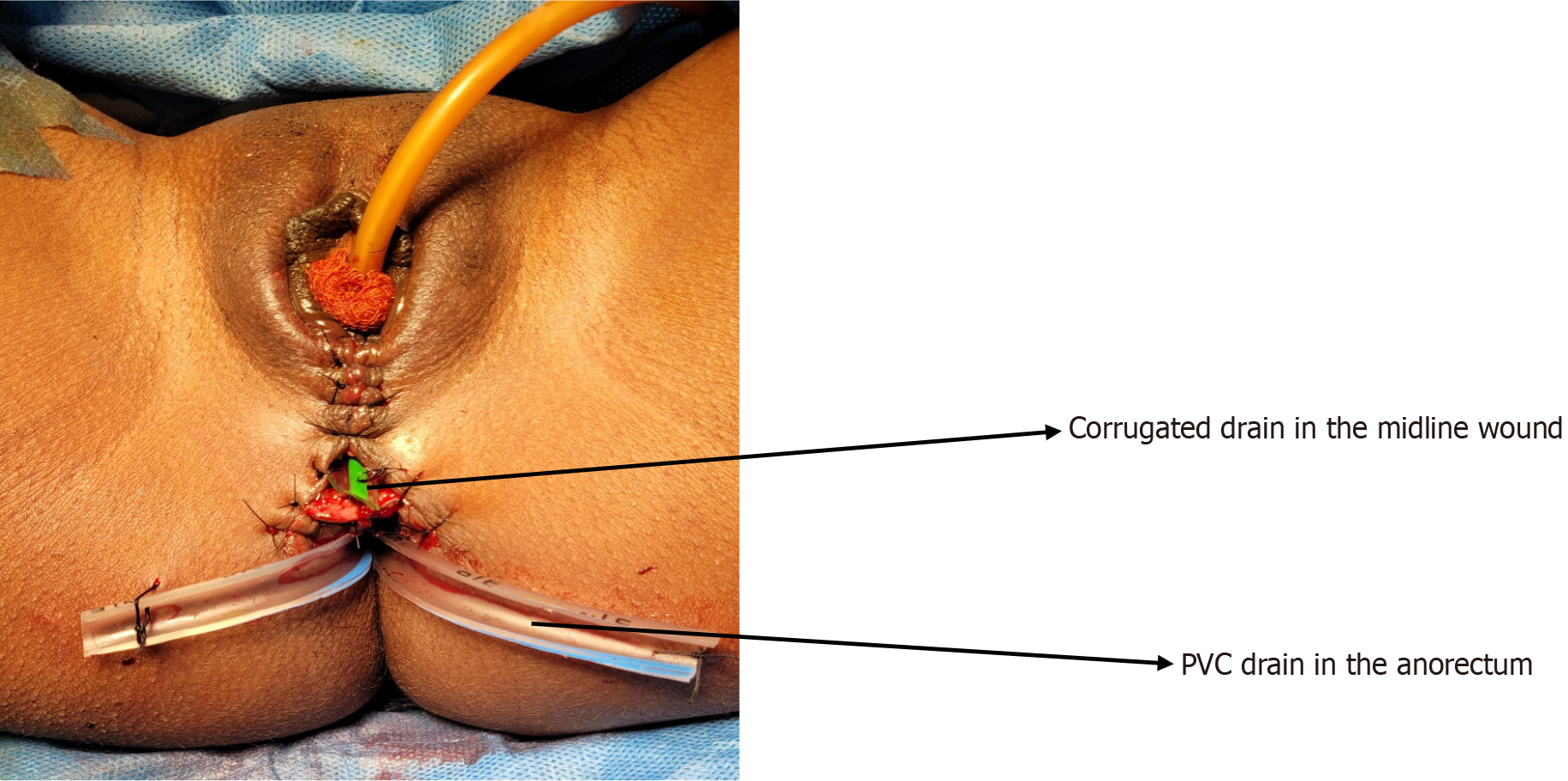
She was taken up for surgery after discussion and counselling regarding the surgical procedure with the patient and her parents. Surgical procedure involved anorectoplasty, vaginoplasty, sphincteroplasty and levatorplasty. Surgery was performed in lithotomy position in regional anaesthesia under antibiotic coverage (Injection Cefuroxime and metroni
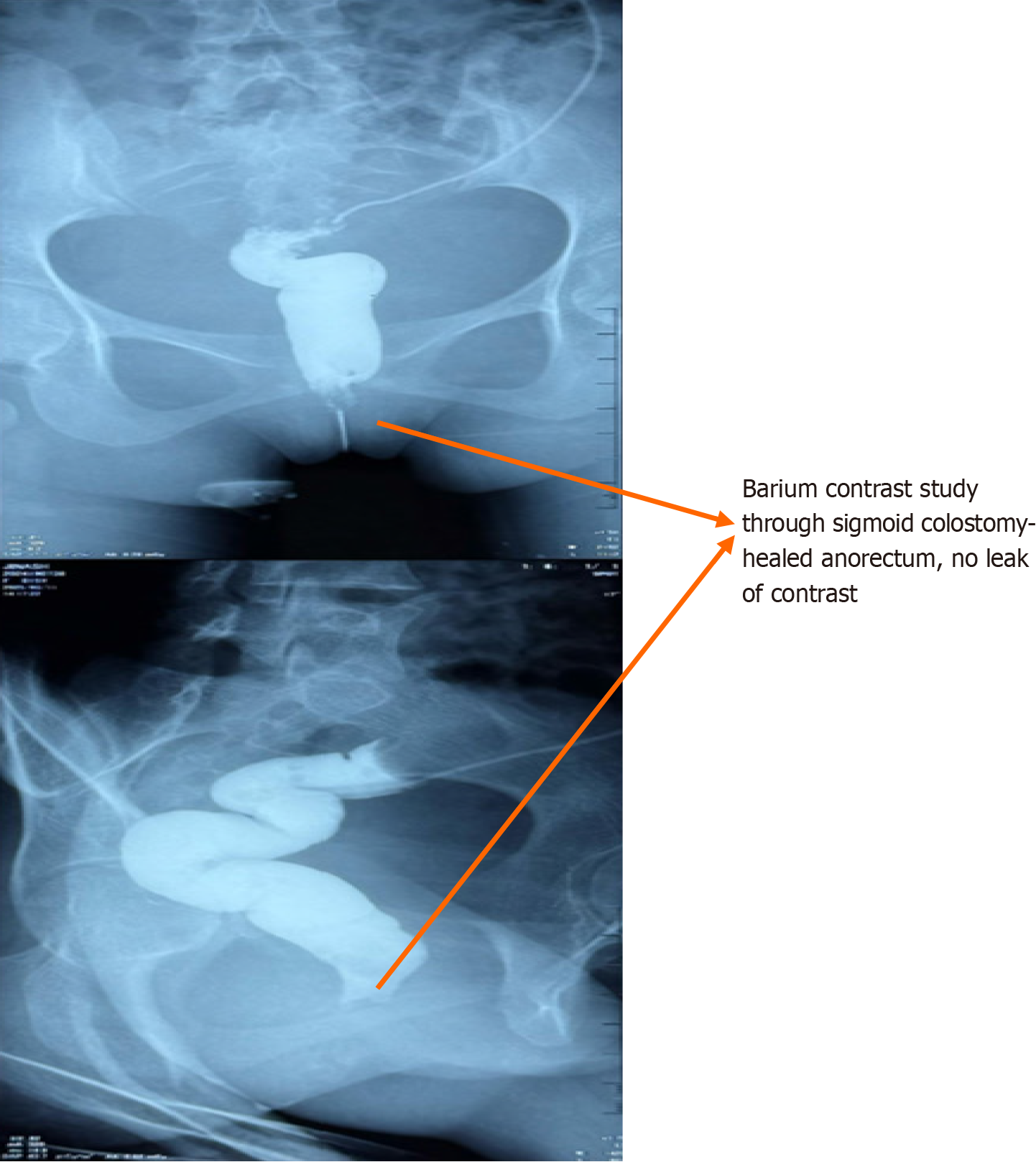
Postoperative course was uneventful. Drain was removed on POD5 and patient was discharged on POD7 without any complication. On two months follow up she is asymptomatic with well healed anorectum (Figures 4 and 5).
Iatrogenic cloacal deformities typically result from obstetric injuries. The high-risk factors reported are operative vaginal deliveries with use of forceps, primiparity, large foetal weight, and median episiotomies. Other cause of such deformity occurs during any perineal procedure for gynaecological pathology as was evident in this case[3].
Accurate diagnosis involves physical examination and imaging modalities. Most commonly used modality is MRI, anorectal ultrasound which provides valuable insights into structural abnormalities of anal sphincter complex, assisting in preoperative planning. Another novel modality used in complex cloacal malformations is rotational fluoroscopy with 3D reconstruction facilitates diagnostic accuracy of complex anatomy and preoperative surgical planning[4].
Functional assessment of anal sphincter is assessed with anorectal manometry. This is not mandatory preoperatively but helps in assessing the faecal continence functional outcome in postoperative period. Further, Clinical scoring systems like the Wexner incontinence score and quality-of-life assessments are crucial for evaluating symptom severity and tracking postoperative improvements.
Management of iatrogenic cloacal deformity is found to be more challenging compared to traumatic due to multiple attempted interventions followed by traumatic inflammatory changes leading to fibrosis of the tissues and disturbed anatomical planes. Therefore, attempt to definitive repair should be postponed to at least 3 months or when the local inflammation subsides[5]. Approaches for reconstruction can be perineal, abdominal or posterior sagittal, but the most preferred in iatrogenic deformity have been reported to be perineal approach. Pena and Hendren were the two pioneers who had reported multiple management strategies for congenital common cloaca according to the length of common cloaca and associated anomalies[6,7].
Since, there is no standard procedure described yet for management of iatrogenic cloaca, its management principles are followed similar to the congenital cloacal malformation which is based on length of common cloaca[8]. He has described posterior sagittal approach for mobilizing anterior rectal wall and posterior vaginal wall followed by vaginoplasty and anoplasty for common channel shorter than 1 cm. For common channel length between 1 and 3 cm, he added the need of total urogenital mobilisation before repair via posterior sagittal approach. With increase in length of common channel, he advised for combined posterior sagittal and transabdominal approach for adequate mobilisation. In case of inadequate tissue for vaginal repair, vaginal switch[9] or vaginal replacement with rectum, sigmoid or small bowel was suggested. Similar approach can be applied for management of iatrogenic cloaca considering the extent of injury to rectovaginal septum.
The repair process described, consists of three major steps. The first step, as described by Penna[6] for the correction of congenital cloaca, involves the dissection of the rectovaginal septum to separate the rectal and vaginal walls, along with the reinforcement of the sphincters. This step begins with the injection of adrenaline saline into the rectovaginal plane, followed by a transverse, curvilinear, or X-shaped incision on the perineal skin at the anovaginal septum[10]. The dissection plane is then deepened between the vaginal and rectal walls, extending laterally into the ischiorectal fossa and cranially up to the levator ani. Care must be taken to avoid the inadvertent creation of buttonholes in either mucosa.
The second step focuses on the identification and mobilization of the sphincter complex muscles, which include the internal and external anal sphincters and the levator ani muscle. Mobilization is performed from lateral to medial, beginning in the para-rectal space. The sphincter complex is then approximated or overlapped, with concurrent recon
The third and final step involves the formation of the perineal body by approximating the puborectalis and transverse perineal muscles, along with the repair of the anorectal and vaginal mucosa. This strengthens the pelvic floor and reconstructs the neovagina and anal canal. Various methods for vaginal reconstructed for congenital cloacal deformity are tabulated in Table 1, as described by Peña[6], which can be applied equally in iatrogenic cloaca also. If the puborectalis muscle is inadequate for approximation, a bulbocavernosus (Martius) or gracilis muscle flap can be used for perineal body reconstruction. Vaginal mucosal replacement may also be performed using rectal, colonic, or small bowel tissue in cases where native mucosa is insufficient. Skin closure can be achieved through simple approximation or the use of skin flaps (e.g., island or lotus petal flaps)[11,12]. Alternatively, partial wound closure may be employed to allow fluid drainage and secondary intention healing, which has been associated with a reduced risk of wound infection.
| 1. For vaginal pull through | Total urogenital mobilisation |
| Vagino-urethroplasty | |
| 2. For vaginal replacement | Rectum |
| Small bowel | |
| Colon | |
| 3. Flaps | Vaginal flap |
| Skin/Labial flap | |
| 4. Vaginal switch |
The role of a Defunctioning stoma remains controversial. Proponents argue that diverting faecal matter from the suture site reduces the risk of infection, wound dehiscence and allows optimal healing of the sutured muscles by preventing stool passage through the anal canal. However, there is no evidence of benefit of routine defunctioning stoma. In a retrospective study[13], author has shown similar rates of perineal wound dehiscence in patient with and without defunctioning stoma with higher rates of stoma related complications along with need of second surgery in patients with defuncting stoma. Rather, most of the surgeons have used alternative options for avoiding perineal wound dehiscence than stoma, like partial closure of wound with healing by secondary intent. Defunctioning stoma should be selectively used in case of complex cloacal deformity with multiple attempts of repair or significant faecal contamination.
Postoperative management includes adequate pain control with analgesics, prophylactic antibiotics, and restrictions on sitting or squatting to minimize strain on the surgical site. Regular inspection of the wound is essential to detect early signs of infection or dehiscence. Patients are typically discharged after 3 to 4 days, with a follow-up scheduled within 7 to 14 days to assess suture site healing, the presence of rectovaginal fistula, and faecal incontinence. Sexual activity should be avoided for at least three months to ensure proper healing.
The surgical repair/ reconstruction of cloacal type injury is not free from complications. The early complications include urinary retention, wound infection, wound dehiscence and surgical site hematoma. The most common early complication is wound infection, which can be managed conservatively with drainage and regular dressing. Similarly, surgical site hematoma also needed to be drained followed by regular dressing.
The late surgical complications include vaginal stricture/shortening, dyspareunia, anal stricture, fecal incontinence, development of rectovaginal or rectocutaneous fistula. Some patient may land up with complete failure of the recon
| Ref. | Age, gender/No. of patients | Aetiology | Clinical presentation | Examination | Evaluation | Operative procedure | Follow up |
| Ibrahim et al[14] | 45, F | Remote vaginal delivery | Postcoital bleed, faecal urgency, NO faecal incontinence | Grade 4 perineal tear, Absent perineal body, receding post vaginal wall, no anterior anal sphincter | Manometry- diminished IAS and EAS pressure, hypersensitivity of rectal sensation, RAIR+ | Sphincteroplasty (overlapping), levatoroplasty, vaginoplasty, perineal body reconstruction, rectocele repair | 6 months- no faecal incontinence |
| Balmaceda et al[1] | 17, F | Vaginal delivery-7 days (high BW, forcep usage) | Anal incontinence, vaginal discharge | Hypotonic sphincter, disruption of anterior rectoanal wall and perineal body, lower middle third of rectovaginal septum, vaginal mucosa | EUS- anterior defect of IAS+EAS | Sphincteroplasty (overlapping), anoplasty, perineal body repair, vaginoplasty | Postop- perianal subcutaneous fistula- healed spontaneously. Six months- good continence |
| Stavros et al[15] | 39, F | 3 years after vaginal delivery | Common cloaca | Absent perineal body, absent resting and squeeze pressure. | - | - | - |
| Venkatesh et al[16] | 44 | Obstetric injury (39), Others (5) | Faecal incontinence, recurrent infections | Anterior defect of IAS+EAS | Manometry and imaging | Sphincteroplasty, levatorplasty, and flaps | Improved continence in 39, incontinence to flatus in 4, incontinence to liquid and flatus in 1 |
| Haitham et al[17] | 30, F | Post primary repair of genital injury due to sexual assault | Stools per vagina | Rectovaginal fistula at 2 cm from anal verge. EAS intact | Fistula repair with diversion colotomy | Asymptomatic after 1 year of stoma reversal | |
| Spelzini et al[18] | 27, F | 2 year post vaginal delivery | Stool per vagina | Common cloaca | Rectovaginal septum repair, perineal body reconstruction | 2 years, asymptomatic | |
| Present case | 15, F | Mismanaged calpohematometra | Stool per vagina | Common cloaca | MRI | Anorectoplasty, vaginoplasty, sphincterplasty with levaterplasty and creation of rectovaginal septum | 2 months asymptomatic, waiting for colostomy closure |
In rare cases, the loss of the uterus and ovaries, as happened in our patient, have a significant impact on sexual and reproductive health, as well as psychosocial well-being. Even patients with intact reproductive organs may experience long-term issues such as irregular menstrual cycles, infertility, dyspareunia, and early menopause. This hormonal disruption may further increase the risk of cardiovascular disease, osteoporosis, and other hormone-related changes. To prevent the effect of hormonal disruption, expert opinions and follow up is advised regarding use of hormonal therapy and counselling.
Iatrogenic cloacal deformities are rare but debilitating conditions. This case highlights the mismanagement of hematocolpometra leading to iatrogenic cloaca and later attempted failed repair. It is better not to attempt repair if one is inexperienced but refer the patient to the expert centre for better outcome and quality of life. Since there is no standard protocol for its management, further research and collaboration are needed to develop a standardized protocols to improve long-term outcomes for affected patients.
| 1. | Balmaceda R, Galvarini M, Affroti L, Kerman J, Fermani C, Kerman A. Traumatic cloaca repair. Presentation of a case and review of the literature. Rev Argent Coloproct. 2022;33:132. [DOI] [Full Text] |
| 2. | Sieber WK, Klein R. Cloaca with non-adrenal female pseudohermaphrodism. Pediatrics. 1958;22:472-477. [PubMed] [DOI] [Full Text] |
| 3. | Goh JT, Tan SB, Natukunda H, Singasi I, Krause HG. Outcomes following surgical repair using layered closure of unrepaired 4th degree perineal tear in rural western Uganda. Int Urogynecol J. 2016;27:1661-1666. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 4. | Patel MN. Use of rotational fluoroscopy and 3-D reconstruction for pre-operative imaging of complex cloacal malformations. Semin Pediatr Surg. 2016;25:96-101. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 5. | Khanduja KS, Yamashita HJ, Wise WE Jr, Aguilar PS, Hartmann RF. Delayed repair of obstetric injuries of the anorectum and vagina. A stratified surgical approach. Dis Colon Rectum. 1994;37:344-349. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 36] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 6. | Peña A, Levitt MA, Hong A, Midulla P. Surgical management of cloacal malformations: a review of 339 patients. J Pediatr Surg. 2004;39:470-9; discussion 470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 129] [Cited by in RCA: 105] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 7. | Hendren WH. Cloaca, the most severe degree of imperforate anus: experience with 195 cases. Ann Surg. 1998;228:331-346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 114] [Cited by in RCA: 101] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 8. | Bischoff A. The surgical treatment of cloaca. Semin Pediatr Surg. 2016;25:102-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 36] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 9. | Bischoff A, Levitt MA, Breech L, Hall J, Peña A. Vaginal switch--a useful technical alternative to vaginal replacement for select cases of cloaca and urogenital sinus. J Pediatr Surg. 2013;48:363-366. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 17] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 10. | Kaiser AM. Cloaca-like deformity with faecal incontinence after severe obstetric injury--technique and functional outcome of ano-vaginal and perineal reconstruction with X-flaps and sphincteroplasty. Colorectal Dis. 2008;10:827-832. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 19] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 11. | Altomare DF, Rinaldi M, Bucaria V, Marino F, Lobascio P, Sallustio PL. Overlapping sphincteroplasty and modified lotus petal flap for delayed repair of traumatic cloaca. Tech Coloproctol. 2007;11:268-270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Draganic B, Solomon MJ. Island flap perineoplasty for coverage of perineal skin defects after repair of cloacal deformity. ANZ J Surg. 2001;71:487-490. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 13. | Hollingshead JR, Warusavitarne J, Vaizey CJ, Northover JM. Outcomes following repair of traumatic cloacal deformities. Br J Surg. 2009;96:1082-1085. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 14. | Ibrahim N, Igdoura N, Chou Q. 216 surgical repair of an obstetric traumatic cloacal defect. Continence. 2022;2:100305. [DOI] [Full Text] |
| 15. | Stavros S, Papapanagiotou IK, Zacharakis D, Migklis K, Mantzioros R, Domali E, Chatzipapas I, Drakakis P, Rodolakis A. Cloacal type defect of the anal canal following an obstetric anal sphincter trauma. Clin Case Rep. 2021;9:e04309. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Venkatesh KS, Ramanujam P. Surgical treatment of traumatic cloaca. Dis Colon Rectum. 1996;39:811-816. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 18] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 17. | Torky HA, El-Sayed AA, Saleh WF. Iatrogenic recto-vaginal fistula as a late consequence of failed primary repair of genital injury caused by sexual assault. Int Urogynecol J. 2017;28:1843-1844. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 18. | Spelzini F, Frigerio M, Manodoro S, Verri D, Nicoli E, Milani R. Repair of a traumatic cloaca after obstetric anal sphincter injury. Int Urogynecol J. 2016;27:495-497. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |