Published online Aug 26, 2025. doi: 10.12998/wjcc.v13.i24.106459
Revised: April 10, 2025
Accepted: May 8, 2025
Published online: August 26, 2025
Processing time: 109 Days and 22.8 Hours
Osteochondroma of the hand and phalanges is rare. Although rare, solitary phalangeal osteochondromas can result in pain, cosmetic deformity, compression of nearby neurovascular structures and tendons, or functional limitation of adjacent joints that warrant surgical correction when symptomatic. At times, involvement of the growth plate by juxtaepiphyseal exostosis can cause angu
We reported a case of a 3-year-old female with a right-sided painless deformity of the index finger along with swelling over the base of the index finger and its management.
This case report focused on the natural history of phalangeal exostosis and its association with angular deformities of the fingers. We demonstrated that the timely excision of the juxtaepiphyseal exostosis would allow the surgeon to achieve acute correction of the angular deformity with full functional recovery without recurrence at the 2-year follow-up. Significant delay of excision until skeletal maturity might necessitate corrective osteotomy of the finger deformity and tendon release for intrinsic tightness.
Core Tip: This case report focused on the natural history of phalangeal exostosis and its association with angular deformities of the fingers. We demonstrated that the timely excision of the juxtaepiphyseal exostosis would allow the surgeon to achieve acute correction of the angular deformity, improvement of hand function, and unimpeded development of fine and gross motor skills. Significant delay of excision until skeletal maturity might necessitate corrective osteotomy of the finger deformity and tendon release for intrinsic tightness. Despite complete excision in pediatric patients, close follow-up is required for the progression of deformity and recurrence. Our patient attained full functional recovery and deformity correction and no recurrence at the 2-year follow-up.
- Citation: Vanapalli R, Mlv SK, Ansari MT. Rare phenotype of juxtaepiphyseal osteochondroma of the proximal phalanx and its management: A case report. World J Clin Cases 2025; 13(24): 106459
- URL: https://www.wjgnet.com/2307-8960/full/v13/i24/106459.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i24.106459
Osteochondroma is a cartilage-capped bony overgrowth with corticomedullary continuity of the underlying bone. It typically arises during the growth phase and continues to grow until skeletal maturity. Most of the osteochondromas of the hand originate from the distal part of the metaphysis of the metacarpals or the proximal part of the proximal phalanx and very rarely from the carpal bones[1-4]. They are clinically asymptomatic and may cause impingement of neu
A 3-year-old female presented with a right-sided painless deformity of the index finger along with swelling over the base of the index finger (Figure 1).
The swelling and deformity were insidious in onset and progressive over the 6 months prior to presentation without any pain. There was no history of trauma or similar complaints elsewhere.
No significant past history.
No significant personal and family history.
On examination there was a painless mass on the ulnar side of the base of the proximal phalanx, which had gradually increased in size over 6 months. There was no significant history of trauma to the finger. There was a volar subluxation of the second metacarpophalangeal (MCP) joint and 30-degree flexion deformity of the proximal interphalangeal joint, with radial deviation of the index finger. The index finger was also found to be supinated by 10 degrees. The radial angulation was attributed to the mass effect over the ulnar aspect and subluxation of the MCP joint. The flexion deformity of the proximal interphalangeal joint was secondary to volar subluxation. There was no significant shortening of the phalanx or the index finger. The nail bed appeared to be normal. The skin over the swelling was thick, but there were no signs of inflammation.
The blood investigations were within normal limits.
Radiological examination showed volar subluxation of the second MCP joint due to mass effect with irregular bony overgrowth from the ulnar aspect of the proximal phalanx of the index finger extending inferiorly towards the second metacarpal bone (Figure 2). Subsequent magnetic resonance imaging revealed a widened base of the proximal phalanx with minimal contrast enhancement on structured time-dependent inverse regression images. However, the rest of the phalanges of the index finger and second metacarpal were normal in morphology and signal intensity.
The diagnosis was suggestive of juxtaepiphyseal osteochondroma of the proximal phalanx with deformity and surgical correction was opted considering the child’s age, along with the size of the exostosis, severity of the deformity, and subluxation of the joint.
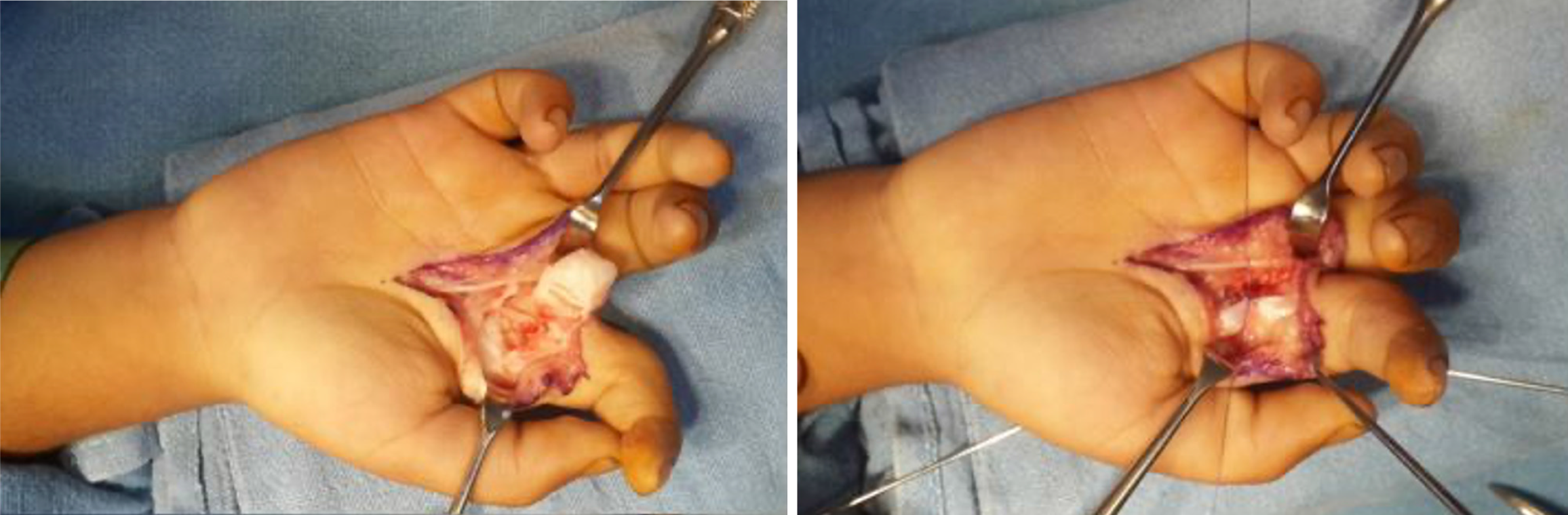
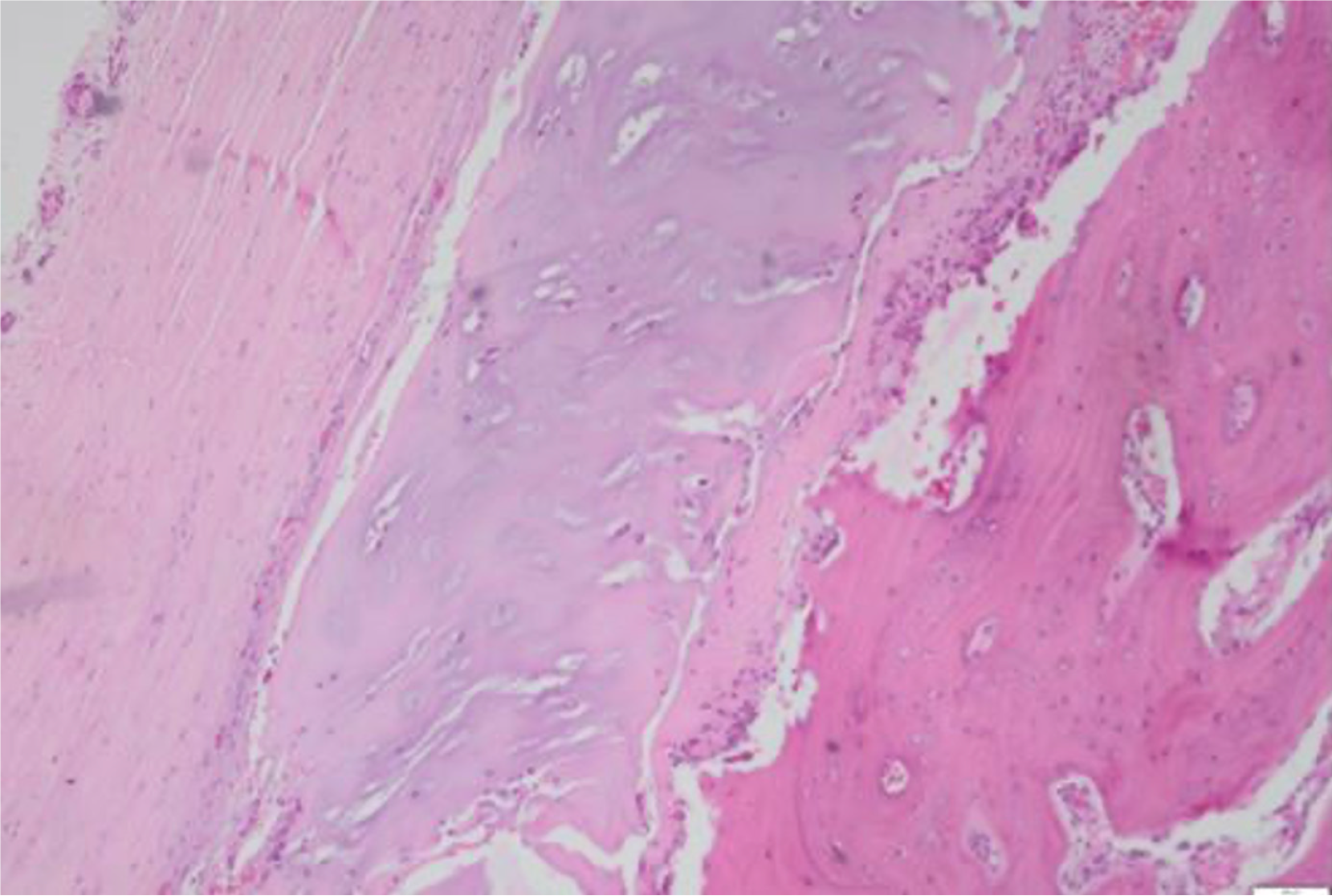
The excisional biopsy (Figure 3) of osteochondroma was planned under general anesthesia using a palmar approach to reach the second MCP joint. Radial and ulnar neurovascular bundles were secured. The A1 pulley was found to be tight, adhered over the flexor digitorum superficialis (FDS) and meticulously released. There was underlying tenosynovitis of long flexors (FDS) secondary to volar subluxation of the MCP joint and mass effect, eventually contributing to the flexion deformity of the proximal interphalangeal joint. The tendon of FDS was retracted radially. The base of the exostosis was separated from the parent bone with a bone cutter, and the mass was sent for histopathological examination. The volar plate was inspected and found to be intact. The MCP joint was reduced, and full extension of the index finger was tested by tenodesis effect with maximal wrist flexion and ensuring complete release of the A1 pulley. The deformity was corrected acutely by pronating the index finger into the anatomical position and reducing the second MCP joint, which was stabilized with two cross K wires (Figure 4). A volar slab was applied to support the fixation and to maintain the reduction. The excisional biopsy specimen was subjected to pathological examination, which revealed fibrocartilagenous elements characteristic of exostosis (Figure 5).
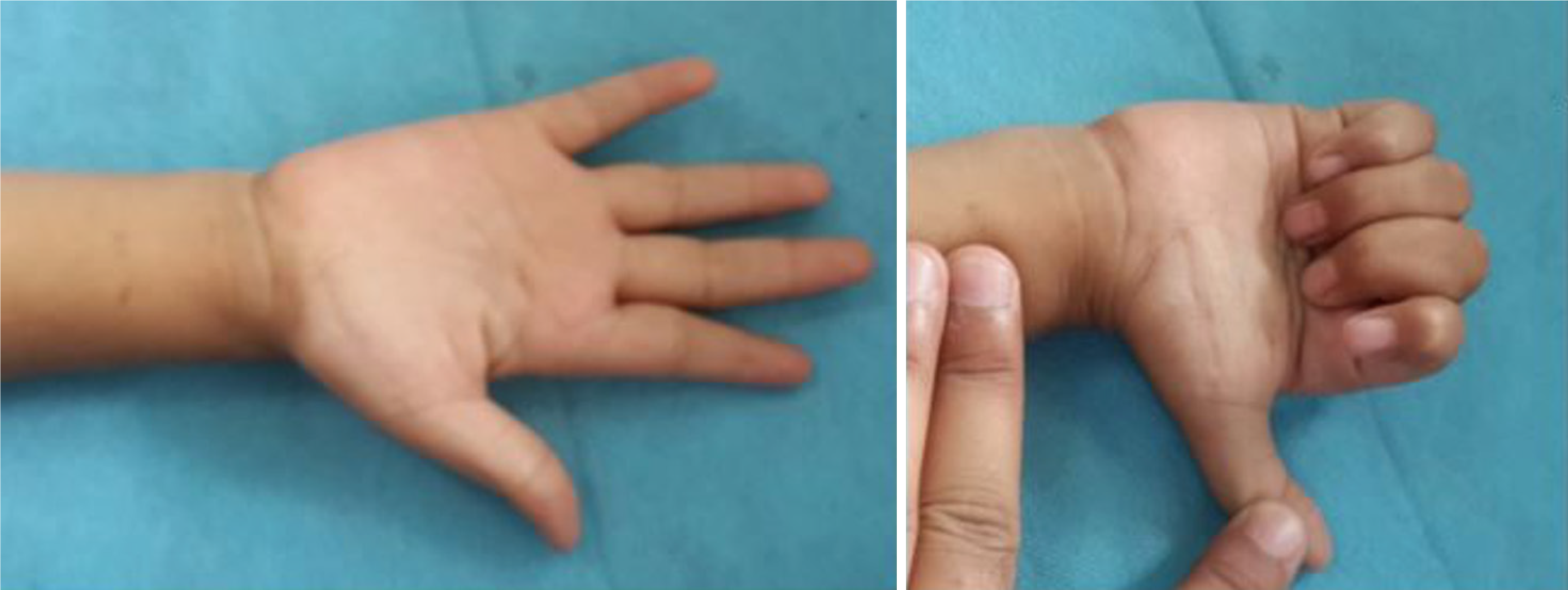
The volar slab was discontinued, and K wires were removed after 4 weeks. Physical therapy included passive tendon gliding exercises, opening and closing the hand, and finger stretching exercises. The child was encouraged to continue using her right dominant hand while playing and taught active exercises during each follow-up visit. The child was followed up regularly for 2 years with a strict physical therapy protocol. At the end of the 2-year follow-up, grip strength was adequate (Figure 6), and there was no evidence of clinical or radiological recurrence (Figure 7).
The hand is a common location for osteochondroma in multiple hereditary exostoses patients and is a rare site for solitary osteochondromas. In patients with multiple hereditary exostoses, they are known to cause deformities of the forearm and hand, and when in isolation, they have been described to cause symptoms due to pressure effects. Rimmer et al[2] described scaphoid osteochondroma with radio carpal arthritis due to impingement with the radial styloid process. Spinner et al[3] published a case report of superficial radial nerve compression caused by scaphoid exostosis. Koshi et al[4] described a rare case report of solitary osteochondroma of a trapezium with trapeziometacarpal arthrosis. All of the above cases were managed successfully with excision. Shah et al[5] reported a case of capitate exostosis causing rupture of the extensor digiti minimi tendon due to attrition. The patient presented with dorsal wrist pain managed by surgical excision of the tumor and side-side tendon transfer of residual distal stump of extensor digiti minimi.
Solitary osteochondroma is even rarer in phalanges. Although rare, solitary phalangeal osteochondromas can result in pain, cosmetic deformity, compression of nearby neurovascular structures, tendons or functional limitation of adjacent joints and warrant surgical correction when symptomatic. At times involvement of the growth plate by juxtaepiphyseal exostosis can cause angulation deformity, necessitating corrective osteotomy. The hand is a common location of exostosis development in patients with an autosomal dominant syndrome called multiple hereditary exostosis (MHE). MHE causes a spectrum of pathologies, the most common of which is a deformity of the forearm and hand, but at times the only presenting symptom in a child can be a simple trigger finger. Bizarre parosteal osteochondromatous proliferation[6], Nora’s lesion, turret exostosis, and heterotopic ossification are the possible differentials to be considered in the case of phalangeal osteochondroma. We have discussed the possible presentations, management options, and eventual outcome on various presentations of phalangeal osteochondroma in the literature (Table 1).
| No. | Ref. | Location | Age/sex | Presentation | Surgical procedure | Outcome |
| 1 | Salim et al[7] | Volar aspect of the proximal phalanx of left middle finger | 12/M | Painful range of motion. Restriction of flexion of MCP joint | En bloc excision | Painless full range of motion of MCP joint |
| 2 | Hayo et al[8] | Intra-articular; 7 patients: Solitary tumor; 1 patient: MHE | 2 females and 6 males, with a mean age of 5.74 years | Clinodactyly deformity | En bloc excision | Correction of deformity |
| 3 | Kwon et al[9] | Volar proximal part of proximal phalanx of left middle finger | 21/M | Trigger finger with flexion contracture of the PIP joint | En bloc excision + repair of A1 and A2 pulley with Z-plasty lengthening | Correction of locking and flexion contracture |
| 4 | Palaniswamy et al[10] | Radial aspect of middle phalanx of left 4th finger | 47/M | Recurrent tumor that was excised twice before | En bloc excision | No further recurrence |
| 5 | Al-Harthy et al[11] | Atypical osteochondroma of proximal phalanx of right ring finger | 5/F | Trigger finger with normal X rays | Excision of hidden osteochondroma | Asymptomatic after 2 months |
| 6 | Stern et al[12] | Dorsum of proximal phalanx of the right index finger | 4/F | Swan-neck deformity | En bloc excision | Asymptomatic after 3 months with full range of motion |
| 7 | Dieudonne et al[13] | Middle phalanx of the right index finger | 3 month/F | Radially deviated right index finger | En bloc excision at 22 months of age; lesion recurred at 4 years of age; Recurrent lesion was resected with a diagnosis of BPOP | No further recurrence noted |
| 8 | Yamamoto et al[14] | Proximal phalanx of right ring finger | 3/M | Swelling with minimally restricted extension | Spontaneous regression of the osteochondroma by the age of 10 years | Asymptomatic at 10 years of age |
| 9 | Yabumoto et al[15] | Middle phalanx of the right middle finger | 50/F | Atypical A3 pulley trigger finger | En bloc excision + repair of the pulley | No recurrence |
| 10 | Karr et al[16] | Proximal phalanx of the middle finger in a case of MHE | 18 month old child | Trigger finger | En bloc excision of the tumor with release of the pulley (A1 and initial part of A2) | Asymptomatic |
| 11 | De Oliveira et al[17] | 2 patients with MHE | 9/F, 13/F | Trigger finger | En bloc excision of the tumor with release of the pulley (A1 and initial part of A2) | At 6 months no triggering but residual flexion lag of 20°; Asymptomatic after 2 months |
| 12 | Ohnishi et al[18] | 10 patients (solitary) and 6 patients (MHE) | 0 to 9 years; 14 males and 2 females | Restricted range of motion of the adjacent joints and angular deformity | 14 patients underwent simple excision and in 3 patients osteotomy with excision of tumor | 2 patients had 30° degrees of residual restriction of range of motion; 2 patients 10° of residual angular deformity |
| 13 | Al Qattan et al[19] | Solitary multi lobed osteochondroma from the base of middle phalanx | 25/M | Restriction of range of motion of PIP joint | Marginal excision | Recovery of range of movement |
| 14 | Baek et al[20] | 10 patients with solitary osteochondroma | 8 were male and two female | Restriction of range of movement and deformity | Excision of mass and corrective osteotomy if required | Improvement in function |
| 15 | Yoshioka et al[21] | MHE | 1/M | Restriction of movement | Excision of the mass | Improvement in function |
Ohnishi et al[18] classified phalangeal osteochondromas into three types based on their location. Type A lesions are located at the nonepiphyseal side of the metaphysis, type B at the metaphysis on the epiphyseal plate side, and type C from the diaphysis of the phalanx. In our patient, the lesion was type B in nature.
Phalangeal osteochondromas were described to occur either as a solitary lesion or as a spectrum of MHE. In our patient, the swelling was solitary. The symptoms varied from swelling to restriction of range of movement[7,14,18,20], both of which were relieved post excision. In our patient swelling was one of the complaints in addition to the deformity. Deformity both in the sagittal as well as coronal plane have been described in the literature due to osteochondroma[8,12,13,18]. The osteotomy was performed in skeletally immature patients as well, and the outcomes were poor when there was preexisting arthritis.
In our patient, the deformity was corrected post-excision, and there was no need for an osteotomy for the same. The deformity in the coronal plane and the flexion deformity were corrected after the excision. In a few other case reports the only presenting complaint was trigger finger[9,11,15-17]. Juxtaepiphyseal exostosis of phalanges can result in angular deformity rather than disturbance in longitudinal growth and can be treated by simple excision of the osteochondroma, which can result in the correction of the deformity. A second stage osteotomy can be planned if the deformity persists or when the child attains skeletal maturity.
This case report focused on the natural history of phalangeal exostosis and its association with angular deformities of the fingers. We demonstrated that the timely excision of the juxtaepiphyseal exostosis would allow the surgeon to achieve acute correction of the angular deformity, improve hand function, and unimpede development of fine and gross motor skills. Significant delay of excision until skeletal maturity might necessitate corrective osteotomy of the finger deformity and tendon release for intrinsic tightness. Despite complete excision in pediatric patients, close follow-up is required for the progression of deformity and recurrence.
| 1. | Chan SY, Ip FK, Wong TC, Wan SH. Exostosis in the Hand: Case Series and Literature Review. JOTR. 2012;16:66-69. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 2. | Rimmer SG, Bhoora IG, Hooper G. Scaphoid exostosis and radio-carpal osteoarthrosis. J Hand Surg Br. 1995;20:741-744. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Spinner RJ, Spinner M. Superficial radial nerve compression due to a scaphoid exostosis. J Hand Surg Br. 1996;21:781-782. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 13] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 4. | Koshi H, Shinozaki T, Hosokawa T, Yanagawa T, Takagishi K. Solitary osteochondroma of the trapezium: case report. J Hand Surg Am. 2011;36:428-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 5. | Shah NR, Wilczynski M, Gelberman R. Osteochondroma of the capitate causing rupture of the extensor digiti minimi: case report. J Hand Surg Am. 2009;34:46-48. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Nora FE, Dahlin DC, Beabout JW. Bizarre parosteal osteochondromatous proliferations of the hands and feet. Am J Surg Pathol. 1983;7:245-250. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 236] [Cited by in RCA: 197] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 7. | Salim S, Boopathi K, Saravanan R. Solitary Phalangeal Osteochondroma in a 12-Year-Old. Eplasty. 2022;22:ic6. [PubMed] |
| 8. | Hao Y, Guo JC, Wang XL, Shao JF, Feng JX, He JP. Phalangeal Intra-Articular Osteochondroma Caused a Rare Clinodactyly Deformity in Children: Case Series and Literature Review. Front Endocrinol (Lausanne). 2021;12:677245. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 9. | Kwon HY, Kang HJ. Trigger finger due to phalangeal osteochondroma of an adult: A case report. J Orthop Surg (Hong Kong). 2020;28:2309499020969991. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 10. | Palaniswamy SS, Subramanyam P. Recurrent Intra Articular Osteochondroma of Left 4(th) Finger. Indian J Nucl Med. 2022;37:204-205. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 11. | Al-Harthy A, Rayan GM. Phalangeal osteochondroma: a cause of childhood trigger finger. Br J Plast Surg. 2003;56:161-163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Stern PJ, Phillips D. Phalangeal osteochondroma: an unusual cause of swan-neck deformity. J Hand Surg Am. 1986;11:70-73. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 13. | Dieudonne G, Monu J, Hicks D. BPOP in early childhood following resection of osteochondroma: report of a case. Emerg Radiol. 2024;31:435-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 14. | Yamamoto T, Kurosaka M, Mizuno K. Spontaneous resolution of a phalangeal solitary osteochondroma. J Hand Surg Am. 2001;26:556-558. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Yabumoto T, Endo T, Itoga R, Kawamura D, Matsui Y, Iwasaki N. Unique skin findings in a case of the A3 pulley trigger finger due to an osteochondroma. Jt Dis Relat Surg. 2024;35:249-253. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 16. | Karr MA, Aulicino PL, DuPuy TE, Gwathmey FW. Osteochondromas of the hand in hereditary multiple exostosis: report of a case presenting as a blocked proximal interphalangeal joint. J Hand Surg Am. 1984;9:264-268. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 11] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 17. | de Oliveira RK, Delgado PJ, Geist JG. Pediatric Trigger Finger due to Osteochondroma: A Report of Two Cases. Hand (N Y). 2017;12:99-105. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 18. | Ohnishi T, Horii E, Shukuki K, Hattori T. Surgical treatment for osteochondromas in pediatric digits. J Hand Surg Am. 2011;36:432-438. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 19. | Al-Qattan MM, Al-Marshad F, Al-Shammari J, Rafique A. A giant multi-lobed osteochondroma of the phalanx in an adult: A case report. Int J Surg Case Rep. 2017;31:10-13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 20. | Baek GH, Rhee SH, Chung MS, Lee YH, Gong HS, Kang ES, Kim JK. Solitary intra-articular osteochondroma of the finger. J Bone Joint Surg Am. 2010;92:1137-1143. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 21. | Yoshioka S, Hamada Y, Takata S, Takai H, Yasui N. An Osteochondroma Limiting Flexion of the Proximal Interphalangeal Joint in Hereditary Multiple Exostosis: a Case Report. Hand (N Y). 2010;5:299-302. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |