Published online Jun 6, 2025. doi: 10.12998/wjcc.v13.i16.103373
Revised: December 30, 2024
Accepted: January 17, 2025
Published online: June 6, 2025
Processing time: 82 Days and 6.6 Hours
Lumbar disc extrusion, a common spinal disorder, is particularly uncommon in its severely displaced form, especially in young patients. This condition can pose diagnostic challenges due to its nonspecific presentation.
A 36-year-old male patient presented with persistent low back pain and radiating leg pain lasting half a month, which had worsened over the previous four days. Lumbar magnetic resonance imaging scans showed an abnormal signal within the vertebral canal at the L3 level, suggesting either a disc cyst or an epidural hematoma. Based on these findings, the patient was provisionally diagnosed with either condition. Surgical exploration was conducted, revealing an extruded lumbar disc, which was subsequently excised. Following surgery, the patient's symptoms completely resolved.
High-grade lumbar disc extrusion in young patients is rare but should be consi
Core Tip: This case report introduces a unique case of high cephalad migration of lumbar disc herniation in a 36-year-old male patient. The patient exhibited persistent low back pain and radiating leg pain, with symptoms worsening over time. Lumbar magnetic resonance imaging scans revealed an abnormal signal within the vertebral canal at the L3 level. Physical examination demonstrated tenderness in the lumbar region, restricted lumbar spine mobility, and numbness and sensory decrement in the right lower limb. Differential diagnoses included discal cysts and spinal epidural hematomas. Due to the rarity and challenging nature of the lesion's location, open surgery was selected as the treatment option. Intraoperative ultrasonography facilitated precise localization of the lesion, which was successfully resected. The postoperative outcome was favorable, with complete resolution of symptoms and a Visual Analog Scale score of 0. This case underscores the importance of considering atypical pathogenic mechanisms in young patients with lumbar disc herniation and highlights the role of intraoperative ultrasonography in guiding surgical management.
- Citation: Zhou JG. Diagnosis and surgical challenges of extremely severe head and lumbar disc herniation in young patients: A case report. World J Clin Cases 2025; 13(16): 103373
- URL: https://www.wjgnet.com/2307-8960/full/v13/i16/103373.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i16.103373
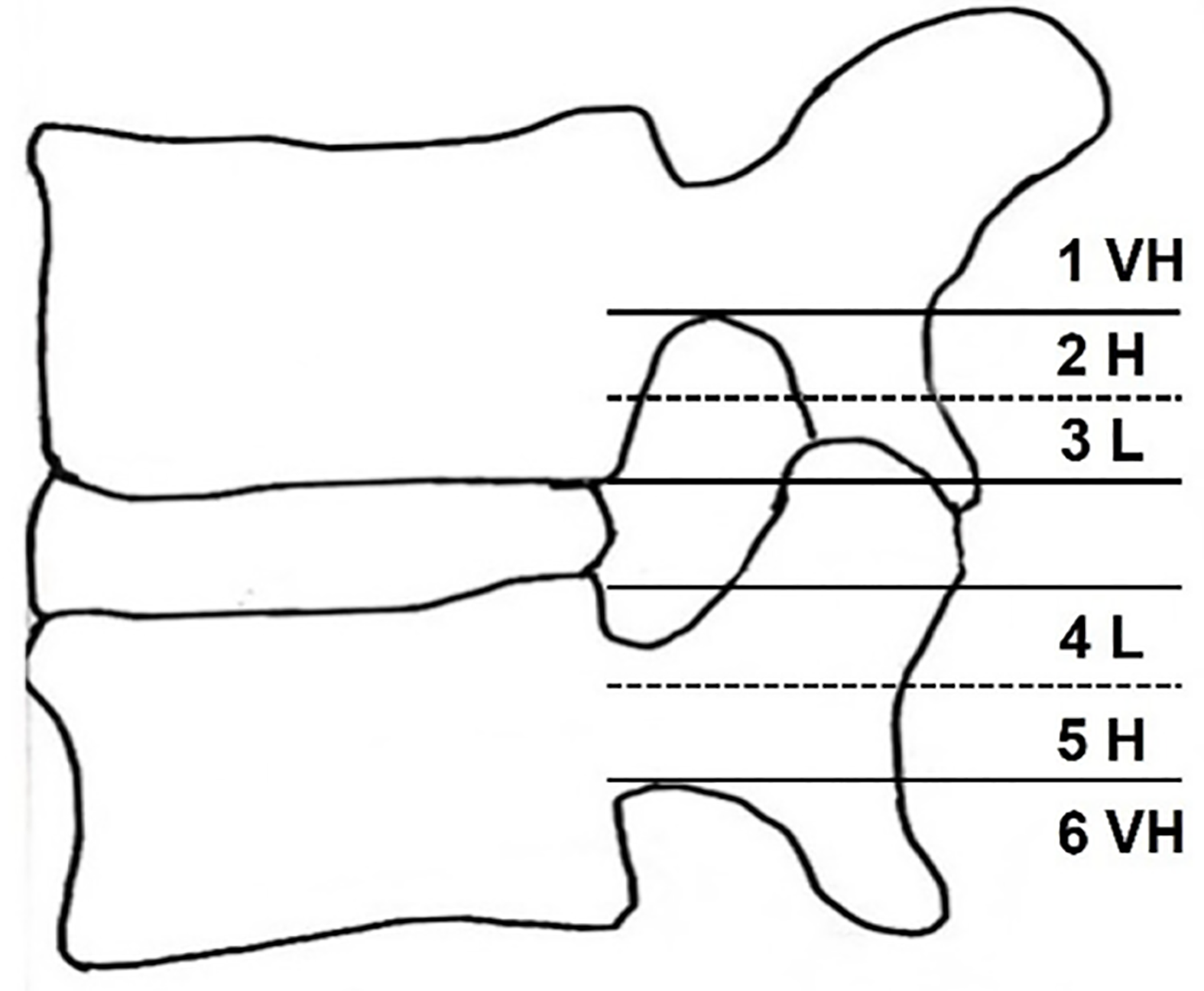
Lumbar disc herniation (LDH) is a prevalent spinal disorder characterized by the protrusion of disc tissue beyond the annulus fibrosus and posterior longitudinal ligament, invading or displacing into the epidural space, potentially compressing the spinal cord or nerves and eliciting a variety of clinical manifestations[1]. The incidence of this condition is approximately 1%, with the most common involvement observed at the L4/5 and L5/S segments. Regarding patient age distribution, the average ages for LDH at the L2/3 and L3/4 segments are 59.6 years and 59.5 years, respectively. In contrast, those for the L4/5 and L5/S segments are 49.5 years and 44.1 years, respectively, indicating that the incidence of protrusions increases at segments above L4/5 as age advances. Furthermore, surgical intervention is more frequently performed in the 20 to 40 age group and among male patients[2,3]. The medical community classifies lumbar disc extrusion into six grades on the sagittal plane of magnetic resonance imaging (MRI) based on the specific direction and degree of extrusion (Figure 1 and Table 1)[4]. Among these grades, very high-cephalad migration of lumbar disc extrusion is a unique and rarely encountered subtype in clinical practice, particularly in young patients.
| Grade | Direction and degree | Range of migration distance |
| 1 | Superior very high | Beyond the inferior margin of the upper pedicle |
| 2 | Superior high | From the inferior margin of the upper pedicle to the midpoint between the inferior margin of the upper pedicle and superior disc margin |
| 3 | Superior low | From the midpoint between the inferior margin of the upper pedicle and superior disc margin to the superior disc margin |
| 4 | Inferior low | From the inferior disc margin to the midpoint between the inferior margin of the lower pedicle and inferior disc margin |
| 5 | Inferior high | From the midpoint between the inferior margin of the lower pedicle and inferior disc margin to the inferior margin of the lower pedicle |
| 6 | Inferior very high | Beyond the inferior margin of the lower pedicle |
This study aims to provide clinicians with valuable references for diagnosing and treating this unique condition, particularly in young patients, through a detailed case report of a young male patient experiencing very high-cephalad migration of lumbar disc extrusion. This case analysis will enhance our understanding of this specific type of lumbar disc extrusion, allow for the optimization of treatment plans, and ultimately contribute to better treatment outcomes and an improved quality of life for patients.
Persistent low back pain and radiating leg pain that had persisted for half a month, with a recent exacerbation over the past four days.
A 36-year-old male driver, with a body mass index (BMI) of 31.14, presented to the hospital with persistent low back pain and radiating leg pain that had persisted for half a month, with a recent exacerbation over the past four days. The primary symptoms included low back pain, numbness, and a sensation of swelling in the outer region of the right lower leg. These symptoms were partially alleviated when the patient rested. The preoperative visual analog scale (VAS) score was recorded as 30. The patient had no significant previous medical history.
The patient had no significant previous medical history.
No significant personal or family history is present.
Upon physical examination, no spinal deformities were observed. Specifically, tenderness was detected at the L3/4 and L4/5 intervertebral spaces, while axial percussion pain was absent. Restricted range of motion in the lumbar spine was noted. In terms of sensory examination, the right lower limb exhibited numbness and a sensation of swelling in the lateral region, accompanied by a decrease in superficial sensation in the posterolateral area. Furthermore, the right straight leg raising test was positive at 30 degrees, and the strengthening test was also positive. Specifically, dorsiflexion muscle strength of the right great toe was reduced. The left lower limb examination results were normal. Bowel and bladder functions were within normal limits.
Aspartate aminotransferase 61.20 U/L, alanine aminotransferase 100.30 U/L, total cholesterol 6.56 mmol/L, triglycerides 11.20 mmol/L.
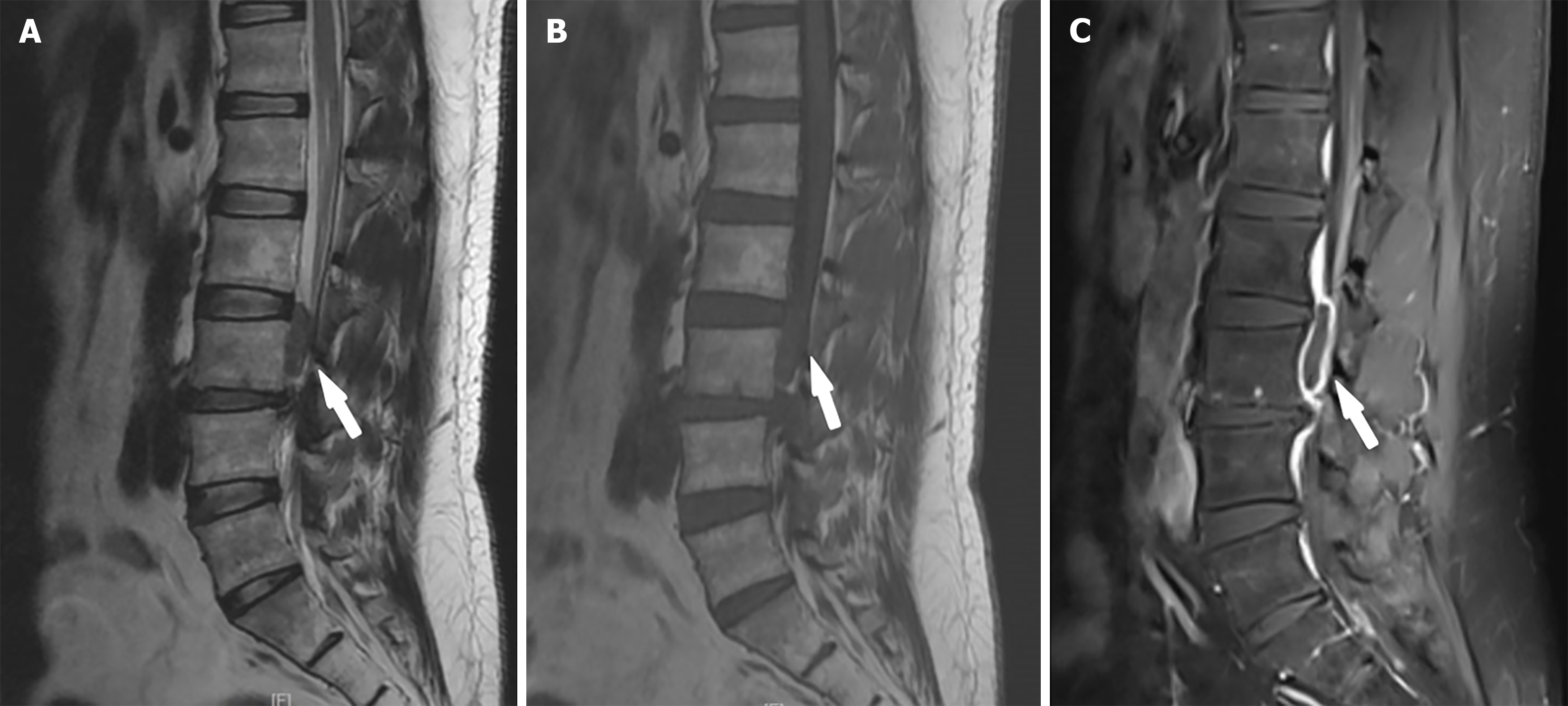
Diagnostic imaging, including plain and enhanced lumbar MRI scans, revealed a significant reduction in the height of the L3-L4 intervertebral disc. There was a long T1 short T2 signal in the vertebral canal at the level of the L3 vertebra (Figure 2). Enhancement showed an elliptical abnormal signal in the epidural space at the level of the L3 vertebra, with linear enhancement at the edge and no enhancement in the center. The lesion, measuring 15.2 mm × 11.7 mm × 33.5 mm, caused compression and deviation of the dural sac to the left (Figures 2 and 3). The patient's blood glucose levels were normal, and no nuclear magnetic resonance imaging of the head or entire spine was conducted. Preoperative diagnosis considerations were 1. Disc cyst; 2. Epidural hematoma.
Lumbar disc extrusion. Based on the patient's age, clinical manifestations, physical examination, and imaging findings, a definitive diagnosis poses challenges.
Recommendation for Open Surgical Intervention Given the advantages of open surgery in terms of facilitating exploration, avoiding intraoperative exposure difficulties, and reducing the risks of postoperative cerebrospinal fluid leakage or the need for additional spinal canal decompression in special circumstances, it is recommended to proceed with open surgical treatment.
Preoperative and Postoperative Considerations Comprehensive preoperative evaluations are necessary to delineate the extent and precise location of the lesion. Following surgery, close monitoring of neurological function recovery is essential, and early initiation of rehabilitation training is recommended to facilitate patient recovery.
Importance of Postoperative Lifestyle Adjustment and Lumbar Muscle Exercise The significance of adjusting the patient's lifestyle and enhancing lumbar muscle exercise after surgery cannot be overlooked, as these measures are crucial for preventing recurrence of the condition.
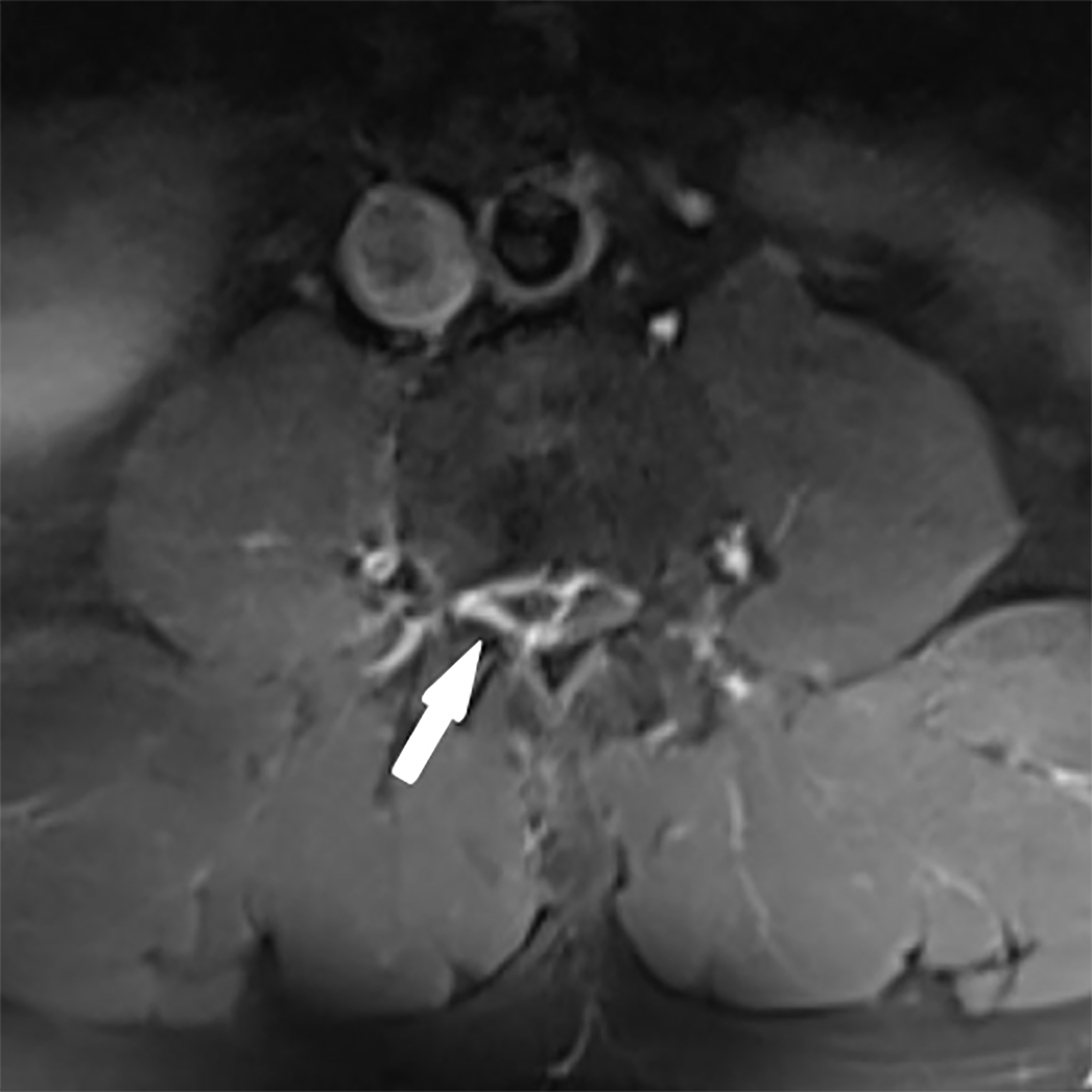
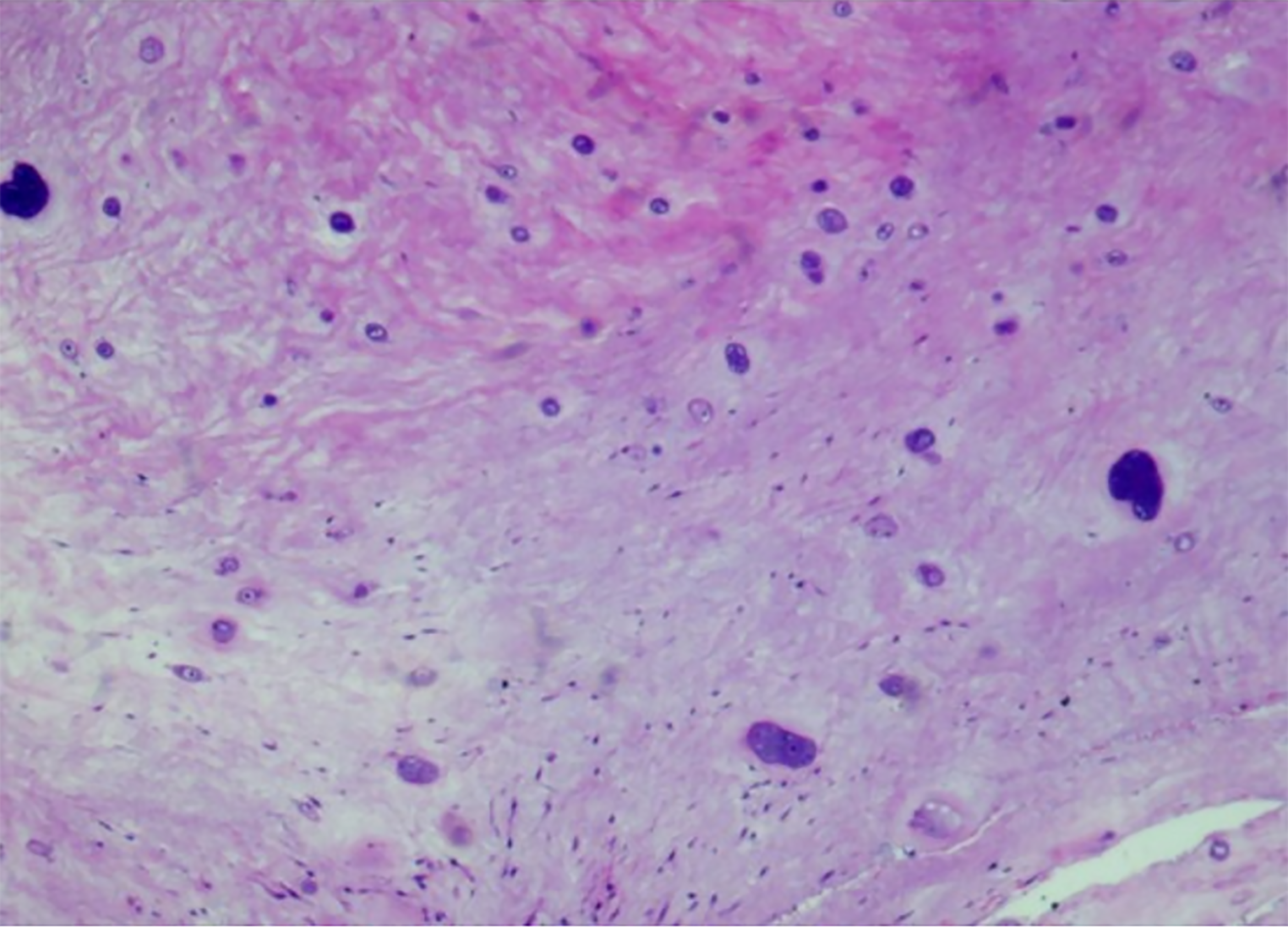
Open surgery was performed. Intraoperative ultrasound examination revealed that the lesion was located in the plane of the L3 vertebra, ventral to the vertebral canal, with a low signal echo, indicating its distinct characteristics (Figure 4). The dural sac was pulled to the left and positioned posteriorly with high tension, making exposure difficult. After incision of the dura mater to release cerebrospinal fluid, the intradural pressure decreased, allowing for exposure. The extruded disc was found on the shoulder and axillary regions of the L3 nerve root, appearing slightly yellowish, having a brittle yet resilient texture, and lacking blood supply (Figure 5). The extruded disc was excised in pieces until complete removal was confirmed, and the spinous process was reduced.
Postoperative lumbar MRI revealed the repositioning of the dural sac at the level of the L3 vertebra (Figure 6). Pathological examination revealed degenerated disc nucleus pulposus tissue (Figure 7). One week post-surgery, the patient's symptoms fully resolved. The VAS score, assessed two weeks post-surgery, was 0. Three months subsequent to the procedure, the patient reported no recurrence of pain or discomfort in the back and legs.
LDH is a complex and variable pathological process, with displacement occurring in multiple directions, including cephalad and caudal. Research on the direction of LDH displacement has reported varying data from different research teams. Studies by Igarashi et al[5] found that the proportion of cephalad and caudal displacements was 27.8% and 72.2%, respectively, and noted a significant increase in the incidence of cephalad displacement in the upper lumbar discs of older patients, possibly related to changes in the anterior epidural space (AES) and sedentary lifestyles[5,6]. In contrast, Ahn et al[7] reported different proportions of 46.53% and 53.47%, but their findings did not align with those of other studies. Lee et al[8] reported that cephalad displacement of LDH (Grade 1 + 2) accounted for only 3.5%, significantly lower than other grades. Furthermore, Ahn et al[7] reported that surgical LDH cases were most common in Grade 4, followed by Grade 5 and Grade 1. However, Ahn et al[7] data only indicated a higher surgical rate for extremely cephalad displacement of LDH (Grade 1) and did not accurately reflect the proportion of LDH direction and severity. These differences primarily stem from variations in sample size and research methods.
Although all existing studies have yet to provide precise ratios or significant differences in the age distribution of cephalad displacement, they have broadly mentioned the prevalence of this phenomenon among older patients and have accordingly put forward corresponding theoretical support. Notably, the occurrence in this young patient case suggests that young individuals may also be susceptible to this condition. Therefore, it is crucial to pay close attention to lumbar health in young people, especially those in high-risk groups such as those with occupations requiring prolonged sitting, obesity, and poor trunk muscle strength and condition.
AES refers to the narrow space between the dura mater and the bony membrane of the vertebral canal as well as the posterior longitudinal ligament. Igarashi et al[5] found that the AES at the L2–L3 segment is relatively spacious, and the fatty tissue within the space tends to atrophy with age. These factors contribute to the higher incidence of cephalad displacement of lumbar discs in older individuals. Additionally, sedentary behavior in older adults weakens the effect of gravity on herniated material, increasing the pressure within the spinal canal, which may facilitate cephalad displacement of herniated disc tissue[5]. Besides age and lifestyle, factors such as trunk muscle status[9], intervertebral stress distribution[10], and anatomical variations[11] also have direct impacts, further complicating the direction of LDH displacement. To date, there have been no specific reports detailing the occurrence of cephalad displacement in young patients, indicating that this phenomenon is relatively uncommon within the young population and, consequently, merits thorough investigation. Notably, the presentation of LDH in the lower lumbar spine in this young patient prompts us to consider the necessity of exploring additional potential pathogenic mechanisms.
In terms of diagnosis, although leg and back pain are common symptoms of LDH, they are not essential for diagnosis. MRI is the preferred imaging modality, capable of clearly demonstrating LDH. However, owing to specific conditions such as ring enhancement, MRI results may lead to diagnostic difficulties. Therefore, a thorough assessment that integrates clinical symptoms, physical signs, and imaging studies is crucial for an accurate diagnosis.
It is noteworthy that discal cysts and spinal epidural hematomas can be easily confused during diagnosis. Owing to the unclear pathogenesis of discal cysts, surgical procedures have revealed the presence of hemorrhage within these cysts, along with complex and variable intracystic components. On contrast-enhanced T1-weighted imaging, both discal cysts and spinal epidural hematomas may exhibit similar radiological characteristics, specifically manifesting as a thickened rim of enhancement. The liquid content within the cysts varies widely, ranging from serous to mucinous, resulting in a diversity of signal intensities within the cysts.12,13 This variability in signal intensity undoubtedly increases the difficulty in differentiating discal cysts from other conditions, particularly LDH that may present with overlapping symptoms.
Regarding treatment, traditional Chinese medicine (TCM) physiotherapy and Western surgical interventions have their respective advantages. TCM massage and myofascial manipulation can regulate the body, relax muscles, strengthen bones, prevent muscle atrophy, improve lumbar flexibility, adjust local muscle tension, and increase spinal stability, thereby preventing the occurrence or recurrence of LDH[9]. Healthy lifestyles, such as avoiding prolonged sitting, enhancing exercise, and strengthening lumbar and back muscle exercises, can benefit LDH patients[14]. Hu et al[15] reported sequestered LDH can regress within a relatively short timeframe without surgery.
In Western medicine, advances in techniques and instrumentation have gradually shifted LDH surgery from open procedures to minimally invasive approaches. Percutaneous endoscopic discectomy is currently a safe and effective minimally invasive surgical method, but it is not suitable for all patients. Lee et al[8], Yu et al[16], and Wang et al[17] argue that minimally invasive surgery (MIS) for highly cephalad displaced LDH may face challenges such as anatomical barriers and the risk of nerve injury, which may prevent complete resection of the herniated material. Therefore, when preoperative diagnosis is uncertain, the selection of surgical approach becomes particularly crucial. While MIS offers advantages such as reduced trauma and faster recovery, it may pose risks including exposure difficulty, cerebrospinal fluid leakage, and the need for additional decompression in certain scenarios. Notably, in cases with unusual lesion locations, such as the high-grade upward migration of lumbar discs observed in this instance, MIS may fail to achieve optimal exposure and resection. Consequently, open surgery was chosen in this case. Open surgery provides a clear and direct view of the vertebral canal and the protruding disc, effectively mitigating the risks associated with MIS. Through open surgery, surgeons can visually assess the lesion and perform precise resection and decompression. Furthermore, the application of intraoperative ultrasonography played a pivotal role. The intraoperative ultrasonography accurately pinpointed the lesion, which was located within the third vertebral body plane, along the ventral aspect of the spinal canal. This technique not only facilitated the accurate identification and localization of the protruding disc but also served as a crucial reference for surgical manipulation. Although MIS holds advantages in certain aspects, it is not applicable in all situations. When choosing a surgical approach, factors such as the patient's specific condition, lesion location, and surgical risks should be thoroughly considered. For the patient in this case, open surgery combined with intraoperative ultrasonography represented an effective and safe treatment option.
Firstly, the present study is inherently limited to a single case report, which fundamentally constrains the generalizability of the findings. Thus, caution should be exercised when extrapolating the results to other scenarios. Secondly, the diagnostic process was challenging because of the uncommon clinical manifestations of the disease. This led to preoperative diagnostic considerations that did not definitively point to LDH, highlighting the complexity and potential for misdiagnosis in such cases. Furthermore, the surgical approach employed in this study was open surgery, which may not reflect the most advanced or minimally invasive surgical techniques currently available for LDH. Advances in surgical techniques and instrumentation may offer alternative treatment options with potential benefits in reducing morbidity and shortening recovery time. Lastly, the long-term follow-up data on patient prognosis and outcomes are limited. Although the patient's symptoms improved within one week post-surgery, long-term follow-up is crucial for comprehensively assessing the durability of treatment effects and the patient's overall functional recovery.
LDH and displacement represent a complex yet intriguing research field, with numerous unknowns awaiting further exploration. Through rigorous research and the accumulation of practical experience, we can gain a deeper understanding of this condition and optimize its management, ultimately enhancing therapeutic outcomes and quality of life for patients. Additionally, it is imperative to enhance public health education, particularly among younger individuals, to raise awareness and understanding of lumbar health, which holds significant importance in preventing the occurrence of lumbar disc prolapse and related disorders.
| 1. | Fardon DF. Nomenclature and classification of lumbar disc pathology. Spine (Phila Pa 1976). 2001;26:461-462. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 64] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Shiga Y. The Essence of Clinical Practice Guidelines for Lumbar Disc Herniation, 2021: 1. Epidemiology and Natural Course. Spine Surg Relat Res. 2022;6:319-321. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 3. | Dammers R, Koehler PJ. Lumbar disc herniation: level increases with age. Surg Neurol. 2002;58:209-12; discussion 212. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 44] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 4. | Ahn Y, Kim JE, Yoo BR, Jeong YM. A New Grading System for Migrated Lumbar Disc Herniation on Sagittal Magnetic Resonance Imaging: An Agreement Study. J Clin Med. 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Igarashi T, Hirabayashi Y, Shimizu R, Saitoh K, Fukuda H, Mitsuhata H. The lumbar extradural structure changes with increasing age. Br J Anaesth. 1997;78:149-152. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 50] [Cited by in RCA: 50] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 6. | Daghighi MH, Pouriesa M, Maleki M, Fouladi DF, Pezeshki MZ, Mazaheri Khameneh R, Bazzazi AM. Migration patterns of herniated disc fragments: a study on 1,020 patients with extruded lumbar disc herniation. Spine J. 2014;14:1970-1977. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 46] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Ahn Y, Jeong TS, Lim T, Jeon JY. Grading system for migrated lumbar disc herniation on sagittal magnetic resonance imaging: an agreement study. Neuroradiology. 2018;60:101-107. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 8. | Lee S, Kim SK, Lee SH, Kim WJ, Choi WC, Choi G, Shin SW. Percutaneous endoscopic lumbar discectomy for migrated disc herniation: classification of disc migration and surgical approaches. Eur Spine J. 2007;16:431-437. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 137] [Cited by in RCA: 180] [Article Influence: 9.5] [Reference Citation Analysis (0)] |
| 9. | Xu J, Ding X, Wu J, Zhou X, Jin K, Yan M, Ma J, Wu X, Ye J, Mo W. A randomized controlled study for the treatment of middle-aged and old-aged lumbar disc herniation by Shis spine balance manipulation combined with bone and muscle guidance. Medicine (Baltimore). 2020;99:e23812. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 10. | Kirnaz S, Capadona C, Wong T, Goldberg JL, Medary B, Sommer F, McGrath LB Jr, Härtl R. Fundamentals of Intervertebral Disc Degeneration. World Neurosurg. 2022;157:264-273. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 123] [Article Influence: 30.8] [Reference Citation Analysis (0)] |
| 11. | Pouriesa M, Fouladi RF, Mesbahi S. Disproportion of end plates and the lumbar intervertebral disc herniation. Spine J. 2013;13:402-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 12. | Lee HK, Lee DH, Choi CG, Kim SJ, Suh DC, Kahng SK, Roh SW, Rhim SC. Discal cyst of the lumbar spine: MR imaging features. Clin Imaging. 2006;30:326-330. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 56] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 13. | Al-Mutair A, Bednar DA. Spinal epidural hematoma. J Am Acad Orthop Surg. 2010;18:494-502. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 73] [Article Influence: 4.9] [Reference Citation Analysis (0)] |
| 14. | Deyo RA, Mirza SK. CLINICAL PRACTICE. Herniated Lumbar Intervertebral Disk. N Engl J Med. 2016;374:1763-1772. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 168] [Cited by in RCA: 220] [Article Influence: 24.4] [Reference Citation Analysis (1)] |
| 15. | Hu C, Lin B, Li Z, Chen X, Gao K. Spontaneous regression of a large sequestered lumbar disc herniation: a case report and literature review. J Int Med Res. 2021;49:3000605211058987. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 16. | Yu Y, Jiang Y, Xu F, Mao Y, Yuan L, Li C. A novel vertebral trench technique (VTT) involving transforaminal endoscopic lumbar foraminotomy (TELF) for very highly up-migrated lumbar disc herniation above L5. BMC Musculoskelet Disord. 2021;22:693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Wang D, Xu JC, Cheng W, Gao WS, Bao JH, Zhu L, Hu QF, Pan H. [Treatment of migrated lumbar intervertebral disc herniation by percutaneous spinal endoscopy through bone tunnel]. Zhongguo Gu Shang. 2021;34:994-1001. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |