Published online Jul 16, 2025. doi: 10.12998/wjcc.v13.i20.104609
Revised: March 8, 2025
Accepted: March 20, 2025
Published online: July 16, 2025
Processing time: 103 Days and 23.4 Hours
Proximal bile duct injury (BDI), which often occurs after laparoscopic cholecystec
A 39-year-old female had a routine LC in 2017. The patient sustained a proximal BDI during the surgery. In the months that followed, recurrent bouts of cholangitis occurred. A hepaticojejunostomy biliary reconstruction was performed in 2018. However, hepatic cholangitis persisted. In 2021 and 2022, MRCP scans revealed biliary stasis, duct dilation, and a stricture at the hepaticojejunostomy site. A subsequent percutaneous transhepatic cholangiography (PTC) confirmed these findings and led to drain placement. The treatment included internal and external biliary drain placements, repeated balloon dilations of the stricture, percutaneous transhepatic cholangioscopy to extract intrahepatic lithiasis, and insertion of a biodegradable biliary stent. Since the first PTC intervention, there have been no hospital admissions for cholangitis. Liver function tests showed improvement, and for five months following the biodegradable stenting, the condition remained stable. Long-term surveillance with regular imaging and blood work has been emphasized. The final diagnosis is recurrent biliary stricture secondary to proximal BDI. Treatment, including hepaticojejunostomy, repeated PTC with balloon dilation, and biodegradable biliary stenting, has led to complete drainage of the biliary system. Ongoing follow-up remains crucial for monitoring the patient's progress and maintaining their health.
This case demonstrated how strictures and recurrent cholangitis complicate the management of BDI after LC. A customized and multidisciplinary approach to control chronic biliary disease was proven effective, as shown by the patient’s good outcome. This was achieved by integrating balloon dilatation sessions, biliary drainage, stone clearing, and biodegradable stent placement. Long-term follow-up and continued monitoring remain essential to ensure patient stability and prevent further complications.
Core Tip: Effective management of recurrent biliary stricture following proximal bile duct injury requires a multidisciplinary approach, including timely surgical intervention, such as hepaticojejunostomy, and regular imaging using advanced techniques, such as magnetic resonance cholangiopancreatography. Incorporating innovative treatment modalities, such as biodegradable biliary stenting, can significantly improve patient outcomes by enhancing patency without the need for stent removal. Regular follow-up visits are crucial to assess stricture remodeling and prevent recurrence. Clinicians should remain vigilant for signs of cholangitis and be prepared to implement a combination of endoscopic and percutaneous interventions to ensure optimal management of complex biliary complications.
- Citation: Elsayed G, Mohamed L, Almasaabi M, Barakat K, Gadour E. Hepaticojejunostomy and long-term interventional treatment for recurrent biliary stricture after proximal bile duct injury: A case report. World J Clin Cases 2025; 13(20): 104609
- URL: https://www.wjgnet.com/2307-8960/full/v13/i20/104609.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i20.104609
Proximal biliary injury can often lead to complex biliary structuring disease and is most commonly managed by hepa
However, repairs performed by a nonspecialized hepatopancreatobiliary team frequently lead to results that are less than ideal[3]. Patients with hepaticojejunostomy strictures commonly present with recurrent cholangitis, occasionally accompanied by jaundice. Laboratory findings often reveal elevated levels of alkaline phosphatase and leukocytosis. Although ultrasound can detect intrahepatic bile duct dilation in 50% of cases, magnetic resonance cholangiopancreatography (MRCP) provides more precise imaging of strictures. However, in patients with nondilated bile ducts, factors such as pneumobilia and nearby intestinal loops, can obscure the diagnosis[4].
Antibiotics and percutaneous biliary drainage, which also validate the diagnosis of anastomotic stricture, are com
A 39-year-old woman underwent laparoscopic cholecystectomy (LC), which was complicated by proximal bile duct injury (BDI). Subsequently, she experienced recurrent episodes of cholangitis. She has been presenting to the hospital with typical symptoms of cholangitis, mainly abdominal pain and tenderness.
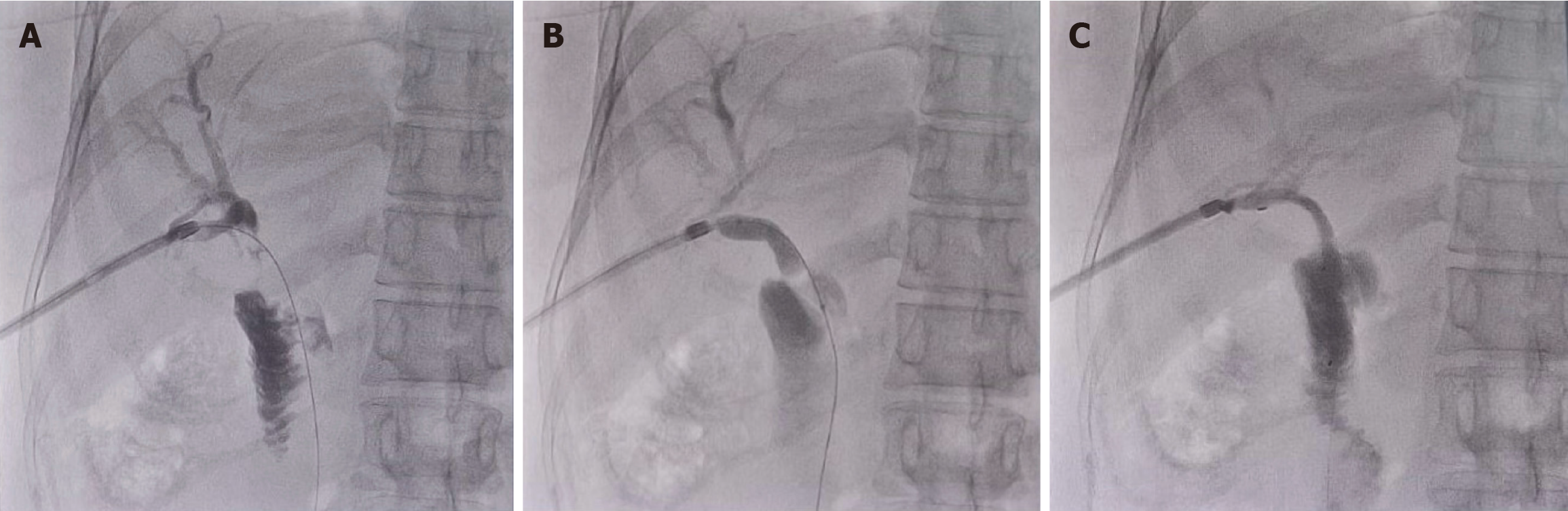
In 2018, she underwent hepaticojejunostomy biliary reconstruction, followed by prolonged T-tube drainage. Despite these interventions, the patient continued to experience multiple episodes of hepatic cholangitis, which were managed with repeated antibiotic courses and frequent hospital admissions. In December 2021, MRCP revealed postcholecystectomy biliary stasis, with dilation of the intrahepatic biliary radicals and a possible stricture at the hepaticojejunostomy site. A follow-up MRCP in October 2022 revealed further hepatic duct dilation and multiple filling defects in the common hepatic duct, suggesting stricture formation and obstruction at the hepaticojejunostomy site. Then the patient underwent an endoscopic retrograde cholangiopancreatography (ERCP) with cholangioscopy which confirmed the MRCP findings (Video 1). Immediate percutaneous transhepatic cholangiography (PTC) confirmed the diagnosis (Figure 1A) and facilitated placement of a 12-Fr internal/external biliary drain (Cook). Follow-up magnetic resonance imaging in October 2023 showed normal biliary drainage with minimal dilation of the biliary ducts and evidence of pneumobilia, suggesting a functioning biliary drain. Subsequent PTC revealed an ongoing 3-cm hepaticojejunostomy site stricture, which required balloon dilation up to 12 mm and persistent mid-balloon wasting (Figure 1B). A 12-Fr internal/external biliary drain (Cook) was then inserted for internal drainage.
In March 2024, another elective PTC showed with stricture, for which balloon dilatation using controlled radial expan
In August 2024, the patient underwent another PTC with anterograde biodegradable biliary stent insertion using three radiopaque markers at the proximal, middle, and distal portions of the biodegradable 11.8-Fr, 6-cm-long stent (SX/ELLA stent DV) (Figure 1C). To maximize stent drainage, in-stent balloon dilatation up to 6 mm was performed. Thereafter, anterograde diagnostic cholangiogram showed free flow of contrast through the stent lumen into the jejunal loops. Fluoroscopy confirmed satisfactory stent position. Since the first PTC intervention, the patient has had no documented hospital admission for cholangitis and achieved remarkable improvements in liver function tests (Table 1). She remained clinically and biochemically stable for 5 months after biodegradable biliary stenting. She will be followed-up during clinic visits and with blood testing every 3 months.
| Liver function test | Reference range/unit | October 9, 2024 | October 22, 2022 |
| Total bilirubin | < 21.0 μmol/L | 7.68 | 11.34 |
| Direct bilirubin | ≤ 5.0 μmol/L | 3.76 | 6.68 |
| Alkaline phosphatase | 35-104 U/L | 169 | 366.92 |
| Alanine aminotransferase | < 35 U/L | 61.40 | 19.39 |
| Aspartate aminotransferase | < 35 U/L | 41.50 | 23.65 |
| Albumin | 35.0-52.0 g/L | 41.80 | 24.04 |
| Protein | 64-83 g/L | 82.100 | 77.08 |
LC.
No family history of similar condition and no other personal history.
Physical examination was unremarkable except for mild abdominal tenderness. Vital signs were all normal throughout.
Table 1 shows laboratory examinations.
In December 2021 MRCP: Postcholecystectomy biliary stasis, dilation of intrahepatic biliary radicals, possible stricture at the hepaticojejunostomy site. In October 2022 MRCP: Further hepatic duct dilation, multiple filling defects in the common hepatic duct, stricture formation and obstruction at the hepaticojejunostomy site. In October 2022 PTC: Confirmed diagnosis of stricture at hepaticojejunostomy site. In October 2023 magnetic resonance imaging: Normal biliary drainage, minimal dilation of biliary ducts, evidence of pneumobilia. In October 2023 PTC: Ongoing 3-cm hepaticojejunostomy site stricture, mid-balloon wasting during balloon dilation. In March 2024 PTC: Persistent stricture, mid-balloon wasting during balloon dilation. In August 2024 PTC: Successful placement of biodegradable biliary stent, free flow of contrast through stent lumen into jejunal loops.
Recurrent biliary stricture secondary to proximal BDI.
Hepaticojejunostomy, repeated PTC with balloon dilatation, and ultimately biodegradable biliary stenting.
Complete drainage of the biliary system. Long-term follow-up with regular imaging and blood tests is essential to moni
This case clearly highlighted the complexities and challenges of managing a patient who developed a series of biliary complications after cholecystectomy. Despite multiple biliary interventions, our patient required biliary stenting to increase the chance of stricture remodeling. These complications can result in medical and financial burden to patients and healthcare providers. In this case, ERCP proved superior to PTC as a first-line approach due to its less invasive nature and ability to provide both diagnostic and therapeutic interventions in a single procedure. The successful use of ERCP for biliary drainage and stent placement demonstrated its efficacy in managing complex biliary strictures, avoiding the need for more invasive percutaneous techniques initially.
Advancements in laparoscopic surgical techniques and equipment have led to the use of LC as the preferred surgical technique for gallbladder removal. However, the increasing number of reported BDI as a complication of LC has become a major concern. Although a rare complication, BDI has been well documented to have incidence rates of 0.37% in Belgium, 0.42% in Italy, and 1.12% in China[8]. BDIs can significantly alter the postsurgical course and potentially lead to bile leak, bile duct stricture, and chronic cholangitis. Therefore, BDIs are linked to morbidity, mortality, and a significant financial burden on healthcare systems[9].
The postoperative management of BDI includes antibiotic prophylaxis for acute cholangitis, especially in the setting of predictable incomplete drainage. Management decisions can vary depending on the extent of BDI. In our patient, surgical treatment was chosen, because the bile duct continuity was completely destroyed. In particular, to restore biliary drai
This case highlighted several key considerations for treating patients with biliary complications after cholecystectomy. To identify and treat recurrent strictures and cholangitis, careful follow-up is essential. This patient required a range of interventions, from biliary drainage to refined endoscopic procedures; this highlighted the fact that multidisciplinary care involving gastroenterologists, interventional radiologists, and surgeons is crucial to optimize outcomes[10]. Moreover, as major improvements in the treatment of complicated biliary disorders, sophisticated imaging and minimally invasive procedures, such as biodegradable stenting and cholangioscopy, were performed on this patient. More clinical trials are required to evaluate the safety and efficacy of biodegradable stents in treating refractory biliary strictures. Furthermore, the persistence of the stricture despite several treatment modalities raised the likely need for even more creative methods, such as novel stent designs or therapeutic approaches, in the future. Regardless of the clinical results of biodegradable biliary stenting, patients should be offered long-term follow-up to ascertain the rates of real stricture remodeling and recurrence.
This case demonstrated how strictures and recurrent cholangitis complicate the management of BDIs after LC. A cus
| 1. | Dimou FM, Adhikari D, Mehta HB, Olino K, Riall TS, Brown KM. Incidence of hepaticojejunostomy stricture after hepaticojejunostomy. Surgery. 2016;160:691-698. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 64] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 2. | Dopazo C, Diez I, Quintero J, Curell A, González-Junyent C, Caralt M, Pando E, Lázaro JL, Molino JA, Juamperez J, Castells L, Pérez M, Bilbao I, Segarra A, Charco R. Role of Biodegradable Stents as Part of Treatment of Biliary Strictures after Pediatric and Adult Liver Transplantation: An Observational Single-Center Study. J Vasc Interv Radiol. 2018;29:899-904. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 15] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Mauri G, Michelozzi C, Melchiorre F, Poretti D, Tramarin M, Pedicini V, Solbiati L, Cornalba G, Sconfienza LM. Biodegradable biliary stent implantation in the treatment of benign bilioplastic-refractory biliary strictures: preliminary experience. Eur Radiol. 2013;23:3304-3310. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 64] [Cited by in RCA: 57] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 4. | Arabi M, Alrehaili B, Salman R, Qazi S, Bashir O, Abdullah K, Almoaiqel M. Percutaneous Transhepatic Biodegradable Stent Placement for Benign Anastomotic Biliary Strictures: Short-Term Outcomes of a Single-Institution Experience. Arab J Interv Radiol. 2019;3:19-22. [RCA] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Huespe PE, Oggero S, de Santibañes M, Boldrini G, D Agostino D, Pekolj J, de Santibañes E, Ciardullo M, Hyon SH. Percutaneous Patency Recovery and Biodegradable Stent Placement in a Totally Occluded Hepaticojejunostomy After Paediatric Living Donor Liver Transplantation. Cardiovasc Intervent Radiol. 2019;42:466-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 6. | Karanikas M, Bozali F, Vamvakerou V, Markou M, Memet Chasan ZT, Efraimidou E, Papavramidis TS. Biliary tract injuries after lap cholecystectomy-types, surgical intervention and timing. Ann Transl Med. 2016;4:163. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 14] [Cited by in RCA: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 7. | Siiki A, Sand J, Laukkarinen J. A systematic review of biodegradable biliary stents: promising biocompatibility without stent removal. Eur J Gastroenterol Hepatol. 2018;30:813-818. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 40] [Article Influence: 5.7] [Reference Citation Analysis (0)] |
| 8. | Yang S, Hu S, Gu X, Zhang X. Analysis of risk factors for bile duct injury in laparoscopic cholecystectomy in China: A systematic review and meta-analysis. Medicine (Baltimore). 2022;101:e30365. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 15] [Reference Citation Analysis (0)] |
| 9. | Vincenzi P, Mocchegiani F, Nicolini D, Benedetti Cacciaguerra A, Gaudenzi D, Vivarelli M. Bile Duct Injuries after Cholecystectomy: An Individual Patient Data Systematic Review. J Clin Med. 2024;13. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 10. | de'Angelis N, Catena F, Memeo R, Coccolini F, Martínez-Pérez A, Romeo OM, De Simone B, Di Saverio S, Brustia R, Rhaiem R, Piardi T, Conticchio M, Marchegiani F, Beghdadi N, Abu-Zidan FM, Alikhanov R, Allard MA, Allievi N, Amaddeo G, Ansaloni L, Andersson R, Andolfi E, Azfar M, Bala M, Benkabbou A, Ben-Ishay O, Bianchi G, Biffl WL, Brunetti F, Carra MC, Casanova D, Celentano V, Ceresoli M, Chiara O, Cimbanassi S, Bini R, Coimbra R, Luigi de'Angelis G, Decembrino F, De Palma A, de Reuver PR, Domingo C, Cotsoglou C, Ferrero A, Fraga GP, Gaiani F, Gheza F, Gurrado A, Harrison E, Henriquez A, Hofmeyr S, Iadarola R, Kashuk JL, Kianmanesh R, Kirkpatrick AW, Kluger Y, Landi F, Langella S, Lapointe R, Le Roy B, Luciani A, Machado F, Maggi U, Maier RV, Mefire AC, Hiramatsu K, Ordoñez C, Patrizi F, Planells M, Peitzman AB, Pekolj J, Perdigao F, Pereira BM, Pessaux P, Pisano M, Puyana JC, Rizoli S, Portigliotti L, Romito R, Sakakushev B, Sanei B, Scatton O, Serradilla-Martin M, Schneck AS, Sissoko ML, Sobhani I, Ten Broek RP, Testini M, Valinas R, Veloudis G, Vitali GC, Weber D, Zorcolo L, Giuliante F, Gavriilidis P, Fuks D, Sommacale D. 2020 WSES guidelines for the detection and management of bile duct injury during cholecystectomy. World J Emerg Surg. 2021;16:30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 139] [Cited by in RCA: 106] [Article Influence: 26.5] [Reference Citation Analysis (0)] |