Published online Jul 6, 2025. doi: 10.12998/wjcc.v13.i19.104083
Revised: February 6, 2025
Accepted: February 24, 2025
Published online: July 6, 2025
Processing time: 100 Days and 0.4 Hours
Tuberculosis (TB) remains a global health concern despite decreasing incidence. Delayed TB diagnosis can exacerbate patient outcomes and lead to broader public health issues such as mass infections. Differentiation between TB and bacterial pneumonia is often complicated by variable clinical and radiological manifestations of TB, leading to diagnostic delays.
An 89-year-old, Japanese male patient with a history of diabetes mellitus, hypertension, and hypothyroidism presented with right-sided chest pain. Based on the elevated inflammatory response, right pleural effusion, and infiltrating shadow in the lung field, the diagnosis of right pleurisy was made and the anti
There are cases of TB wherein temporary improvement apparently could be shown through treatment with antimicrobial agents other than anti-TB drugs, necessitating careful evaluation in atypical cases of bacterial pneumonia.
Core Tip: There are cases of tuberculosis (TB) wherein diagnosis is delayed because they appear to improve temporarily after using an antimicrobial other than fluoroquinolone. In cases of pneumonia that follow an atypical course, such as one that improves after treatment with antibacterial drugs but then worsens again, reevaluating the possibility of TB is extremely important.
- Citation: Hara M, Yashiro T, Yashiro Y. Delayed diagnosis of pulmonary tuberculosis with pleuritis due to ampicillin/sulbactam: A case report. World J Clin Cases 2025; 13(19): 104083
- URL: https://www.wjgnet.com/2307-8960/full/v13/i19/104083.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i19.104083
Although the global incidence of tuberculosis (TB) is decreasing, it remains an important cause of death among infectious diseases[1]. Delayed TB diagnosis not only worsens prognosis but also causes social problems such as infection to surroundings. Symptoms of TB are often characterized by prolonged cough, chest pain, fatigue, weight loss, fever, and night sweats[2]. Radiographic findings are commonly associated with pulmonary TB, such as upper lobe cavitary lesions and centrilobular nodules[3]. However, these clinical and radiological findings are not specific for TB; we often detect TB without these findings[2,3]. Therefore, distinguishing TB from bacterial pneumonia is sometimes challenging in the clinical practice[4]. Fluoroquinolones are commonly used for community-acquired pneumonia; it is well known that their partial effectiveness against TB can delay diagnosis and affect prognosis[5,6]. In contrast, the impact of antimicrobials other than fluoroquinolones on the course of TB is not well known. Herein, we report a case of pulmonary TB with pleuritis wherein the diagnosis was delayed due to administration of sulbactam/ampicillin.
An 89-year-old Japanese man was referred to our hospital due to intermittent right chest pain, low grade fever, and fatigue since discharge from hospitalization for pneumonia 2 months ago.
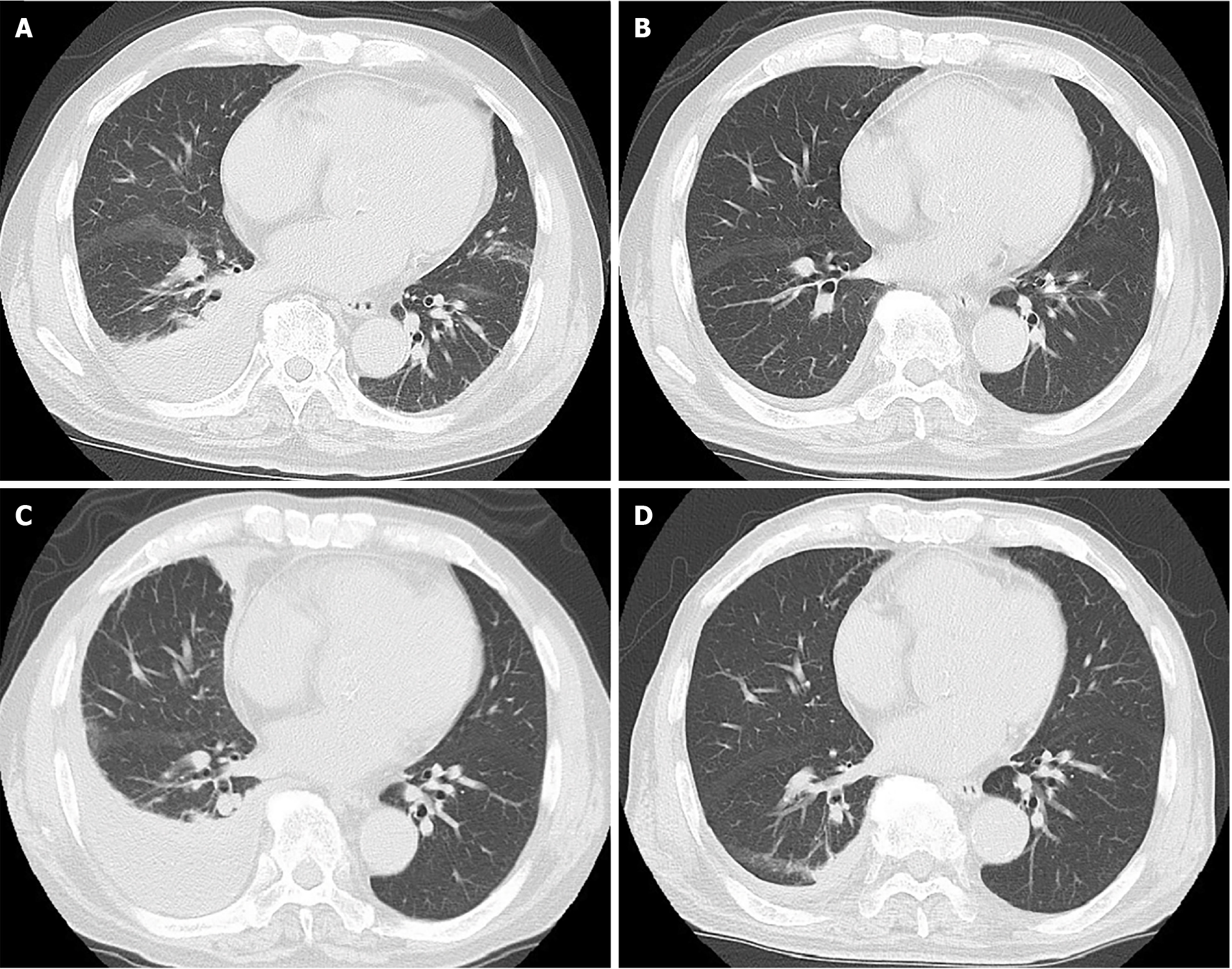
The patient was referred to our hospital three months before this admission for right chest pain that lasted for five days. This was based on the right chest pain, elevated inflammatory response, infiltrative shadows in the lower lobes of the right lung, and right pleural effusion on a chest computed tomography (Figure 1A). A sputum culture could not be submitted due to poor sputum expectoration. Thoracentesis was not performed because the pleural effusion was small, as observed on chest ultrasonography, and a risk of lung penetration existed. Diagnosis of bacterial pneumonia and pleurisy was made; the administration of the antibiotic sulbactam/ampicillin 9 g/day was started. Eight days after administration of sulbactam/ampicillin, his symptoms and radiological findings improved (Figure 1B). Therefore, the patient was discharged and followed up by his family doctor. However, during follow-up, his symptoms, including right chest pain, low grade fever, and fatigue, recurred. He was diagnosed with a relapse of pleurisy, and antibiotics, including fluo
The patient had a history of hypertension, hypothyroidism, and diabetes mellitus. Hypertension was well controlled with cilnidipine (20 mg, qd), and levothyroxine sodium hydrate (25 μg, qd) had been administered for hypothyroidism. His diabetes was controlled with linagliptin (5 mg, qd). He had surgery for colon cancer seven years ago.
He had no history of smoking, allergies, or notable family history of respiratory or malignant diseases.
Physical examination revealed a body temperature of 36.1 °C, pulse rate of 67/min, blood pressure of 113/48 mmHg, respiratory rate of 22/min (mildly labored), and O2 saturation of 92% on ambient air. No murmurs were heard; the lungs were clear on auscultation. There were no rashes, joint swelling, or limb deformities suggestive of autoimmune diseases.
Laboratory tests showed a re-elevated inflammatory response, a white blood cell count of 9400/μL, with 77.6% segmented neutrophils, a C-reactive protein level of 13.6 mg/dL, a high hemoglobin A1c level of 7.6%, and renal dysfunction, with blood urea nitrogen levels of 22 mg/dL and creatinine levels of 1.18 mg/dL. Interferon-gamma release assays (IGRA) were withholding judgment. The right pleural effusion had reaccumulated and had increased further compared with his previous hospitalization; right thoracentesis was performed to collect a pleural fluid sample. The pleural fluid examination revealed an elevated lymphocyte ratio of 91%, a serum protein level of 7.9 g/dL, and a lactate dehydrogenase (LDH) level of 200 U/L, as well as a pleural fluid protein level of 5.3 g/dL, an LDH level of 818 IU/L, and exudative effusion. Pleural fluid cytology did not reveal any malignant findings. The pleural fluid adenosine deaminase level was high at 107.6 U/L. Although Ziehl–Neelsen staining of the pleural fluid yielded negative results, a polymerase chain reaction test of Mycobacterium TB (Mtb) was positive.
Chest CT scan showed an infiltrative shadow in the lower right lobe and increased right pleural effusion (Figure 1C).
Pulmonary TB with pleuritis.
Isoniazid (0.3 g, qd), rifampicin (0.6 g, qd), and ethambutol (0.75 g, qd) were administered. Pyrazinamide was not administered because of the patient’s age and poor vitality at treatment initiation.
The patient’s general condition gradually improved and the right pleural effusion decreased due to anti-TB drugs, (Figure 1D). Acid-fast bacterium culture was positive in sputum and pleural fluid and was isoniazid- and rifampicin-susceptible. Two months after the initiation of three-drug therapy, the treatment was switched to two-drug therapy comprising isoniazid and rifampicin for 10 months. After completion of 12 months of TB treatment, careful follow-up has been performed every six months; no flare-ups of chest pain or other symptoms or re-accumulation of pleural effusions have been observed. Careful follow-up was scheduled to be continuously performed for 2 years after completing treatment.
An estimated 10.6 million people were ill with TB worldwide in 2022, increasing to 10.3 million in 2021 from 10.0 million in 2020, following a decline between 2010 and 2020[7]. This reversal of progress up to 2020 is thought to reflect the impact of disruption in essential TB services during the coronavirus disease 2019 pandemic worldwide. Whereas some countries have reduced the burden of TB disease to fewer than 10 cases per 100000 people per year, the incidence of TB remains high in low-income countries[7]. Furthermore, in 2022, the total number of deaths caused by TB was 1.30 million globally, and TB remains the second leading cause of death worldwide from a single infectious agent[7].
The characteristics of TB symptoms include prolonged cough, chest pain, weakness or fatigue, weight loss, fever, and night sweats[8]. However, these symptoms are not specific to TB; in many cases, these symptoms do not occur[2], particularly in older individuals, who are less likely to present with classic symptoms of cough, hemoptysis, fever, and night sweats than are younger adults[9]. Although imaging findings of pulmonary TB are characterized by a predominance of upper lobe cavitary and centrilobular nodules, these characteristics are not present in some cases. Furthermore, cases of TB without these radiological findings are also reported[3]. Therefore, TB diagnosis is often delayed because TB can be misdiagnosed as common community-acquired pneumonia. A delayed TB diagnosis leads to delayed initiation of appropriate treatment, resulting in a worsened prognosis and resistance to anti-TB drugs. Furthermore, social problems such as nosocomial and mass infections can occur because of delayed diagnosis. Early diagnosis and prevention of TB spread are critical components of public health strategies. Community-level interventions, such as health promotion activities and educational sessions, can encourage individuals to seek screening and treatment. These activities and sessions have shown some success in increasing detection of TB cases[10].
In the present case, no significant symptoms other than right-sided chest pain were observed at the time of initial examination, and no cavity shadows or centrilobular nodules characteristic of TB were observed on imaging. Furthermore, a sputum test for acid-fast bacilli could not be performed because of poor sputum production and a pleural fluid test was not performed because of the small amount of pleural effusion at the time of initial examination. Bacterial pleurisy was initially diagnosed based on physical and radiological findings, followed by the administration of ampicillin/sulbactam, which resulted in an approximately 3-month delay in establishing a definitive TB diagnosis. In the present case, the submission of sputum smear and culture tests by attempting to induce sputum at the time of initial hospitalization, as well as analysis of gastric fluid specimens and IGRA, could have led to TB diagnosis and avoided the delay in diagnosis caused by the use of ampicillin/sulbactam.
Fluoroquinolones are used to treat community-acquired pneumonia and achieve temporary improvement in TB symptoms, resulting in a delay in the correct diagnosis of TB, further affecting prognosis[5,6]. Additionally, the use of antimicrobial agents other than fluoroquinolones, such as penicillin with beta-lactamase inhibitors and carbapenems, can lead to delayed TB diagnosis due to temporary improvements in symptoms and radiological findings of TB[11,12]. Previous studies have discussed the delayed diagnosis of TB caused using these antimicrobial agents, their direct and partial effects on TB, the possibility that these agents can effectively treat co-infections caused by other bacteria, and the time-consuming process of determining the effectiveness of the prescribed antimicrobials[5]. In the present case, a bacteriological examination could not be submitted at the time of admission 2 months ago, and the possibility that there was co-infection with bacteria other than TB and that ampicillin/sulbactam had an effect on those bacteria cannot be ruled out. Furthermore, clinical findings of TB can improve temporarily depending on various factors such as the patient's immune status, underlying disease, and natural course of TB[13,14]. TB manifests with various clinical conditions in its natural history; approximately 5%–10% of infected people develop active TB[15]. Symptoms and radiological findings of TB are non-specific particularly in older adults, wherein TB diagnosis is more often delayed and mortality is higher[16]. The present case was also an older adult (89-year-old) and was on treatment for diabetes. Factors such as age, immune status, and background disease might have influenced the course of this temporary improvement in TB.
On the other hand, one of the mechanisms by which TB is resistant to beta-lactams is that TB produces beta-lactamases[17,18]. With these researches as a background, the in vitro activity of beta-lactam and beta-lactamase inhibitors against TB and their clinical efficacy against multidrug-resistant TB have been reported[19-23]. Even in the present case, the clinical course of the right pleural effusion, in which Mtb was subsequently detected, temporally decreased after ampicillin/sulbactam administration, suggesting the possibility that ampicillin/sulbactam was temporarily effective against Mtb.
In this case, IGRA at the time of pleurisy relapse showed borderline levels. IGRA is in vitro blood test that measures T cell release of interferon-gamma following stimulation by antigens unique to Mtb and a few other mycobacteria[24]. IGRA has specificity > 95% for diagnosis of TB infection, since it is not affected by Bacillus Calmette–Guérin vaccination or most nontuberculous mycobacteria[25]. However, human immunodeficiency virus infection, aging, low lymphocyte counts, and the use of immunosuppressive drugs can cause false negatives[26-28]. In this case, the patient was 89-year-old man. This may have been one of the reasons why the IGRA result was inconclusive. If IGRA had been performed at the time of the initial hospitalization, the possibility of TB would have been considered based on the results of the judgment pending; a TB diagnosis could have been made with additional tests such as thoracentesis. In terms of treatment, in this case, given the patient's age of 89, we chose to treat him with isoniazid, rifampicin, and ethambutol rather than pyrazinamide. However, in recent years there have been reports that pyrazinamide regimens can be safely used in older adults, and the use of pyrazinamide was considered an important option[29]. In addition, a 4-month regimen of rifapentine and moxifloxacin has been non-inferior to standard therapy and is expected to become a treatment option in the future[30].
A clinical course that appears to have temporarily improved with treatment other than anti-TB drugs can lead to the assumption that the patient does not have TB, which is disadvantageous. To prevent delayed TB diagnosis, appropriate bacteriological tests should be performed at the initiation of pneumonia treatment. However, difficulty in obtaining samples can occur, as in this case. Therefore, when the condition of patients is improved with antibiotics other than anti-TB drugs while the clinical findings repeatedly worsen or an atypical course of bacterial infection occurs, a reassessment should be performed to determine whether the patients could have TB.
TB remains an important differential disease for respiratory tract infections; sometimes it is very difficult to distinguishing it from bacterial pneumonia is sometimes very difficult. As in this case, there are cases of TB wherein it appears that a temporary improvement has been achieved through treatment with antimicrobial agents other than anti-TB drugs due to various factors, such as the patient's immune status and natural course of TB. To prevent delays in TB diagnosis, appropriate sample submissions for bacteriological examination, including testing for acid-fast bacilli, are required before initiating antibiotics in cases of pneumonia. When it is difficult to submit samples at the start of pneumonia treatment, re-evaluation for TB infection is necessary in cases of an atypical course, such as relapse after temporary improvement in pneumonia with antimicrobial agents against common bacteria.
| 1. | Furin J, Cox H, Pai M. Tuberculosis. Lancet. 2019;393:1642-1656. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 371] [Cited by in RCA: 552] [Article Influence: 92.0] [Reference Citation Analysis (0)] |
| 2. | Miller LG, Asch SM, Yu EI, Knowles L, Gelberg L, Davidson P. A population-based survey of tuberculosis symptoms: how atypical are atypical presentations? Clin Infect Dis. 2000;30:293-299. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 52] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 3. | Komiya K, Yamasue M, Goto A, Nakamura Y, Hiramatsu K, Kadota JI, Kato S. High-resolution computed tomography features associated with differentiation of tuberculosis among elderly patients with community-acquired pneumonia: a multi-institutional propensity-score matched study. Sci Rep. 2022;12:7466. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 4. | Cavallazzi R, Wiemken T, Christensen D, Peyrani P, Blasi F, Levy G, Aliberti S, Kelley R, Ramirez J; Community-Acquired Pneumonia Organization (CAPO) Investigators. Predicting Mycobacterium tuberculosis in patients with community-acquired pneumonia. Eur Respir J. 2014;43:178-184. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 14] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 5. | Wang JY, Hsueh PR, Jan IS, Lee LN, Liaw YS, Yang PC, Luh KT. Empirical treatment with a fluoroquinolone delays the treatment for tuberculosis and is associated with a poor prognosis in endemic areas. Thorax. 2006;61:903-908. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 95] [Cited by in RCA: 96] [Article Influence: 5.1] [Reference Citation Analysis (0)] |
| 6. | Dooley KE, Golub J, Goes FS, Merz WG, Sterling TR. Empiric treatment of community-acquired pneumonia with fluoroquinolones, and delays in the treatment of tuberculosis. Clin Infect Dis. 2002;34:1607-1612. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 76] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 7. | World Health Organization. Global tuberculosis report ‘2023’. Available from: https://iris.who.int/bitstream/handle/10665/373828/9789240083851-eng.pdf?sequence=1. |
| 8. | World Health Organization. Tuberculosis. Available from: https://www.who.int/health-topics/tuberculosis#tab=tab_2. |
| 9. | Korzeniewska-Kosela M, Krysl J, Müller N, Black W, Allen E, FitzGerald JM. Tuberculosis in young adults and the elderly. A prospective comparison study. Chest. 1994;106:28-32. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 99] [Cited by in RCA: 96] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 10. | Mhimbira FA, Cuevas LE, Dacombe R, Mkopi A, Sinclair D. Interventions to increase tuberculosis case detection at primary healthcare or community-level services. Cochrane Database Syst Rev. 2017;11:CD011432. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 47] [Article Influence: 5.9] [Reference Citation Analysis (0)] |
| 11. | Craig SE, Bettinson H, Sabin CA, Gillespie SH, Lipman MC. Think TB! Is the diagnosis of pulmonary tuberculosis delayed by the use of antibiotics? Int J Tuberc Lung Dis. 2009;13:208-213. [PubMed] |
| 12. | Wang M, Fitzgerald JM, Richardson K, Marra CA, Cook VJ, Hajek J, Elwood RK, Bowie WR, Marra F. Is the delay in diagnosis of pulmonary tuberculosis related to exposure to fluoroquinolones or any antibiotic? Int J Tuberc Lung Dis. 2011;15:1062-1068. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 23] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 13. | Walter C, Acuña-Villaorduna C, Hochberg NS, Sinha P. Case Report: Tuberculosis Autoregression after Minimal Treatment and Review of the Literature. Am J Trop Med Hyg. 2022;107:595-599. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 14. | Millington KA, Gooding S, Hinks TS, Reynolds DJ, Lalvani A. Mycobacterium tuberculosis-specific cellular immune profiles suggest bacillary persistence decades after spontaneous cure in untreated tuberculosis. J Infect Dis. 2010;202:1685-1689. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 42] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 15. | Behr MA, Edelstein PH, Ramakrishnan L. Revisiting the timetable of tuberculosis. BMJ. 2018;362:k2738. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 192] [Cited by in RCA: 261] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 16. | Packham S. Tuberculosis in the elderly. Gerontology. 2001;47:175-179. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 12] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 17. | Kasik JE, Monick M, Schwarz B. beta-Lactamase activity in slow-growing nonpigmented mycobacteria and their sensitivity to certain beta-lactam antibiotics. Tubercle. 1980;61:213-219. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 18. | Segura C, Salvadó M. Beta-lactamases of Mycobacterium tuberculosis and Mycobacterium kansasii. Microbiologia. 1997;13:331-336. [PubMed] |
| 19. | Cynamon MH, Palmer GS. In vitro activity of amoxicillin in combination with clavulanic acid against Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1983;24:429-431. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 79] [Cited by in RCA: 72] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 20. | Chambers HF, Kocagöz T, Sipit T, Turner J, Hopewell PC. Activity of amoxicillin/clavulanate in patients with tuberculosis. Clin Infect Dis. 1998;26:874-877. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 103] [Cited by in RCA: 105] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 21. | Nadler JP, Berger J, Nord JA, Cofsky R, Saxena M. Amoxicillin-clavulanic acid for treating drug-resistant Mycobacterium tuberculosis. Chest. 1991;99:1025-1026. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 82] [Cited by in RCA: 77] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 22. | Prabhakaran K, Harris EB, Randhawa B. Bactericidal action of ampicillin/sulbactam against intracellular mycobacteria. Int J Antimicrob Agents. 1999;13:133-135. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 23. | Pagliotto AD, Caleffi-Ferracioli KR, Lopes MA, Baldin VP, Leite CQ, Pavan FR, Scodro RB, Siqueira VL, Cardoso RF. Anti-Mycobacterium tuberculosis activity of antituberculosis drugs and amoxicillin/clavulanate combination. J Microbiol Immunol Infect. 2016;49:980-983. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 24. | Lewinsohn DM, Leonard MK, LoBue PA, Cohn DL, Daley CL, Desmond E, Keane J, Lewinsohn DA, Loeffler AM, Mazurek GH, O'Brien RJ, Pai M, Richeldi L, Salfinger M, Shinnick TM, Sterling TR, Warshauer DM, Woods GL. Official American Thoracic Society/Infectious Diseases Society of America/Centers for Disease Control and Prevention Clinical Practice Guidelines: Diagnosis of Tuberculosis in Adults and Children. Clin Infect Dis. 2017;64:111-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 348] [Cited by in RCA: 486] [Article Influence: 60.8] [Reference Citation Analysis (0)] |
| 25. | Pai M, Zwerling A, Menzies D. Systematic review: T-cell-based assays for the diagnosis of latent tuberculosis infection: an update. Ann Intern Med. 2008;149:177-184. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1001] [Cited by in RCA: 939] [Article Influence: 55.2] [Reference Citation Analysis (0)] |
| 26. | Yamasue M, Komiya K, Usagawa Y, Umeki K, Nureki SI, Ando M, Hiramatsu K, Nagai H, Kadota JI. Factors associated with false negative interferon-γ release assay results in patients with tuberculosis: A systematic review with meta-analysis. Sci Rep. 2020;10:1607. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 27. | Nguyen DT, Teeter LD, Graves J, Graviss EA. Characteristics Associated with Negative Interferon-γ Release Assay Results in Culture-Confirmed Tuberculosis Patients, Texas, USA, 2013-2015. Emerg Infect Dis. 2018;24:534-540. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 33] [Cited by in RCA: 52] [Article Influence: 8.7] [Reference Citation Analysis (0)] |
| 28. | Wong SH, Gao Q, Tsoi KK, Wu WK, Tam LS, Lee N, Chan FK, Wu JC, Sung JJ, Ng SC. Effect of immunosuppressive therapy on interferon γ release assay for latent tuberculosis screening in patients with autoimmune diseases: a systematic review and meta-analysis. Thorax. 2016;71:64-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 85] [Cited by in RCA: 82] [Article Influence: 9.1] [Reference Citation Analysis (0)] |
| 29. | Taniguchi J, Jo T, Aso S, Matsui H, Fushimi K, Yasunaga H. Safety of pyrazinamide in elderly patients with tuberculosis in Japan: A nationwide cohort study. Respirology. 2024;29:905-913. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Reference Citation Analysis (0)] |
| 30. | Dorman SE, Nahid P, Kurbatova EV, Phillips PPJ, Bryant K, Dooley KE, Engle M, Goldberg SV, Phan HTT, Hakim J, Johnson JL, Lourens M, Martinson NA, Muzanyi G, Narunsky K, Nerette S, Nguyen NV, Pham TH, Pierre S, Purfield AE, Samaneka W, Savic RM, Sanne I, Scott NA, Shenje J, Sizemore E, Vernon A, Waja Z, Weiner M, Swindells S, Chaisson RE; AIDS Clinical Trials Group; Tuberculosis Trials Consortium. Four-Month Rifapentine Regimens with or without Moxifloxacin for Tuberculosis. N Engl J Med. 2021;384:1705-1718. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 156] [Cited by in RCA: 312] [Article Influence: 78.0] [Reference Citation Analysis (0)] |