Published online Aug 6, 2025. doi: 10.12998/wjcc.v13.i22.107325
Revised: April 4, 2025
Accepted: April 16, 2025
Published online: August 6, 2025
Processing time: 50 Days and 15.5 Hours
Patients with paraplegia are vulnerable to ischial pressure ulcers. Surgical treatments often lead to complications such as seroma and infection, necessitating repeated interventions that increase surgical difficulty. This case report aimed to introduce a novel treatment strategy combining negative pressure wound therapy (NPWT) with a fenestrated Penrose drain to manage refractory seroma in patients with a history of ischial pressure ulcers.
A 63-year-old woman presented with soft tissue defects on the left ischium and right trochanter. After surgical debridement, an inferior gluteal artery perforator (IGAP) flap was used to reconstruct the left ischium. NPWT was applied at a setting of 75 mmHg on postoperative day 3 owing to the development of seroma, combined with a fenestrated Penrose drain to facilitate effective drainage of serous fluid. A 54-year-old man presented with a 4 cm × 2 cm ulcer on the left ischium after previous excision and flap coverage. After thorough debridement, the IGAP flap was elevated, and NPWT with a fenestrated Penrose drain was implemented immediately postoperatively at 75 mmHg to promote drainage. Both patients achieved a stable recovery without complications.
NPWT combined with a fenestrated Penrose drain placement is a promising strategy for addressing refractory seromas in cases of complex pressure ulcers.
Core Tip: Combining incisional negative pressure wound therapy (NPWT) with a fenestrated Penrose drain promotes wound healing and manages fluid accumulation in dependent areas. In paraplegic patients, the ischial area is particularly susceptible to fecal and urine contamination. This approach protects the ischial region from contamination and reduces the need for frequent dressing changes. The timing and pressure settings for NPWT can be flexibly determined based on flap circulation viability and accompanying procedures such as skin grafts. This report provides a reliable option for managing refractory seromas in cases of complex pressure ulcers.
- Citation: Kim S, Jeon HB, Kang DH. Negative pressure wound therapy with a fenestrated penrose drain for refractory seroma following ischial flap: A case report. World J Clin Cases 2025; 13(22): 107325
- URL: https://www.wjgnet.com/2307-8960/full/v13/i22/107325.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i22.107325
Pressure injuries, also known as bedsores, decubitus ulcers, and pressure ulcers, are localized injuries to the skin and soft tissues resulting from prolonged pressure and shear, typically over bony prominences[1]. The ischium is a common site of pressure injury, especially in paraplegic patients who use wheelchairs for extended periods[2]. Pressure ulcers can be treated conservatively or surgically with a flap, depending on the stage, size, bone involvement, and general condition of the patient[3]. Furthermore, treatments are expensive, involving both conservative and surgical management, and may require lengthy hospitalization[4]. Surgical treatment for pressure sores include excision of the ulcer, the underlying bony prominence, or the bursa, if present, followed by closure of the defect with a flap[5].
Seroma formation is a commonly reported complication resulting from the accumulation of serum in the internal spaces[6]. Seroma formation often leads to patient discomfort, increased probability of infection, wound dehiscence, and slower wound healing, thereby requiring further surgical intervention. Repetitive surgical reinterventions lead to scarring of the surrounding tissue and reduction of the available local tissue, which limits surgical options prior to flap surgery. However, for patients with recurrent pressure ulcers, despite increased surgical challenges, complication-free results are the optimal outcome.
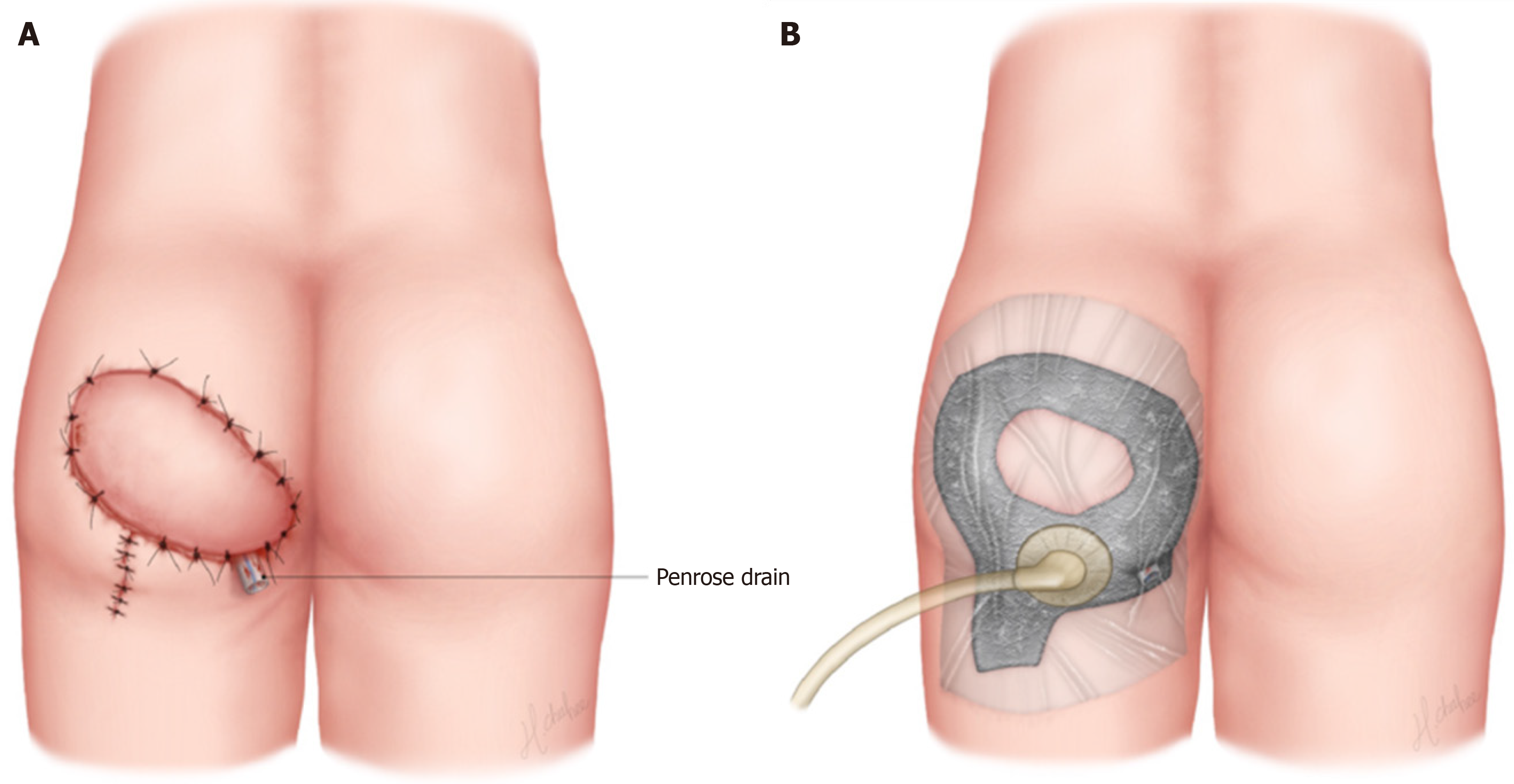
Here, we present a novel treatment strategy for refractory seroma after flap coverage of ischial pressure ulcers using negative-pressure wound therapy (NPWT) with a fenestrated Penrose drain (Figure 1).
The study was approved by the Institutional Review Board of Dankook University Hospital (IRB No.2025-03-025) and performed in accordance with the principles of the Declaration of Helsinki.
Case 1: A 63-year-old woman was referred to our tertiary hospital complaining of two recurrent pressure ulcers located at her previous surgical site.
Case 2: A 54-year-old male was referred to our tertiary hospital complaining of recurrent ulceration of the left ischium.
Case 1: Soft tissue defects (1.5 cm × 3 cm and 4 cm × 5 cm) were observed on the left ischium and right trochanter, respectively. The patient had previously undergone multiple flap surgeries for the left ischial wound, including a V-Y posterior thigh flap using the profunda femoris artery perforator and biceps femoris muscle flaps.
Case 2: The patient had previously undergone elliptical excision and local flap coverage for a left ischial wound at another local hospital. He then had a prolonged sedentary period and presented with a 4 cm × 2 cm wound dehiscence with a refractory seroma on the previous operation site.
Case 1: The patient underwent surgery due to spinal inflammation 40 years ago, which subsequently resulted in paraplegia. Other than paraplegia, her medical history is unremarkable.
Case 2: The patient underwent surgery for a spinal fracture sustained in a traffic accident 10 years ago, which subsequently resulted in paraplegia. His medical history is otherwise unremarkable, except for paraplegia and thoracolumbar scoliosis.
Cases 1 and 2: No significant personal or family history was reported.
Case 1: The soft tissue surrounding the left ischial wound exhibited scarring, and the ulcer had extended into deeper tissues, which indicated a pressure ulcer grade classification ≥ 3. Purulent discharge was observed in the malodorous wound. The right trochanter was covered with a dark eschar, and no discharge was observed.
Case 2: There was a 4 cm × 2 cm open wound on the left ischium with surrounding soft tissue scarring. A 3 cm undermining into the subcutaneous layer was noted, along with serous discharge. The wound bed was probed, and tested positive for bone.
Cases 1 and 2: The patient’s preoperative laboratory tests were within normal ranges.
Case 1: Computed tomography imaging revealed a 4.7 cm × 1.8 cm enhancing thick-walled fluid collection with internal free air and overlying skin thickening in the left ischium, along with ill-defined perilesional soft tissue densities in the subcutaneous fat layer of the left ischial area. On the right trochanter, an increased soft tissue density lesion was observed in the subcutaneous fat layer.
Case 2: Enhanced thick-walled fluid collection was observed in the left ischium, along with ill-defined perilesional soft tissue density.
Case 1: The patient was diagnosed with recurrent pressure ulcers on the left ischium and right trochanter.
Case 2: The patient was diagnosed with recurrence of pressure ulcers at the site of the previous left ischial flap.
Case 1: Surgical debridement of the necrotic tissue revealed a deep dead space in the left ischial tuberosity (Figure 2A) Conventional NPWT was performed 3 times per week for wound bed preparation. Thereafter, an inferior gluteal artery perforator (IGAP)-based fascio-cutaneous transposition flap on the left ischium and a V-Y musculocutaneous flap on the right trochanter were created using a Jackson-Pratt (JP) drain.
On postoperative day (POD) 3, serous fluid collection was observed in the dependent area of the left ischium, despite JP drainage. There were no signs of flap circulation changes, and the seroma was removed through the incisional margin. Subsequently, a cylindrical 6 mm Penrose drain, fenestrated to enhance fluid evacuation, was inserted with its distal end placed at the base of the dead space (Figure 2B). A portion of the NPWT foam dressing was cut to create a space where the opposite end of the fenestrated Penrose drain was positioned, such that additional serous fluid could be drained. The flap, including the incisional margin and fenestrated Penrose drain, was covered with a foam dressing and an adhesive film was attached to the surrounding skin for sealing. A conventional NPWT device (V.A.C., KCI USA, Inc., San Antonio, TX, United States) with a pressure of 75 mmHg in continuous mode was applied over the film to place negative pressure on the fenestrated Penrose drain (Figure 2C). The NPWT was changed at 2–3-day intervals, and fluid collection and flap circulation were evaluated each time the foam dressing was removed. On POD 14 the NPWT combined with a fenestrated Penrose drain was replaced with a conventional dressing (Mepilex® absorbent foam).
Case 2: Surgical debridement of the scar tissue and of chronic granulation tissue was performed, which revealed a deep soft tissue defect requiring flap coverage (Figure 3A). NPWT was applied for wound preparation and was changed at 2–3-day intervals. An 8 cm × 15 cm inferior gluteal artery perforator-based fasciocutaneous flap was elevated and transpositioned to cover the left ischial defect area sufficiently. Two JP drains were inserted into the base of the flap to prevent fluid collection. The donor site was closed directly from the distal margin and the remnant was covered with a split-thickness skin graft from the ipsilateral posterior thigh. A fenestrated Penrose tube drain was inserted through the margin into the left ischial tuberosity in the previously affected area (Figure 3B). The corresponding part of the NPWT foam dressing was excised to enable the drain to be positioned, and conventional NPWT with 75 mmHg in continuous mode was applied immediately, including the flap margin, a fenestrated Penrose drain, and skin graft (Figure 3C). Except for the incisional margin, a large window was created for the remaining flaps for serial monitoring. The NPWT was changed on POD 5, and there were no signs of wound complications, including flap failure, dehiscence, or hematoma. The NPWT was then replaced every 2–3 days. On POD 8, the NPWT with a fenestrated Penrose drain was removed and replaced with conventional dressing as the flap and skin graft had stabilized.
Case 1: The flap survived and healed completely, and the patient was discharged without complications. At 2-months follow-up, she remained complication-free (Figure 2D).
Case 2: The patient was discharged without complications. The surgical site remained stable during the 2-month follow-up period (Figure 3D).
NPWT is an effective option in wound management as it facilitates improved blood flow, wound contraction, and interstitial fluid removal[7,8]. The safety and efficacy of the prophylactic application of NPWT during surgery have been consistently confirmed, and incisional NPWT is particularly beneficial for patients with a higher baseline rate of wound complications[6,9]. We combined the incisional NPWT system with a fenestrated Penrose drainage to prevent seroma formation, which had occurred in previous surgeries despite the use of JP drainage. The lumen of a Penrose drainage tube consists of numerous fine grooves. These characteristics prevent the drainage tube from collapsing completely under negative pressure conditions and help maintain the negative pressure in the dependent area. Umezawa et al[9] reported that the NPWT system in addition to Penrose drainage effectively shortened the time spent waiting for fistulae to heal after head and neck or esophageal cancer surgery. Furthermore, as JP drains are not fixed in the internal spaces, it is possible for such drains to become displaced from the intended area, depending on a patient’s postoperative position. However, the Penrose drain involves a relatively straight drainage tube, usually vertically sutured at the incisional margin; therefore, the risk of displacement is minimal, and it has the advantage of targeting the intended high-risk area.
In the first case, we applied NPWT, including all flaps, given there were no signs of circulatory issues, other than seroma development on POD 3. In the second case, NPWT was applied immediately after flap coverage, and a wide window was created for flap monitoring. The timing of NPWT application can be determined as immediate or delayed depending on the flap circulation and whether there are other indications for immediate NPWT, such as skin grafting. If flap circulation is not stable or flaps need careful monitoring, it may be prudent to delay the application of NPWT or create a window for serial monitoring, as early detection of flap complications can improve the flap survival rate[10]
In both our patients, the ischial defect areas were reconstructed using IGAP fasciocutaneous flaps. The IGAP flap is an attractive surgical option for ischial reconstruction owing to its many advantages, including the ability to preserve peripheral muscle tissue, variability in flap design, relatively good durability, and a low donor site morbidity rate[2]. However, because the ischium is anatomically close to the anus and perineum, surgical wounds are vulnerable to fecal and urine contamination and require frequent dressing changes. Ischial ulceration is particularly common in paraplegic patients with fecal incontinence. Applying NPWT can prevent surgical wounds from contamination with feces and urine and has the advantage of fewer dressing changes.
Both patients were discharged without having experienced any major wound complications. However, during the maintenance period of NPWT, wound maceration was observed along the area covered with the NPWT foam dressing. Maceration improved spontaneously after replacing the NPWT dressing with conventional dressing. Umezawa et al[9] reported that contact dermatitis from taping was the only adverse event observed during NPWT using a Penrose drain after head and neck surgery.
Managing complicated wounds after previous reconstructive surgery is challenging, and treatment options are limited. Complicated surgery can lead to extended hospital stays and increased medical costs. In this challenging situation, NPWT combined with a fenestrated Penrose drain placement can be a useful option for treating recurrent ischial pressure ulcers with refractory seroma following flap coverage.
NPWT combined with a fenestrated Penrose drain is a promising strategy for treating refractory seroma in patients with complex pressure ulcers, reducing the need for repeated interventions and promoting faster recovery without complications.
| 1. | Mervis JS, Phillips TJ. Pressure ulcers: Pathophysiology, epidemiology, risk factors, and presentation. J Am Acad Dermatol. 2019;81:881-890. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 278] [Article Influence: 46.3] [Reference Citation Analysis (0)] |
| 2. | Kim YS, Lew DH, Roh TS, Yoo WM, Lee WJ, Tark KC. Inferior gluteal artery perforator flap: a viable alternative for ischial pressure sores. J Plast Reconstr Aesthet Surg. 2009;62:1347-1354. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 36] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 3. | Kumar U, Jain P. Infragluteal fasciocutaneous flap for management of recurrent ischial pressure sore. Indian J Plast Surg. 2018;51:70-76. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 4. | Keys KA, Daniali LN, Warner KJ, Mathes DW. Multivariate predictors of failure after flap coverage of pressure ulcers. Plast Reconstr Surg. 2010;125:1725-1734. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 77] [Cited by in RCA: 83] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Lee SS, Huang SH, Chen MC, Chang KP, Lai CS, Lin SD. Management of recurrent ischial pressure sore with gracilis muscle flap and V-Y profunda femoris artery perforator-based flap. J Plast Reconstr Aesthet Surg. 2009;62:1339-1346. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 38] [Cited by in RCA: 35] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 6. | Scalise A, Calamita R, Tartaglione C, Pierangeli M, Bolletta E, Gioacchini M, Gesuita R, Di Benedetto G. Improving wound healing and preventing surgical site complications of closed surgical incisions: a possible role of Incisional Negative Pressure Wound Therapy. A systematic review of the literature. Int Wound J. 2016;13:1260-1281. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 178] [Cited by in RCA: 157] [Article Influence: 17.4] [Reference Citation Analysis (0)] |
| 7. | Morykwas MJ, Argenta LC, Shelton-Brown EI, McGuirt W. Vacuum-assisted closure: a new method for wound control and treatment: animal studies and basic foundation. Ann Plast Surg. 1997;38:553-562. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1526] [Cited by in RCA: 1443] [Article Influence: 51.5] [Reference Citation Analysis (0)] |
| 8. | Park JH, Park JU. Flap monitoring with incisional negative pressure wound therapy (NPWT) in diabetic foot patients. Sci Rep. 2022;12:15684. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 9. | Umezawa H, Matsutani T, Yokoshima K, Nakamizo M, Ogawa R. A Novel Tube-Drainage Technique of Negative Pressure Wound Therapy for Fistulae after Reconstructive Surgery. Plast Reconstr Surg Glob Open. 2018;6:e1885. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 10. | Kim TH, Park JH. A novel negative pressure wound therapy (NPWT) monitoring system for postoperative flap management. Medicine (Baltimore). 2021;100:e27671. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |