Published online Jul 16, 2025. doi: 10.12998/wjcc.v13.i20.103627
Revised: February 23, 2025
Accepted: March 8, 2025
Published online: July 16, 2025
Processing time: 133 Days and 6.1 Hours
Osteoporotic vertebral fracture (OVF) is one of the most common sequelae of osteoporosis. Differential diagnosis between OVF and malignant vertebral fracture (MVF) is a challenge in clinical practice. Findings on computed tomo
To determine whether paravertebral soft tissue swelling is useful for differentiation between OVF and MVF.
We retrospectively reviewed the MRI for 165 patients diagnosed with a vertebral fracture between May 2021 and July 2022. Three radiologists evaluated the vertebral segments and thickness of soft tissue swelling on sagittal MRI by consensus. The morphology of the soft tissue swelling was also evaluated. The statistical analyses were performed using the χ2 test and analysis of variance.
The study included 117 patients (153 vertebrae) with OVF and 48 patients (63 vertebrae) with MVF. Soft tissue swelling was observed beneath the anterior longitudinal ligament on sagittal MRI and rim-shaped in the paravertebral area on axial MRI in all 153 vertebrae with OVF (100%) and in 12 (19%) of the 63 vertebra with MVF; the difference was statistically significant (P < 0.001), 95%CI: 3.156–8.735. Soft tissue swelling beneath the anterior longitudinal ligament spanned significantly more vertebral segments in patients with OVF than in those with MVF (P < 0.001), 95%CI: 0.932-1.546. The mean thickness of the soft tissue swelling was significantly greater for OVF than for MVF (5.62 mm ± 2.50 mm vs 3.88 mm ± 1.73 mm, P < 0.05, 95%CI: 0.681–0.920). Post-contrast examination was performed in 13 patients; T1-weighted images confirmed OVF in 11 cases and MVF in 2 cases. Soft tissue swelling in OVF and MVF had a fusiform appearance or appeared as a thin line on sagittal MRI and was rim-shaped on axial MRI. The length and diameter of the soft tissue swelling in patients with OVF decreased during follow-up.
Paravertebral soft tissue swelling is helpful for differentiating between OVF and MVF.
Core Tip: Paravertebral soft tissue swelling is helpful for differentiating between osteoporotic and malignant vertebral fractures (MVFs). Soft tissue swelling beneath the anterior longitudinal ligament on sagittal magnetic resonance images (MRI) and rim-shaped soft tissue swelling in the paravertebral area on axial MRI are common in osteoporotic vertebral fractures (OVFs) and decrease during follow-up. Soft tissue swelling is seen in a minority of MVFs, with irregular nodules seen in most cases. Furthermore, soft tissue swelling beneath the anterior longitudinal ligament spans more vertebral segments in patients with OVFs than in those with MVFs.
- Citation: Han XL, Shi XL, Li QY, Shao YJ, Gao CP. Paravertebral soft tissue swelling on magnetic resonance images helps in differentiation between osteoporotic and malignant vertebral fractures. World J Clin Cases 2025; 13(20): 103627
- URL: https://www.wjgnet.com/2307-8960/full/v13/i20/103627.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i20.103627
Differentiating between osteoporotic and malignant vertebral compression fractures can present a diagnostic dilemma, particularly in the elderly. The etiology of vertebral compression fractures includes trauma, osteoporosis, and neoplastic infiltration[1]. Osteoporosis is one of the most frequently encountered metabolic bone disorders and is a silent problem until a fracture occurs[2]. Osteoporotic vertebral fracture (OVF) is a benign compression fracture that can result from minor trauma and interpretation of such lesions is complicated. It has been estimated that up to one-third of vertebral compression fractures are benign in the elderly population with no known primary malignancy[1]. However, malignant compression fractures must be excluded in elderly patients because the spine is a common site of metastasis for 10%–15% of cancers[2]. Therefore, differentiation between OVF and malignant vertebral fracture (MVF) is necessary for selection of appropriate treatment.
Magnetic resonance imaging (MRI) has made significant contributions to the detection of abnormalities in the spine and has been reported to be superior to other imaging modalities. A previous study attempted to differentiate between benign and MVFs by analyzing imaging characteristics[3]. The investigators found that a band of low signal intensity on both T1-weighted and T2-weighted images, sparing of normal bone marrow signal intensity in the vertebral body, retropulsion of a posterior bone fragment, and multiple compression fractures were suggestive of acute OVF, whereas a convex posterior border on the vertebral body, abnormal signal intensity in the pedicle or posterior elements, and presence of other spinal lesions were suggestive of MVF.
Soft tissue swelling on MRI is widely accepted as a sign of OVF but also occurs in MVF[1,4]. The purpose of this study was to define and characterize the magnetic resonance (MR) pattern of soft tissue swelling in OVF and MVF in the hope of being able to differentiate between these two types of fracture.
The study was approved by our hospital ethics committee. The need for informed consent was waived in view of the retrospective observational nature of the research.
We retrospectively reviewed patients who underwent radiological examination between May 2021 and July 2022 at our institution and were found to have evidence of spinal compression fracture(s) on MRI. The medical records for these patients, including pathological results, were obtained.
The inclusion criteria for the OVF group were as follows: (1) Osteoporosis confirmed by dual-energy X-ray absorptiometry; (2) At least 6 months of follow-up; and (3) Lesion(s) confirmed on MRI not to have expanded during follow-up. The following inclusion criteria were applied for the MVF group: (1) Patient underwent spinal surgery and intraoperative pathological specimens were obtained; (2) Typical MR findings indicating MVF; and (3) Histological confirmation of malignancy. Patients for whom image quality was poor were excluded regardless of whether they had OVF or MVF.
The final study population included 201 patients, of whom 117 had OVF [153 vertebrae; 92 women, 25 men; mean age 69.5 years (range 55–82 years)] and 48 had MVF [63 vertebrae; 21 women, 27 men; mean age 65 years (range 45–72 years)].
Forty-three of the 48 patients in the MVF group had metastatic carcinoma. The primary neoplasms included lung cancer (n = 13), colorectal cancer (n = 9), stomach cancer (n = 7), hepatocellular carcinoma (n = 6), breast cancer (n = 5), and prostate sarcoma (n = 3). The site of the primary cancer was unknown in 3 patients, and 2 patients had multiple myeloma.
MRI of the thoracolumbar spine was performed using a 1.5-T scanner (Signa Excite, GE Healthcare, Chicago, IL, United States) and phased array coils with the patient in the supine position. The imaging protocol included sagittal spin-echo T1-weighted imaging (repetition time/echo time 460–610 ms/7–19 ms, 4 excitations) and sagittal and transverse T2-weighted imaging (repetition time/echo time 3000–4700 ms/88–128 ms, 4–6 excitations). Sagittal short tau inversion recovery images were also obtained. Contrast-enhanced images were obtained in 13 patients after intravenous administration of gadolinium using a T1-weighted spin-echo sequence with fat suppression.
OVFs and MVFs were categorized based on consensus by two observers after reading all available medical records, MRI, and biopsy data.
Characteristic MRI findings for OVF included retropulsion of the posterior bone fragment and a band of low signal intensity on T1-weighted and T2-weighted images. Additional criteria required for a diagnosis of OVF included no current or past history of malignancy and no malignancy found on clinical examination or imaging during at least 3 months of follow-up.
MVF had the following characteristic MRI findings: (1) Non-homogeneous and diffuse T1-hypointense and T2-hyperintense signal patterns involving the entire vertebra; (2) A convex posterior border of the vertebral body; (3) An epidural or focal paraspinal mass; and (4) Progressive deterioration of a fractured vertebra or other newly developed spinal metastasis detected on follow-up MRI. MVF was confirmed by biopsy in 35 patients.
MRI of the spine were retrospectively reviewed using a double-blind approach by two musculoskeletal radiologists with more than 10 years of experience. The morphological features of the soft tissue swelling were evaluated on sagittal and axial MRI. The maximum thickness of soft tissue swelling was measured in the middle slice on sagittal images and recorded. The number of vertebral segments covered by soft tissue swelling beneath the anterior longitudinal ligament was counted in the craniosacral direction. The signal intensity of the soft tissue swelling and paraspinal mass were evaluated.
The statistical analyses were performed using the χ2 test and analysis of variance. A P value < 0.05 was considered statistically significant.
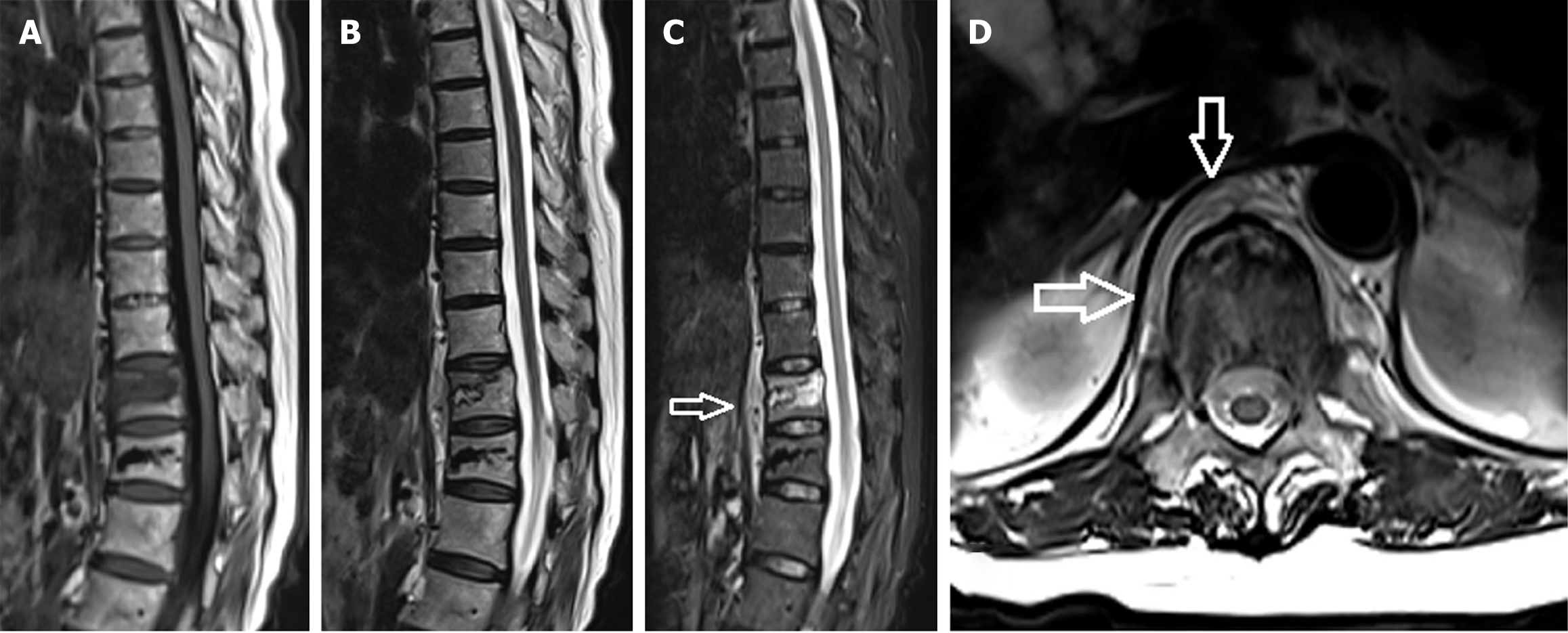
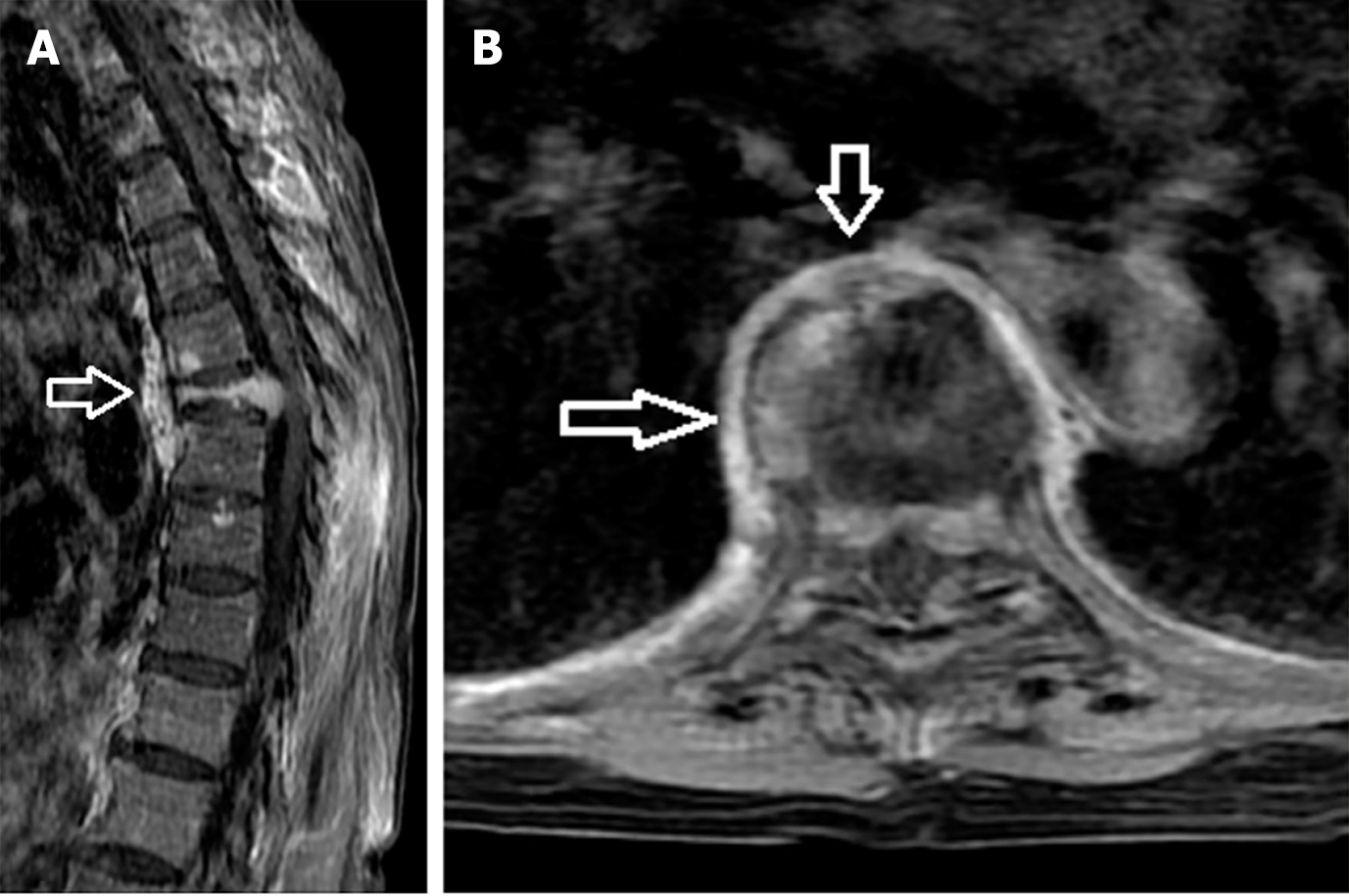
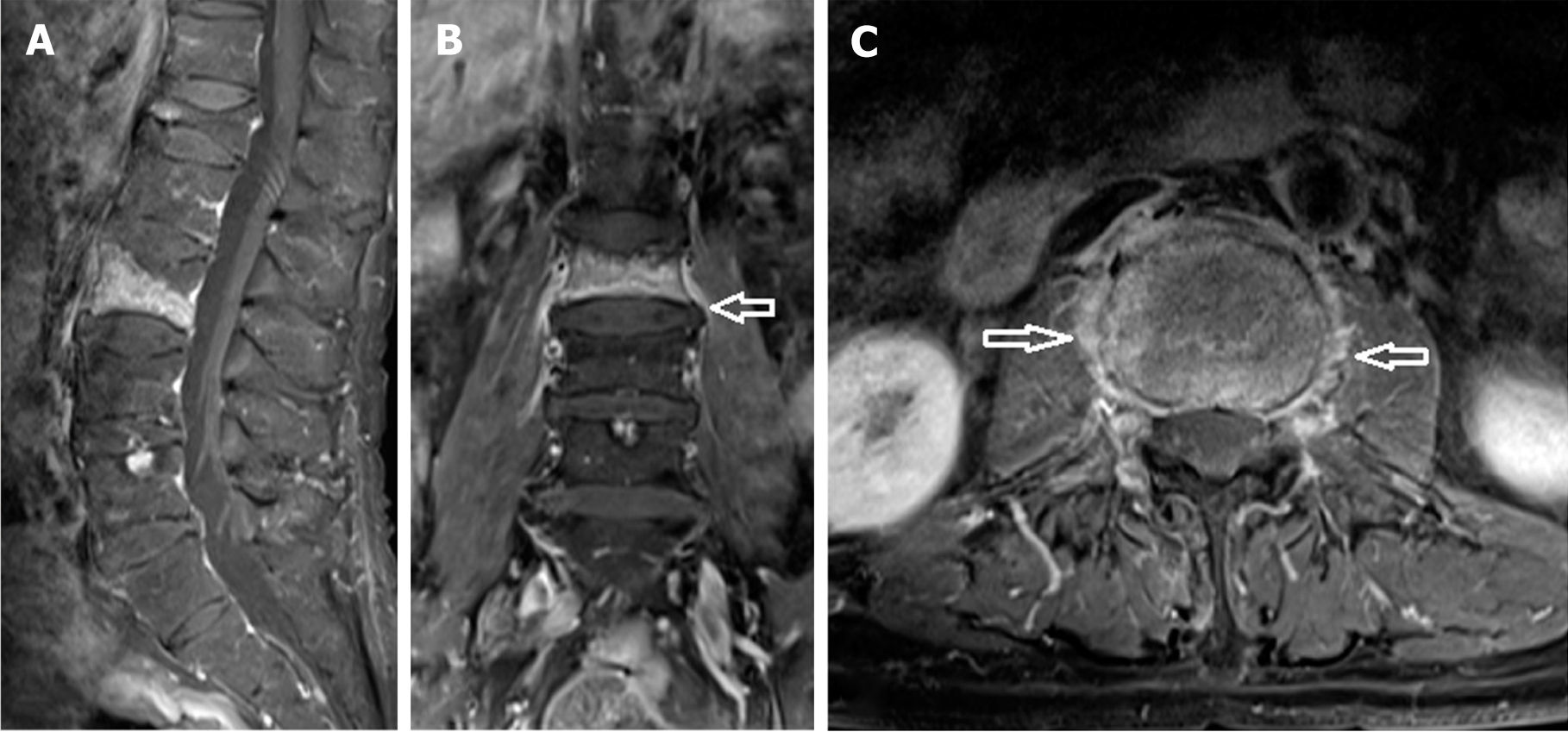
The proportions with soft tissue swelling and soft tissue nodules in the OVF and MVF groups are shown in Table 1. Soft tissue swelling was observed in all 153 vertebrae (100%) with OVF and in 12 (19%) of the 63 vertebra with MVF. The difference was statistically significant (P < 0.001, 95%CI: 3.156–8.735). An irregular soft tissue mass was detected in 51 of the 63 vertebrae with MVF. The soft tissue swelling was consistently rim-shaped on axial MRI whether associated with OVF or MVF (Figures 1, 2 and 3). The soft tissue swelling in OVF and MVF showed homogeneous contrast enhancement on post-enhanced images (Figures 2 and 3).
| Vertebral compression | Soft tissue swelling | Irregular nodule | Total |
| Benign | 153 | 0 | 153 |
| Malignant | 12 | 51 | 63 |
| Total | 165 | 51 | 216 |
The soft tissue swelling beneath the anterior longitudinal ligament in OVF and MVF either extended to multiple vertebral segments or was confined to one vertebral segment (Table 2). Soft tissue swelling extended over multiple segments of the vertebrae in all 153 cases (100%) in the OVF group and in 10 cases (83%) of those in the MVF; the difference was statistically significant (P < 0.05, 95%CI: 0.932-1.546). The longest extension of soft tissue swelling spanned 6 vertebral segments in the OVF group and 5 vertebral segments in the MVF group, and the latter one vertebral body involved. Whether OVF or MVF, soft tissue swelling spanning multiple vertebral segments had a fusiform appearance on sagittal MRI and a regular rim-shaped appearance on axial MRI (Figures 1 and 2).
| Vertebral compression | Multiple vertebral segments | Simple vertebral segment | Total |
| Benign | 153 | 0 | 153 |
| Malignant | 10 | 2 | 12 |
| Total | 163 | 2 | 165 |
The mean thickness of soft tissue swelling was significantly greater in the OVF group than in the MVF group (5.62 mm ± 2.50 mm vs 3.88 mm ± 1.73 mm, P < 0.05) (Table 3).
| Thickness in osteoporotic vertebral fracture (mm) | Thickness in malignant vertebral fracture (mm) | P value | |
| Soft tissue swelling | 5.62 ± 2.50 | 3.88 ± 1.73 | 0.017 |
Osteoporosis is an important clinical and public health problem because of its association with fractures, which are one of the most common causes of disability. Osteoporotic fractures are common in postmenopausal women and in older men[5]. Hip and spine fractures are the most prevalent osteoporotic fractures and have been the most intensively studied. Complications of a vertebral fracture include back pain, decreased mobility, and depression. Furthermore, thoracic fractures cause pulmonary complications and lumbar fractures lead to gastrointestinal symptoms[6].
Osteoporosis is diagnosed based on areal bone mineral density (BMD) as measured by dual-energy X-ray absorptiometry[7], which is widely available for clinical use[8]. BMD is measured to be able to identify patients at high risk of fragility fractures. Other imaging modalities, including computed tomography (CT) and MRI, have been used to improve the assessment of BMD and better understand its relationship with fracture risk[8].
Vertebral compression fractures are common, especially in elderly patients, and may be osteoporotic or malignancy-related. Differentiating between OVF and MVF in the spine is a common problem confronting radiologists and clinicians[9]. Lateral spinal radiographs are conventionally used to assess vertebral fractures based on changes in the shape of the vertebral body. However, this method is usually inadequate for distinguishing between benign and malignant fractures[10]. Signs of OVF include loss of height and evidence of fracture, including lack of endplate parallelism and depression of the endplates on sagittal reconstruction CT images[8]. In contrast, MVF frequently manifests as osteolytic lesions, namely, destruction of cortical and/or cancellous bone[10].
There have been reports suggesting that clinical evaluation and MRI findings, including signal characteristics, cortical disruption, lesion margin, pedicle involvement, enhancement pattern, and paravertebral soft tissue lesions, can distin
The course of OVF is divided into an acute phase (< 2 weeks), a subacute phase (2 weeks to 3 months), and a chronic phase (> 3 months). In OVF, the axial loading force affects not only the vertebral body but also the paravertebral soft tissue[4]. In cases with acute burst fracture of the vertebra, the paravertebral soft tissue not only shows swelling with edematous change but even hemorrhage in some cases[4]. Bousson et al[11] speculated that hemorrhage in OVF was the result of extrusion of a small amount of hematopoietic tissue outside the vertebra rather than true hematoma. Paravertebral soft tissue swelling may show non-homogeneous signal intensity in T1-weighted and T2-weighted images because of hemorrhage or hematopoietic tissue.
Soft tissue swelling beneath the anterior longitudinal ligament spanning multiple vertebral segments is common in OVF, whether solitary or multiple. In our series, soft tissue swelling could extend to over 5 vertebral segments when the OVF was solitary. Soft tissue swelling that extends over multiple vertebral segments typically has a fusiform appearance on sagittal MRI. The maximum diameter measured on sagittal MRI was 1.2 cm in our patients with OVF. In the axial plane, soft tissue swelling has a regular rim-shaped appearance, but may appear as an irregular line in the sagittal plane, especially in the subacute or chronic phase. Our findings are in contrast with those of Bousson et al[11], who found that the thickening was slightly more marked anteriorly. Although there were no nodular or soft tissue masses in any of the patients with OVF in our series, Shih et al[4] described the soft tissue swelling as having an irregular outline. In non-acute vertebral collapse with a benign etiology, edema and extrusion of hemorrhage are absorbed over time, with a decrease in the diameter of the soft tissue swelling and its length in the craniosacral direction. In contrast, MVF tends to deteriorate rapidly to the point where the soft tissue mass can be seen to bulge outward when the tumor fully occupies the vertebral body.
In MVF, the paravertebral soft tissue expands circumferentially[4]. Romeo et al[12] reported that paravertebral or epidural hemorrhage also occurs in MVF. Soft tissue swelling in MVF may have a fusiform appearance on sagittal MRI when it spans multiple vertebral segments. In all our cases of MVF, the soft tissue swelling had a regular rim-shaped appearance on axial MRI. The maximum diameter was 7.2 mm in our series. A malignant fracture is very likely when the circumferential thickening of paraspinal soft tissue is > 1 cm[11,13]. The morphology of a nodular mass in soft tissue is different from that of soft tissue swelling, having a diameter of < 1 cm. The diameter of a soft tissue swelling is signifi
Schwaiger et al[10] reported that the intensity of contrast enhancement in a soft tissue swelling is not a reliable indicator that can be used to differentiate between OVF and MVF, particularly at an early stage. In our series, the area of soft tissue swelling showed significant enhancement on contrast-enhanced T1-weighted images, regardless of whether the fracture was OVF and MVF.
This study has some limitations. First, the study data were collected retrospectively, which means that the possibility of selection bias cannot be excluded. Second, the proportions with soft tissue swelling and irregular nodules were difficult to determine in the MVF group because the swelling occurred only in the early stage of malignancy, whereas all patients with MVF developed nodules in the later stages. Third, the number of segments involved in soft tissue swelling were not accurate in either study group because their length was not matched to an exact number of vertebral bodies in some cases. Further studies in larger sample sizes with longer follow-up periods are needed to validate our findings and explore the potential clinical implications of paravertebral soft tissue swelling in the diagnosis and management of vertebral fractures.
The mechanism of paravertebral soft tissue swelling in OVF is different from that in MVF. Awareness of the differences in imaging manifestations can help to differentiate between these two types of vertebral fracture. Paravertebral soft tissue swelling typically presents with a regular shape on sagittal and axial MRI in OVF but rarely in MVF. Moreover, soft tissue swelling decreases in OVF during follow-up. Irregular soft tissue swelling is a hallmark of MVF and can be used to differentiate MVF from OVF. However, although paravertebral soft tissue swelling is useful for differentiation between these two types of fracture, other MRI characteristics should also be included to ensure a correct diagnosis.
| 1. | Fornasier VL, Czitrom AA. Collapsed vertebrae: a review of 659 autopsies. Clin Orthop Relat Res. 1978;261-265. [PubMed] |
| 2. | Kutsal FY, Ergin Ergani GO. Vertebral compression fractures: Still an unpredictable aspect of osteoporosis. Turk J Med Sci. 2021;51:393-399. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 25] [Cited by in RCA: 53] [Article Influence: 13.3] [Reference Citation Analysis (1)] |
| 3. | Jung HS, Jee WH, McCauley TR, Ha KY, Choi KH. Discrimination of metastatic from acute osteoporotic compression spinal fractures with MR imaging. Radiographics. 2003;23:179-187. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 209] [Cited by in RCA: 147] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 4. | Shih TT, Huang KM, Li YW. Solitary vertebral collapse: distinction between benign and malignant causes using MR patterns. J Magn Reson Imaging. 1999;9:635-642. [PubMed] [DOI] [Full Text] |
| 5. | Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359:1761-1767. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2507] [Cited by in RCA: 2583] [Article Influence: 112.3] [Reference Citation Analysis (0)] |
| 6. | Bliuc D, Nguyen ND, Milch VE, Nguyen TV, Eisman JA, Center JR. Mortality risk associated with low-trauma osteoporotic fracture and subsequent fracture in men and women. JAMA. 2009;301:513-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1130] [Cited by in RCA: 1211] [Article Influence: 75.7] [Reference Citation Analysis (0)] |
| 7. | Wesarg S, Kirschner M, Becker M, Erdt M, Kafchitsas K, Khan MF. Dual-energy CT-based assessment of the trabecular bone in vertebrae. Methods Inf Med. 2012;51:398-405. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Chou SH, LeBoff MS. Vertebral Imaging in the Diagnosis of Osteoporosis: a Clinician's Perspective. Curr Osteoporos Rep. 2017;15:509-520. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 22] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 9. | Karchevsky M, Babb JS, Schweitzer ME. Can diffusion-weighted imaging be used to differentiate benign from pathologic fractures? A meta-analysis. Skeletal Radiol. 2008;37:791-795. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 59] [Cited by in RCA: 55] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 10. | Schwaiger BJ, Gersing AS, Baum T, Krestan CR, Kirschke JS. Distinguishing Benign and Malignant Vertebral Fractures Using CT and MRI. Semin Musculoskelet Radiol. 2016;20:345-352. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 21] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 11. | Bousson V, Royer M, Cortet B. Osteoporotic fractures: challenging cases and diagnostic pitfalls. Joint Bone Spine. 2012;79 Suppl 2:S91-S95. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 12. | Romeo V, Ugga L, Stanzione A, Cocozza S, Cuocolo R, Brunetti A. Differential diagnosis of benign and malignant vertebral compression fractures using conventional and advanced MRI techniques. BJR Open. 2019;1:20180033. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 13. | Tan SB, Kozak JA, Mawad ME. The limitations of magnetic resonance imaging in the diagnosis of pathologic vertebral fractures. Spine (Phila Pa 1976). 1991;16:919-923. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 32] [Article Influence: 0.9] [Reference Citation Analysis (0)] |