Published online Jun 26, 2025. doi: 10.12998/wjcc.v13.i18.103426
Revised: January 18, 2025
Accepted: February 6, 2025
Published online: June 26, 2025
Processing time: 93 Days and 16.2 Hours
Gastric bezoars are masses of indigestible material that accumulate in the stomach, causing nausea, abdominal pain, and vomiting. Persimmon bezoars (diospyrobezoars), which comprise tannins and fibers from persimmons, are relatively rare but may cause significant gastric complications, including gastric outlet obstruction or ileus. Although computed tomography (CT) is a useful ima
Here, we report the case of a 72-year-old woman with a persimmon bezoar that was diagnosed using serial CT imaging and confirmed by endoscopy. CT perfor
Gastric bezoars, particularly persimmon bezoars, present diagnostic challenges because of their variable imaging characteristics. Serial CT can document tem
Core Tip: Gastric bezoars, particularly persimmon bezoars, are rare but significant clinical entities that can lead to complications such as gastric outlet obstruction and ileus. Diagnosis can be challenging because they often appear similar to food debris on imaging. Serial computed tomography can be used to document temporal changes in the internal structure and density of bezoars, reflecting their progressive hardening over time. Early recognition and endoscopic fragmentation remain the most effective management strategies, particularly in patients with predisposing factors such as prior gastric surgery or excessive persimmon consumption.
- Citation: Iwamuro M, Yoshikawa T, Kamio T, Hirata S, Matsueda K, Kametaka D, Otsuka M. Temporal changes in computed tomography findings of a persimmon bezoar: A case report. World J Clin Cases 2025; 13(18): 103426
- URL: https://www.wjgnet.com/2307-8960/full/v13/i18/103426.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i18.103426
Gastric bezoars are conglomerates of indigestible materials that accumulate in the stomach, leading to abdominal pain, bloating, nausea, and vomiting. Among the various types of bezoars, persimmon bezoars, or diospyrobezoars, are relatively rare and primarily comprise tannins and fibers found in persimmons. These substances can polymerize into a solid mass in the acidic gastric environment, particularly in individuals with predisposing factors, such as prior gastric surgery, delayed gastric emptying, and excessive persimmon consumption[1-5]. Diospyrobezoars are more prevalent in regions where persimmons are widely consumed, and pose a unique diagnostic challenge because of their nonspecific presentation[5].
Computed tomography (CT) plays a significant role in identifying gastric bezoars; however, the density of bezoars often resembles that of food debris or gastric contents, making them difficult to detect[6-10]. Misinterpretation of CT findings can delay the diagnosis and treatment of gastric bezoars, leading to complications, such as obstruction of the gastric outlet or migration to the small intestine, thereby causing ileus[11-13]. Serial imaging studies are rarely performed in the case of bezoars; as such, there is a limited understanding of the temporal changes in their physical properties over time, such as density and internal structure.
This report presents a unique case of a persimmon bezoar, focusing on serial CT findings that documented changes in the internal structure and density of the bezoar over time. These findings provide insights into the natural history of bezoars and suggest potential correlations between their imaging characteristics and physical properties. Additionally, this report emphasizes the importance of clinical context and dietary history in diagnosing and managing bezoars effectively.
A 72-year-old Japanese woman presenting with intermittent abdominal bloating and vomiting was referred to our hospital.
The patient had undergone a pylorus-preserving gastrectomy for gastric cancer and right oophorectomy at 43 years of age. At the age of 66 years, the patient was diagnosed with advanced colon cancer. Chemotherapy was initiated but discontinued after four courses because of adverse effects, and the patient subsequently declined further chemotherapy. As tumor shrinkage was achieved with treatment, the patient underwent right hemicolectomy for the ascending colon cancer, which included resection of the small intestine, ovary, and peritoneum, owing to tumor invasion. Due to intolerance to preoperative chemotherapy, the patient refused postoperative chemotherapy. The patient requested CT scans every three months, and no recurrence was noted after surgery.
The patient experienced abdominal fullness after meals and occasional vomiting from ingested food. However, because the symptoms were intermittent, the patient refused to take any medication. Seven months after symptom onset, she developed gastric obstruction, which made eating difficult, and she passed black stools for approximately 10 days. Following the onset of abdominal symptoms, the patient continued to undergo CT scans every three months to monitor for colorectal cancer recurrence, and the radiologist reported no notable abnormalities or signs of recurrence at the time of imaging. She visited her primary care physician, who prescribed mosapride, famotidine, and Clostridium butyricum tablets, which partially relieved the symptoms. Nine months after the onset of the abdominal symptoms, the patient visited our hospital upon request. No endoscopic examinations were performed between abdominal symptom onset and her visit to our hospital.
At the time of her visit to our hospital, she was taking mosapride, famotidine, and Clostridium butyricum tablets. The patient was 150 cm tall and weighed 41 kg, resulting in a body mass index of approximately 18.2.
As previously described, the patient underwent a pylorus-preserving gastrectomy for gastric cancer and right oophorectomy at the age of 43 years. At 66 years of age, the patient underwent right hemicolectomy, including resection of the small intestine, ovary, and peritoneum, for advanced ascending colon cancer.
The patient had no history of alcohol consumption or smoking, and no family history of malignancies or gastrointestinal diseases.
Physical examination revealed multiple scars on her abdomen from previous surgeries for gastric and colon cancers. Her abdomen was soft and flat without palpable masses or signs of peripheral lymphadenopathy.
Laboratory tests at her initial visit showed anemia, with a red blood cell count of 3.3 × 106/μL, hemoglobin concentration of 10.7 g/dL, and hematocrit of 34.8%. Decreased levels of total protein (6.2 g/dL) and albumin (3.9 g/dL) were observed, along with increased levels of aspartate aminotransferase (45 U/L), alanine aminotransferase (43 U/L), gamma-glutamyl transpeptidase (66 U/L), lactate dehydrogenase [267 U/L (normal range: 124-222 U/L)], blood urea nitrogen (22.6 mg/dL), and creatinine (1.24 mg/dL). We considered her anemia, hypoalbuminemia, mild elevation of liver enzyme levels, and impaired renal function to be primarily attributable to malnutrition and dehydration resulting from insufficient oral intake. The carcinoembryonic antigen level was elevated to 9.76 ng/mL (normal range: 0-5 ng/mL), although it had fluctuated within this range over the past year. Cancer antigen 19-9 and other biochemical parameters were within normal limits.
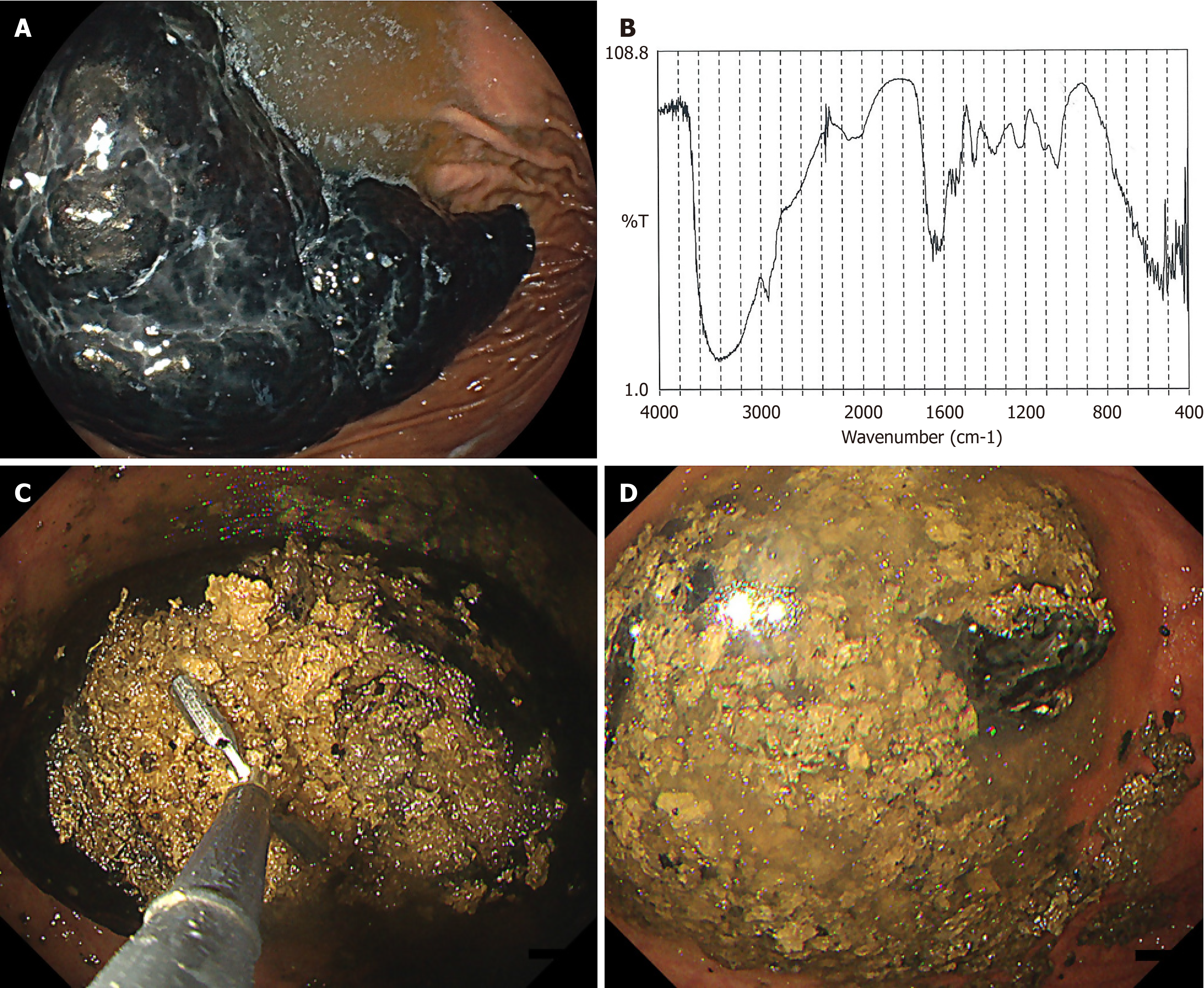
Although medication from the patient’s primary care physician partially relieved her symptoms, we performed esophagogastroduodenoscopy to further evaluate gastric obstruction and the passage of black stools. Esophagogastroduodenoscopy revealed an elongated black gastric bezoar, approximately 10 cm in length, within the stomach (Figure 1A). A review of the patient’s dietary history revealed that she had consumed 4-5 persimmons daily for two weeks, approximately 10 months before presentation. Infrared spectrometry of the bezoar fragments showed a > 98% similarity to the spectra of the persimmon extracts (Figure 1B). Therefore, a definitive diagnosis of persimmon bezoar was established.
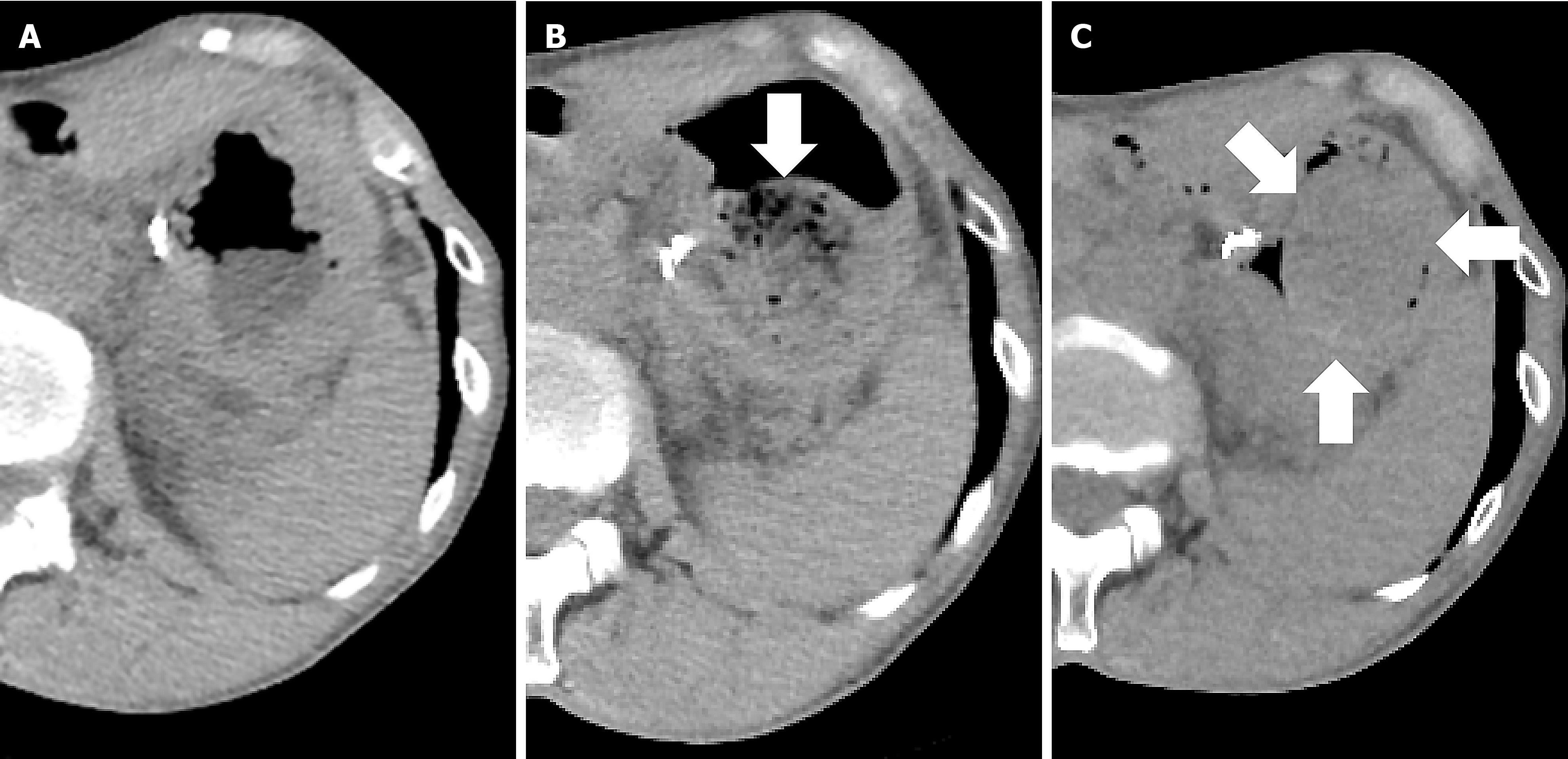
The gastric bezoar was not identified on previous CT scans, even according to the radiologist’s interpretation. Upon reviewing the CT images obtained 12 months previously, no abnormalities were observed in the stomach (Figure 2A). However, a spherical lesion was observed within the stomach on CT performed nine months previously (Figure 2B, arrow). This lesion persisted on CT for six months, with changes observed in its internal structure (Figure 2C, arrows).
Based on the findings of esophagogastroduodenoscopy and infrared spectrometry of the bezoar fragments, the patient was diagnosed with a persimmon bezoar.
Endoscopic fragmentation of the gastric bezoar was performed using alligator forceps (Figure 1C). The procedure was completed in 2.5 hours, during which the bezoar was fragmented into as many small pieces as possible (Figure 1D). Because the patient requested no sedation, an overtube was not used; therefore, repeated insertion and withdrawal of the endoscope were avoided, and bezoar fragment retrieval was not performed using a net device.
On the following day, follow-up esophagogastroduodenoscopy confirmed complete clearance of the bezoar fragments. The patient’s symptoms resolved completely and no recurrence was observed during subsequent monitoring.
When a mass lesion is detected in the stomach, differential diagnoses typically include neoplastic lesions such as gastric cancer, lymphoma, metastatic tumors, and gastrointestinal stromal tumors, as well as other conditions such as hyper
The patient consumed 4-5 persimmons daily for two weeks, after which a gastric bezoar was detected on CT. Persimmon bezoars, also known as diospyrobezoars, are phytobezoars formed by the ingestion of persimmons[2-4]. Predisposing risk factors include prior gastric surgery such as partial gastrectomy, vagotomy, and pyloroplasty, as well as being an older adult or having diabetes[6,7,17,18]. These conditions result in reduced gastric acidity and delayed gastric emptying, which increase the likelihood of bezoar formation. Bezoars can cause abdominal pain, nausea, and vomiting, and obstruct the gastric outlets[19-21]. In some cases, mechanical irritation of the gastric mucosa by bezoars led to the formation of gastric ulcers[5,10], and in other cases, bezoars migrated to the small intestine, causing ileus[11-13]. The patient had a history of excessive persimmon consumption and partial gastrectomy, both of which are risk factors for gastric bezoar formation. Esophagogastroduodenoscopy revealed no gastric ulcers; however, an episode of black stool occurred two months earlier, possibly due to mucosal injury caused by the bezoar.
Infrared spectroscopy is a valuable tool for identifying the components of gastric bezoars[5]. It has been widely used to analyze urinary stones and to provide detailed information on their composition. Similarly, infrared spectroscopy can be applied to gastric bezoars to determine their constituent substances. By identifying the components of gastric bezoars, this technique aids in understanding their formation and contributes to the development of preventive strategies. Early identification and analysis of bezoar composition can lead to better management and potentially reduce the recurrence of bezoars in at-risk patients. In the present case, infrared spectroscopy led to a definitive diagnosis of a persimmon bezoar. We believe that the recurrence of gastric bezoars can be prevented by advising patients to avoid persimmon consumption.
Bezoars can be difficult to detect using CT because their density is often similar to that of the surrounding gastric contents and soft tissues[6-10]. This is particularly true for phytobezoars, which have a density similar to that of food residue and gastric fluid, making them challenging to identify using imaging techniques. Therefore, additional diagnostic methods, such as endoscopy, are required. A previous study revealed that although eight of nine patients underwent CT before endoscopy, the bezoars were mistaken for food debris on CT findings and were overlooked[10]. The bezoar in this patient appeared on CT imaging but was not recognized as an abnormal finding. An interesting aspect of this case is that CT was performed every few months before and after the gastric bezoar formed. A CT scan performed after bezoar formation revealed a spherical mass containing air. However, three months later, the air within the bezoar was no longer visible, and the density became uniform. This suggests that the internal structure of gastric bezoars changes over time. Although there is no method for assessing changes in bezoar hardness over time, bezoars can become harder as time passes after their initial formation.
This case illustrates the temporal changes in gastric bezoars observed on CT and highlights the importance of correlating imaging findings with clinical history and dietary habits. Early recognition and timely endoscopic treatment are crucial for successful management of gastric bezoars, particularly in patients with predisposing risk factors. Notably, changes in the internal density of the bezoar observed on serial CT scans may reflect progressive hardening of the bezoar over time, providing valuable insights into its natural course.
| 1. | Zhang RL, Yang ZL, Fan BG. Huge gastric disopyrobezoar: a case report and review of literatures. World J Gastroenterol. 2008;14:152-154. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 20] [Cited by in RCA: 22] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 2. | Paschos KA, Chatzigeorgiadis A. Pathophysiological and clinical aspects of the diagnosis and treatment of bezoars. Ann Gastroenterol. 2019;32:224-232. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 13] [Cited by in RCA: 35] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 3. | Liu LN, Wang L, Jia SJ, Wang P. Clinical Features, Risk Factors, and Endoscopic Treatment of Bezoars: A Retrospective Analysis from a Single Center in Northern China. Med Sci Monit. 2020;26:e926539. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 4. | Ben-Porat T, Sherf Dagan S, Goldenshluger A, Yuval JB, Elazary R. Gastrointestinal phytobezoar following bariatric surgery: Systematic review. Surg Obes Relat Dis. 2016;12:1747-1754. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 40] [Article Influence: 4.4] [Reference Citation Analysis (0)] |
| 5. | Iwamuro M, Okada H, Matsueda K, Inaba T, Kusumoto C, Imagawa A, Yamamoto K. Review of the diagnosis and management of gastrointestinal bezoars. World J Gastrointest Endosc. 2015;7:336-345. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 214] [Cited by in RCA: 196] [Article Influence: 19.6] [Reference Citation Analysis (5)] |
| 6. | Wang N, Wu X, Lin X, Zhang S, Shen W. Computed tomography with clinical scoring to differentiate phytobezoar from feces in childhood small bowel obstruction. Turk J Pediatr. 2023;65:1002-1011. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Sugimori H, Masaki S, Honjo H, Kudo M, Watanabe T. Visualization of Gastrointestinal Bezoar Movement Causing and Releasing Small Bowel Obstruction on Computed Tomography in a Patient With Diabetes Mellitus. Cureus. 2023;15:e49133. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Wiener BG, Burton RL, Smith SW, Su MK, Biary R, Tay ET. A "madd"-ening confounding: fruit seeds mimicking enteral drug concealment by computed tomography. Clin Toxicol (Phila). 2023;61:559-560. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Parker Cote JL, Gerber BT, Lee H, Miller SN, Meggs WJ. Failure of Computed Tomography (CT) in Detecting an Aspirin Pharmacobezoar: A Case Report. Am J Case Rep. 2022;23:e936752. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 10. | Iwamuro M, Tanaka S, Moritou Y, Inaba T, Higashi R, Kusumoto C, Yunoki N, Ishikawa S, Okamoto Y, Kawai Y, Kitada KI, Takenaka R, Toyokawa T, Okada H. Importance of Second-look Endoscopy on an Empty Stomach for Finding Gastric Bezoars in Patients with Gastric Ulcers. Acta Med Okayama. 2017;71:241-247. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 11. | Dikicier E, Altintoprak F, Ozkan OV, Yagmurkaya O, Uzunoglu MY. Intestinal obstruction due to phytobezoars: An update. World J Clin Cases. 2015;3:721-726. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 48] [Cited by in RCA: 56] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 12. | Kosmidis CS, Mystakidou CM, Varsamis N, Koulouris C, Sevva C, Papadopoulou K, Michael C, Katsios NI, Theodorou V, Miltiadous P, Papadopoulos K, Vlassopoulos K, Zarampouka K, Mantalovas S. Phytobezoar-Induced Mechanical Ileus and Incipient Intussusception: A Case Report. Medicina (Kaunas). 2023;59:1227. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 13. | Pal NL, Panandiker SD, Katiyar G, Vernekar JA. Unusual causes of Small bowel obstruction: a review of the literature and revisited cross-sectional imaging checklist. Emerg Radiol. 2024;31:733-748. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Schulz C, Schütte K, Malfertheiner P. Rare Neoplasia of the Stomach. Gastrointest Tumors. 2015;2:52-60. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 15. | Humphris JL, Jones DB. Subepithelial mass lesions in the upper gastrointestinal tract. J Gastroenterol Hepatol. 2008;23:556-566. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 51] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 16. | Oda, Kondo H, Yamao T, Saito D, Ono H, Gotoda T, Yamaguchi H, Yoshida S, Shimoda T. Metastatic tumors to the stomach: analysis of 54 patients diagnosed at endoscopy and 347 autopsy cases. Endoscopy. 2001;33:507-510. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 165] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 17. | Riaz M, Akbar I, Hassan RE, Ahmad W, Khan H, Khan AU, Khan MH, Shah SS, Tahir A, Tanveer S. Effect of Coca-Cola on the Dissolution of Persimmon-Related Phytobezoar in a Tertiary Care Hospital. Cureus. 2024;16:e54420. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 18. | Gentile M, Illario M, De Luca V, Cestaro G, Velotti N, Sivero S, Musella M. Gastrointestinal bezoars: Review of the literature and report of a rare case of pumpkin seed rectal impaction. Asian J Surg. 2023;46:3432-3436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 19. | Leung E, Barnes R, Wong L. Bezoar in gastro-jejunostomy presenting with symptoms of gastric outlet obstruction: a case report and review of the literature. J Med Case Rep. 2008;2:323. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 10] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 20. | Sulaiman Ambusaidi FM, Al-Yaqoubi M. Gastric bezoar. Int J Pediatr Adolesc Med. 2020;7:199-200. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 21. | Mahir S, Salih AM, Ahmed OF, Kakamad FH, Salih RQ, Mohammed SH, Usf DC, Hassan HA, Abdulla F. Giant phytobezoar; an unusual cause of gastric outlet obstruction: A case report with literature review. Int J Surg Case Rep. 2020;67:154-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (0)] |