Published online Jun 6, 2025. doi: 10.12998/wjcc.v13.i16.101732
Revised: December 24, 2024
Accepted: January 15, 2025
Published online: June 6, 2025
Processing time: 138 Days and 14.8 Hours
Alagille syndrome is a rare autosomal dominant genetic disorder involving multiple organ systems. Its most common manifestations are chronic cholestasis caused by intrahepatic bile duct deficiency and severe hypercholesterolemia as a result of impaired cholesterol metabolism. This report describes a patient with Alagille syndrome in whom a JAG1 mutation was detected by whole-exome sequencing.
The patient presented with severe hypercholesterolemia, biliary and hepatic impairment, pruritus, and triangular facial features. Mutations in the JAG1 gene, which encodes the Notch signaling pathway, were detected by whole-exome sequencing, leading to a diagnosis of Alagille syndrome. The patient was treated using a combination of traditional Chinese and Western medicines. Her chole
The possibility of Alagille syndrome should be considered in children who present with abnormal liver function and severe hypercholesterolemia. Genetic testing is needed to screen for disease-causing mutations and the disease can be treated with Traditional Chinese medicine.
Core Tip: The incidence of Alagille syndrome is a rare disease, and no doctor has ever tried traditional Chinese medicine (TCM) in the treatment of Alagille before, demonstrating the effectiveness of TCM in the treatment of blood lipids. Clinicians need to be careful to ask about the time of onset of the disease when seeing patients, and if they encounter severe hyper lipidaemia they can do genetic testing to rule out inherited metabolic diseases.
- Citation: Jiang CX, Meng YL, Chen D, Shi LP, Yang G, Guo Y, Zhang B, Zhai ZC, Wu ZJ, Liu TN, Wang ZJ, Tian X, Su PY. Genetic disorders leading to severe hyperlipidemia in children: A case report. World J Clin Cases 2025; 13(16): 101732
- URL: https://www.wjgnet.com/2307-8960/full/v13/i16/101732.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i16.101732
Alagille syndrome is a rare autosomal dominant genetic disorder with an incidence of approximately 1 in 70000[1]. This syndrome is a complex congenital disorder characterized by the presence of five primary features: A reduced number of small bile ducts within the liver, narrowing of the pulmonary artery, abnormal butterfly-shaped vertebrae, an ophthalmic condition known as posterior embryotoxon, and a characteristic triangular facial features. Additional manifestations may include cognitive impairment, kidney abnormalities, and delayed growth. Alagille syndrome is associated with mutations in two genes, namely, JAG1 and NOTCH2[2]. This report describes a child with chronic cholestasis and severe hypercholesterolemia in whom a JAG1 mutation was found by whole-exome sequencing. Her symptoms were alleviated by nutritional guidance and treatment with traditional Chinese medicine (TCM) and Western medicine.
The patient was brought to our blood lipid clinic by her parents at the age of 11 years and 7 months with a 10-year history of hyperlipidemia and abnormal liver function.
During the first 50 days after birth, she developed yellow skin and was noticed to have a poor appetite. Laboratory tests at that time had suggested abnormal liver function and severe hyperlipidemia. The parents had taken her to many hospitals, where she received multiple successive treatments to help her liver function, including vitamins, bile acid sequestrants, and lipid-lowering agents. Her hepatic function and severe hyperlipidemia did not improve, and her symptoms continued. On presentation at our facility, she had a poor appetite as well as a body weight that was lower than expected for her age. Her urine was yellowish, and she had intermittent loose stools.
Laboratory investigations performed on day 50 after birth showed the following: Alanine aminotransferase (ALT) 101 U/L, aspartate aminotransferase (AST) 130 U/L, total bilirubin 169.5 μmol/L, gamma-glutamyl transferase (GGT) 360 U/L, alkaline phosphatase (ALP) 540 U/L, direct bilirubin 90.5 μmol/L, and indirect bilirubin 79.0 μmol/L. Abdominal ultrasound showed that the bile duct stenosis was narrow and that the liver was normal. Echocardiography showed an atrial septal defect (left to right shunt). She was diagnosed with infantile hepatitis syndrome and an atrial septal defect. The jaundice subsided after treatment with compound glycyrrhizin tablets, ornithine aspartate granules, and biphenyl diester dropping pills, but her ALT, AST, and ALP levels remained elevated. Further examinations showed that her total cholesterol levels were higher than normal, reaching a maximum of 15.38 mmol/L. She had undergone atrial septal defect closure surgery at another hospital 1 year earlier, and there was no obvious arrhythmia, cyanosis, or palpitations. She continued treatment with glycyrrhizin, glucuronolactone, ursodeoxycholic acid, vitamin supplementation, polyene phosphatidylcholine, and ezetimibe. However, her ALT, AST, ALP, GGT, total cholesterol, and low-density lipoprotein cholesterol levels remained higher than normal on several repeat examinations (Table 1).
| Age | ALT (IU/L) (0-40) | AST (IU/L) (0-40) | GGT (IU/L) (7-32) | TBIL (IU/L) (5.13-22.24) | DBIL (IU/L) (1.7-10.2) | TC mmol/L (2.83-5.2) | LDLC mmol/L (2.07-3.37) | ALP (IU/L) (50-135) | Medicine |
| 50 days | 530 | 773 | 1362 | 54.6 | 34.4 | 15.38 | / | 1203 | Compound glycyrrhizin, Yin lotus clear liver particles |
| 2 years and 10 months | 186 | 148 | 643 | 24.3 | 16.3 | 16.93 | 14.0 | 487 | Vitamin B, vitamin C, polyene phosphatidylcholi-ne, ursodeoxycholic acid |
| 11 years and 7 months | 200 | 116 | 682 | / | / | 12.08 | 4.81 | 497 | Drug withdrawal |
| 11 years and 8 months | 77 | 64 | 264 | / | / | 9.28 | 5.54 | 115 | Ursodeoxycholic acid, vitamin B, Traditional Chinese medicine preparation |
| 11 years and 9 months | 151 | 77 | 597 | 16.8 | 8.7 | 8.7 | 5.29 | 124 | Membrane of Chickens Gizzard |
The patient was born at term with no abnormalities detected on prenatal examination. She received regular vaccinations and had no hereditary diseases. The parents denied a family history of hereditary diseases or consanguinous marriage. The parents and brother were in good health.
The patient’s height was 152 cm and weight was 36 kg, giving a body mass index of 15.58 (calculated as kg/m2). The patient has a prominent forehead, slightly deep-set eye sockets with no eyelid or corneal abnormalities, narrowed eye fissures, a bulbous nose, pointed chin, and dark skin, with scattered miliary rashes on the limbs, scratches and pigmentation on both upper limbs, and obvious pruritus (Figure 1A-C). There was no yellowing of the skin or xanthelasma. The heartbeat are strong and rhythmic, and a 2/6 systolic murmur was heard between the second and third intercostal spaces at the left sternal border.
The results of the laboratory tests at the age of her 50 days and the treatment prescribed were reported earlier. After treatment at our lipid clinic in 2023, her ALT, AST, ALP, and GGT levels trended downwards, with a total cholesterol of 9.28–12.08 mmol/L and a low-density lipoprotein cholesterol of 4.16–6.05 mmol/L (Table 1). Analysis of body composition showed increased body fat and body weight (Table 2).
| Body composition | 11 years and 6 months | 11 years and 8 months | Normal range |
| Total body water (L) | 20.2 | 20.7 | 22.3-27.3 |
| Protein (kg) | 5.3 | 5.6 | 6.0-7.4 |
| Inorganic salt (kg) | 2.14 | 2.14 | 2.07-2.53 |
| Body fat (kg) | 8.4 | 10.3 | 7.2-14.4 |
| Weight (kg) | 36.04 | 38.7 | 36.4-49.2 |
Abdominal ultrasound showed that the bile duct stenosis was narrow and that the liver was normal. Echocardiography showed an atrial septal defect (left to right shunt).
After considering the patient's condition and test results, she was thought to have a severe bile excretion problem and severe hyperlipidemia. Genetic testing identified mutations, and a literature review indicated that she had Alagille.
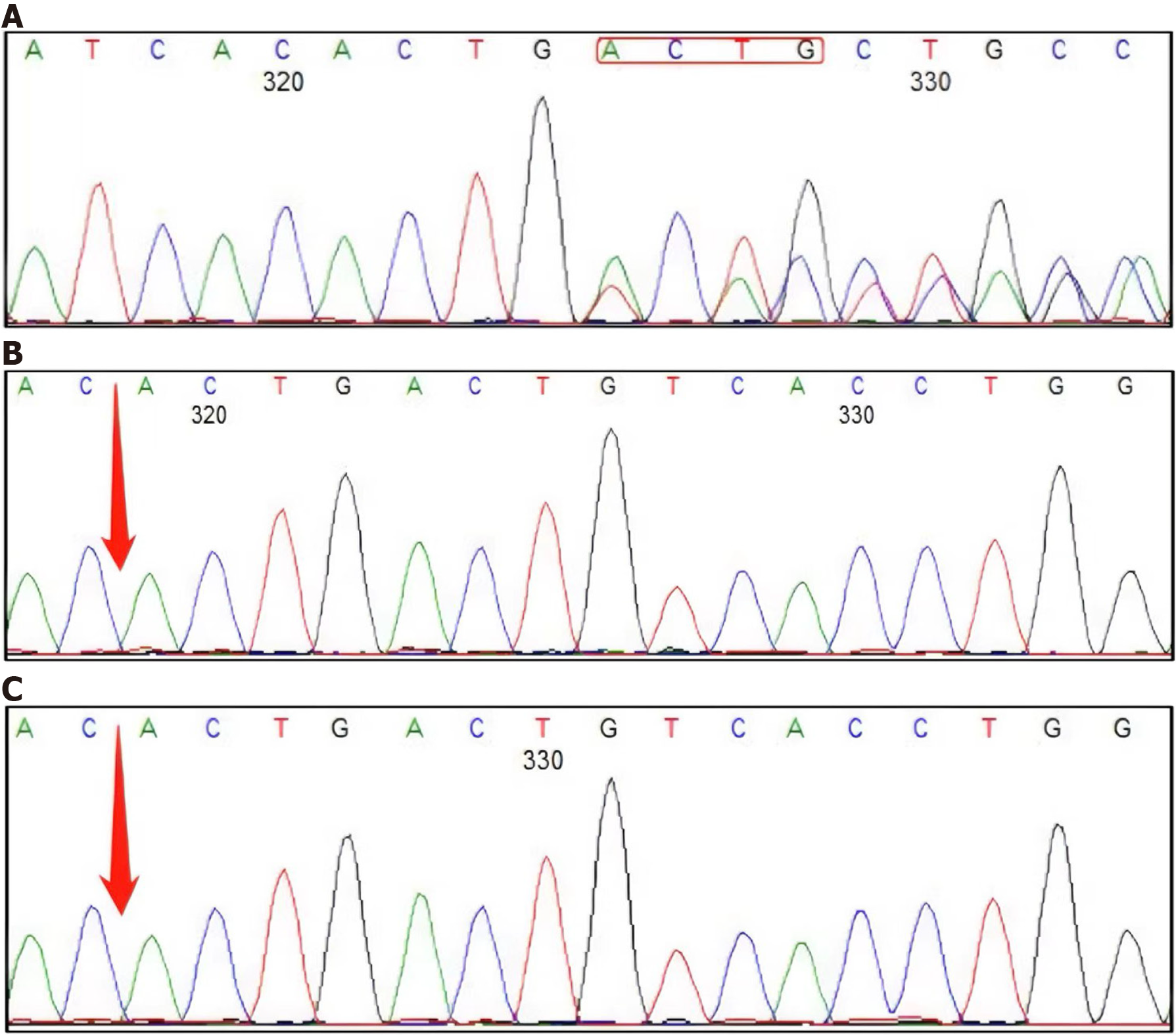
Further whole-exome genetic testing revealed a c.2122_2125del (p.Gln708ValfsTer34) mutation in exon 17 of JAG1 (Figure 2A), which can cause type 1 Alagille syndrome. The JAG1 locus was sequenced for the patient's parents and no mutation was found (Figure 2B and C). According to the clinical manifestations and results of genetic testing, the patient was diagnosed with Alagille syndrome.
A nutritionist (Dong Chen) and a lipidologist (Peng-Yu Su) recommended continued use of bicyclol to protect liver function, ezetimibe to lower lipid levels, ursodeoxycholic acid to promote excretion of bile, and nutritional guidance. A TCM physician (Yu-Lin Meng) recommended a Chinese herbal tonic (Chaihu Shuohexuan San) to ease the liver, regulate qi, and promote excretion of bile (Table 3).
| Age | Name of Chinese medicine | Dosages | Name of Chinese medicine | Dosages | Name of Chinese medicine | Dosages | Name of Chinese medicine | Dosages |
| 11 years and 8 months | Radix; Bupleuri | 10 g | Aurantii; Fructus; Immaturus | 10 g | Stir-fried; Atractylodes macrocephala; Koidz | 12 g | Poria | 20 g |
| Ligusticum chuanxiong; Hort | 10 g | Angelica sinensis | 15 g | Chinese Hawthorn Fruit (charred | 15 g | Burnt malt | 15 g | |
| Dried orange peel used in Chinese medicine | 10 g | Paeonia lactiflora | 10 g | Glycyrrhiza uralensis; Fisch | 3 g | |||
| 11 years and 9 months | Membrane of Chickens Gizzard | 5g (take it with lunch) | ||||||
The patient’s liver function tests decreased and her symptoms of cholestasis and pruritus improved. Considering her poor appetite, she was started on chicken gizzard membrane powder under the guidance of nutritionists and specialists in TCM to strengthen the stomach and promote digestion of food (Table 3). By July 2023, her appetite had improved, her bilirubin level was within normal limits, and her cholesterol level was lower than it had been in April 2023 (Table 1), and her itchy skin was reduced and the scratches on her arms disappeared (Figure 1). We plan to adjust the treatment regimen according to her lipid profile at future follow-up visits.
The diagnostic criteria for Alagille syndrome include five main clinical features[1,2], namely, chronic cholestasis, congenital heart disease, an embryonic retrocorneal ring, spinal deformity (butterfly vertebrae or hemivertebrae), and a distinctive facies (broad forehead, deep-set eyes, hypertelorism, and pointed chin). Alagille syndrome involves multiple organs and causes systemic lesions[3]. Our patient had elevated cholesterol and obvious cholestasis since birth that persisted after multiple drug treatments. In Aprill 2023, we performed whole-exome sequencing for this child and found a mutation at JAG1 c.2122_2125. JAG1 encodes the ligand of the Notch2 receptor, which is involved in expression of the Notch signaling pathway. This pathway regulates the development of the intrahepatic bile ducts, craniofacial structures, the heart, kidney, and spine, and the vascular system[2,4]. Therefore, disorders of the Notch signaling pathway can lead to chronic cholestasis, absence of the intrahepatic bile ducts, a characteristic facies, a posterior embryonic corneal ring, butterfly-shaped vertebrae, and other diseases[5]. JAG1 is located at the p12.2 position on chromosome 20 and has a length of 36316 bases with 26 exons. A mutation in exon 17 of JAG1 was detected in our patient, which caused a frameshift mutation at amino acid position 708 of the encoded protein, resulting in a premature stop codon at amino acid position 741, which was predicted to cause nonsense-mediated degradation of mRNA and loss of function.
JAG1 mutation causes loss of the intrahepatic bile ducts, resulting in abnormal excretion of cholesterol and significant increases in low-density lipoprotein cholesterol and total cholesterol. After treatment with ursodeoxycholic acid and vitamin B with adjustments in TCM as recommended by the nutritionist and TCM physician, the liver function tests decreased and the patient’s cholestasis and symptoms of pruritus were alleviated. Considering her poor appetite, she was started on ChaiHu shugan powder, a TCM that regulates qi and strengthens the spleen and stomach. Treatment with chicken gizzard membrane powder strengthened the stomach and promote digestion of food. The child's appetite improved, her bilirubin level returned to normal, and her cholesterol levels decreased. We believe that TCM may have the effect of regulating lipid metabolism. Chicken gizzard membrane powder contains multiple substances, including pepsin and gastric lipase. These enzymes can promote digestion of food and accelerate gastric emptying. Polysaccharides, polypeptides, and other active ingredients in this powder can regulate gastrointestinal motility and improve glucose and lipid metabolism, reducing cholesterol and atherosclerotic plaque[6]. However, the mechanism is not clear.
Conventional treatment of Alagille syndrome includes protection of the liver[4], decreasing lipid levels, reduction of cholestasis, and relief of pruritus. There are evidence showing that a combination of TCM and Western medicine or TCM conditioning is more effective than Western medicine alone in terms of reducing the risk of adverse reactions to oral medication[7]. The advantages of TCM in the treatment of cholestatic diseases have already been demonstrated[8]. The Chai Hu Chinese herbal formula can promote excretion of bile and alleviate itching, while Chuan Xiong and Angelica sinensis promote circulation of blood and hawthorn helps peristalsis and promotes digestion. The case described here indicates that patients with chronic cholestasis and hypercholesterolemia can be treated with TCM. The therapeutic effects of TCM can be further observed based on the current situation of the patient. There is presently no specific pharmacological treatment for patients with Alagille syndrome. Patients with obvious itching can be treated with Chinese medicine combined with a moisturizer.
Ileal bile acid transporter inhibitors can be used in patients with severe cholestasis to reduce the risk of early liver failure, and ameliorate itching[8,9]. We will adherence to dietary guidelines should be encouraged and liver function monitored during follow-up of patients with Alagille syndrome.
Alagille syndrome affects multiple organs. When physicians encounter a patient with abnormal liver function and severe hypercholesterolemia, the possibility of Alagille syndrome should be considered and genetic testing performed to screen for disease-causing mutations. A combination of TCM and Western medicine in addition to conventional therapy can be considered. The role of TCM in maintenance treatment of Alagille syndrome may be underestimated.
| 1. | Kamath BM, Baker A, Houwen R, Todorova L, Kerkar N. Systematic Review: The Epidemiology, Natural History, and Burden of Alagille Syndrome. J Pediatr Gastroenterol Nutr. 2018;67:148-156. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 58] [Cited by in RCA: 78] [Article Influence: 11.1] [Reference Citation Analysis (0)] |
| 2. | McDaniell R, Warthen DM, Sanchez-Lara PA, Pai A, Krantz ID, Piccoli DA, Spinner NB. NOTCH2 mutations cause Alagille syndrome, a heterogeneous disorder of the notch signaling pathway. Am J Hum Genet. 2006;79:169-173. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 582] [Cited by in RCA: 501] [Article Influence: 26.4] [Reference Citation Analysis (0)] |
| 3. | Zanotti S, Canalis E. Notch signaling in skeletal health and disease. Eur J Endocrinol. 2013;168:R95-103. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 51] [Cited by in RCA: 52] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Kohut TJ, Gilbert MA, Loomes KM. Alagille Syndrome: A Focused Review on Clinical Features, Genetics, and Treatment. Semin Liver Dis. 2021;41:525-537. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 39] [Article Influence: 9.8] [Reference Citation Analysis (1)] |
| 5. | Turnpenny PD, Ellard S. Alagille syndrome: pathogenesis, diagnosis and management. Eur J Hum Genet. 2012;20:251-257. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 233] [Cited by in RCA: 272] [Article Influence: 19.4] [Reference Citation Analysis (0)] |
| 6. | Wang N, Gu XY, Wu Y, Wu HY, Liang XY, Xiu YF. [Overview of the clinical application and pharmacological effects of chicken inner gold]. Jiangsu Zhongyiyao. 2021;53:77-81. [DOI] [Full Text] |
| 7. | Wang F, Yang CL, Jin CF, Zhu XX, Jiang H, Ye HJ. [Effect of Modified Yinchen Decoctionand Basic Western Medicine on Intrahepatic Cholestasis of Pregnancy]. Zhonghua Zhongyiyaoxuekan. 2019;37:3038-3041. [DOI] [Full Text] |
| 8. | Wu LN, Sun LY, Zhu ZJ, Wang XM, Wang Y, Ou XJ, Jia JD, Zhao XY. [Clinical and histological characteristics of petients with Alagille syndrome]. Ganzang. 2023;28:351-355. [DOI] [Full Text] |
| 9. | Menon J, Shanmugam N, Vij M, Rammohan A, Rela M. Multidisciplinary Management of Alagille Syndrome. J Multidiscip Healthc. 2022;15:353-364. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 2] [Article Influence: 0.7] [Reference Citation Analysis (0)] |