Published online May 6, 2025. doi: 10.12998/wjcc.v13.i13.101444
Revised: December 5, 2024
Accepted: December 27, 2024
Published online: May 6, 2025
Processing time: 114 Days and 22.7 Hours
Unilateral biportal endoscopic (UBE) surgery has developed rapidly during the past decade. Continuous epidural space irrigation is generally considered the principal reason for cerebral complications following UBE surgery. We present a case of mental symptoms during the general anesthesia awakening period due to pneumocephalus.
A 70-year-old woman with lumbar disc herniation underwent UBE surgery stably under general anesthesia. Uncontrollable hypertension occurred immediately after transfer to the postoperative care unit, accompanied by increased heart rate and tachypnea. During the recovery process, the patient responded to external stimuli but was confused and unable to complete command actions. Neck stiff
Cerebral complications emerging during the general anesthesia awakening period following UBE surgery are not entirely due to increased intracranial pressure. Pneumocephalus induced by dural injury may also be a potential cause.
Core Tip: Unilateral biportal endoscopic (UBE) surgery has developed rapidly during the past decade. Continuous epidural space irrigation is generally considered as the principal reason of cerebral complications following UBE surgery. We herein presented a case of mental symptoms during the general anesthesia awakening period due to pneumocephalus, accompanied by de-cerebrate rigidity. The case indicated that pneumocephalus induced by dural injury may also be a potential cause. Definitive diagnostic imaging is essential to discriminate the special condition.
- Citation: Han C, Ren ZY, Jiang ZH, Luo YF. Cerebral complications after unilateral biportal endoscopic surgery: A case report. World J Clin Cases 2025; 13(13): 101444
- URL: https://www.wjgnet.com/2307-8960/full/v13/i13/101444.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i13.101444
Unilateral biportal endoscopic (UBE) surgery is an emerging technology for the treatment of lumbar disc herniation and stenosis, which integrates endoscopy and microscopic surgery[1,2]. In contrast to conventional single portal endoscopy limited by technical difficulties and restricted field of vision, the independent visualization and working portals in UBE provide surgeons with a better surgical field and operation space[3]. A series of advantages such as minor surgical damage, earlier rehabilitation[1,2,4], as well as a shorter learning curve[5] have ensured its rapid popularity in recent years. Several recent reviews[1,6-8] have focused on procedure-related complications; however, the potential cerebral complications following UBE surgery, such as headache[3] and seizures[9,10], have attracted little attention. In two case reports, intracranial hypertension triggered by irrigation fluid overload was considered the direct reason for convulsive seizures, especially in the presence of dural injury[9,10]. Here we present a case of pneumocephalus-induced seizures following UBE surgery, which might be different to previous reports.
The 70-year-old female patient complained of left lumbocrural discomfort for 1 month, aggravated for 1 week.
The patient underwent elective UBE surgery for lumbar disc protrusions.
The patient had type 2 diabetes mellitus for 5 years which was well controlled with oral metformin. She had no prior history of psychiatric illness, psychotropic drug use, head trauma, fever, seizures, or disorientation.
The patient denied any personal or family history.
Vital signs on admission were as follows: Body temperature, 37.0 °C; blood pressure, 146/74 mmHg; pulse rate 76 bpm; and respiratory rate 18 breaths/min. Physical examination revealed tenderness in multiple intervertebral spaces in the lumbosacral region. The straight leg rise test was positive (60°) only on the left side.
No significant abnormalities were observed.
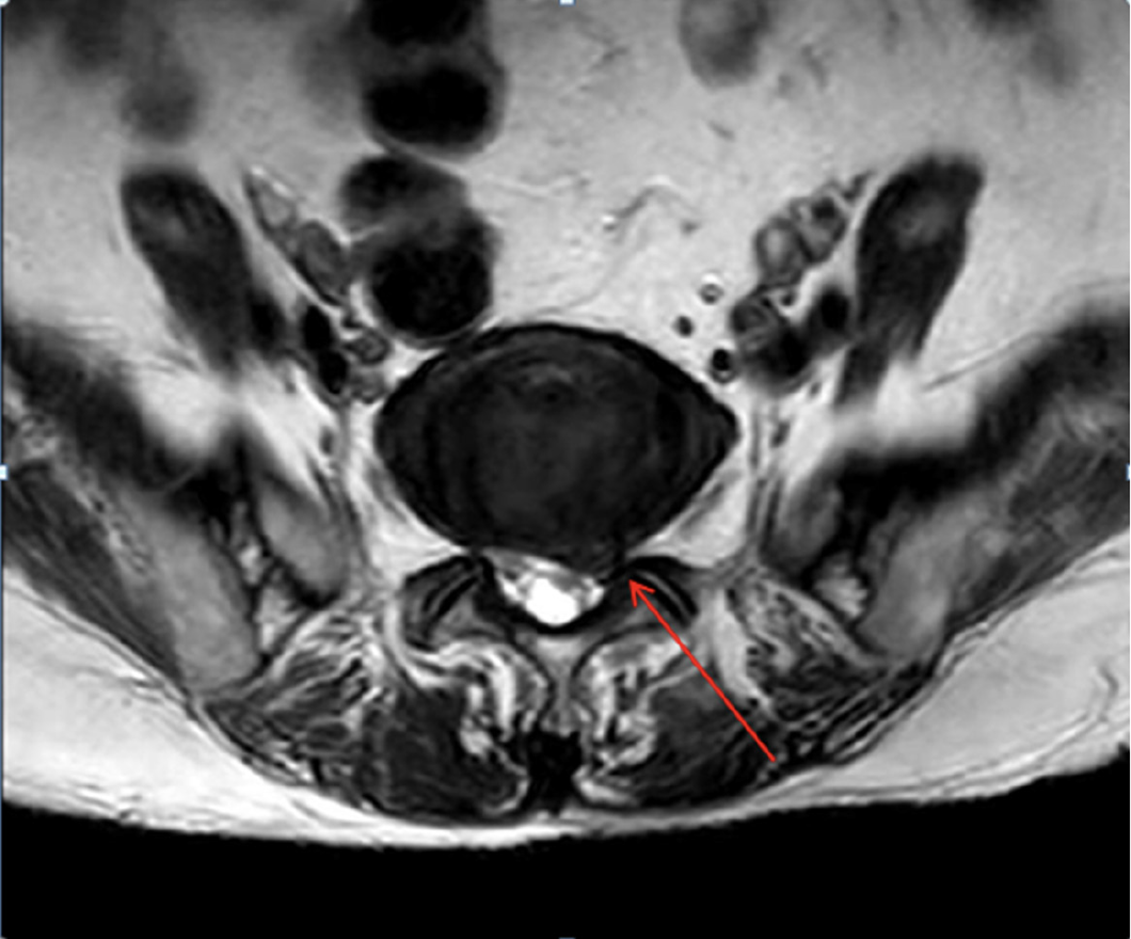
Lumbar magnetic resonance imaging (MRI) showed protruded lumbar disc (L5/S1) (Figure 1) herniation, leading to dural sac compression.
Pneumocephalus-induced seizures.
Following imaging confirmation, the patient was admitted to the ICU with ventilator supportive care. Propofol and remifentanil continuous intravenous infusion was titrated to maintain the patient under sedation.
Upon entering the operating theatre, the patient received standard monitoring including oxygen saturation, heart rate, and electrocardiogram. Right radial artery catheterization was performed to monitor arterial blood pressure. Anesthesia induction was performed by sequential intravenous administration of midazolam 3 mg, sufentanil 20 µg, etomidate 14 mg, followed by cisatracurium 12 mg to facilitate endotracheal intubation. The patient was mechanically ventilated with 100% oxygen, VT 400 mL frequency 12/min was conducted to maintain an end-tidal CO2 of 30–40 mmHg during the surgical procedure. Sufentanil 10 μg was administered before skin incision. Sevoflurane inhalation and remifentanil continuous intravenous infusion were titrated to maintain hemodynamic stability and adequate depth of anesthesia (BIS values 40–60). Another 5 μg sufentanil was given intravenously 5 minutes before suturing.
When the general anesthesia took effect, the patient was placed in the prone position with a support frame on the abdomen. An approximately 6 mm endoscope tunnel and a larger 10 mm incision for instrument operation were performed. Herniated disc fragments (L5/S1) were removed using endoscopic forceps via a fluoroscopic-guided posterolateral transforaminal approach. Dural injury was suspected soon after initiation of surgery, but was not confirmed due to the lack of direct evidence. The surgeons did not acknowledge the occurrence of intraoperative dural injury until imaging evidence was ultimately presented. The entire surgical process lasted 130 minutes, and the irrigation time was 80 minutes with continuous infusion of 5000 mL saline into the epidural space. The saline bag was set at approximately 80 cm above the operation plane.
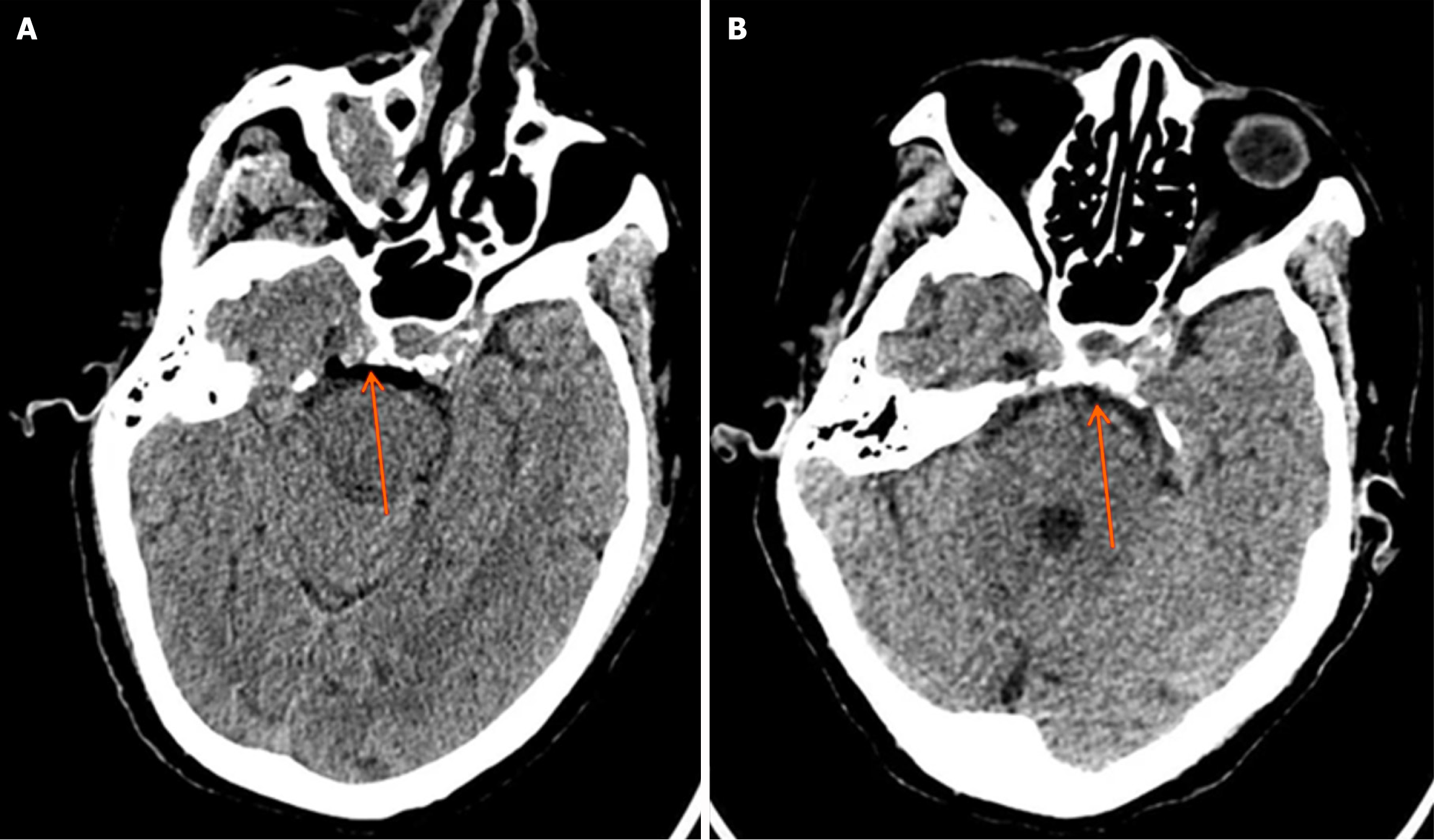
At the end of surgery, all anesthetics were discontinued, and the patient was transferred to the post-anesthesia care unit (PACU) for recovery. On arriving in the PACU, the patient's systolic blood pressure spiked to 180-200 mmHg, accompanied by an increased heart rate of 120-130 bpm. Nitroglycerin and esmolol were immediately administered to control hypertension and rapid heartbeat. Unfortunately, the effect was suboptimal. Considering the possible presence of a dural tear during the surgical procedure, we suspected resistant hypertension of a Cushing reflex triggered by intracranial hypertension. Mannitol and furosemide were then given to reduce intracranial pressure (ICP), and hydrocortisone for brain protection. Ten minutes after entering the PACU, the patient regained spontaneous breathing with a respiratory rate exceeding 30 breaths/min. She responded to external stimuli and opened her eyes involuntarily, but could not follow commands. Both pupils were of equal size and shape, but the patient exhibited neck stiffness and significantly increased muscle strength on the left side (grade 3) compared to the right side (grade 1). Propofol and remifentanil, combined with a muscle relaxant, were administered to control systolic blood pressure at 140-150 mmHg. An urgent brain computed tomography (CT) scan was performed, revealing pneumocephalus surrounding the brainstem (Figure 2).
Three hours later, her consciousness gradually returned. Extubation was performed the next morning, and the patient was subsequently transferred back to the orthopedic ward. She was discharged on the fifth postoperative day without complications. The patient was followed up for 3 months and showed no surgical or brain complications.
Cerebral complications related to UBE surgery have not been fully recognized. Previous reviews attributed postoperative nervous system manifestations after UBE surgery, such as headache, neck pain, and seizures to increased cervical epidural pressure and ICP[9,10]. However, the relationship between seizures and ICP remains controversial. The de-cerebrate rigidity and epilepsy-like episode in our case indicated that cerebral complications might be due to multiple factors, and not entirely the result of increased ICP. Therefore, it is necessary to classify cerebral symptoms after UBE surgery as independent complications for further investigation.
Early studies have reported that patients who underwent endoscopic lumbar discectomy under local anesthesia complained of neck pain, headache, blurred vision, and drowsiness[3,11]. The underlying mechanism may be explained by the irrigation fluid introduced into the spinal canal during surgery which compresses the thecal sac, thereby disrupting the cerebrospinal fluid circulation and increasing ICP and cervical epidural pressure[12]. Besides epidural compression, ICP is also gravely impacted in the presence of dural defects, through which washing fluid can enter the intrathecal space. These prodromal symptoms would generally be relieved by stopping irrigation and improving the outflow[13,14]; however, they may be obscured under general anesthesia. Persistent elevated ICP could trigger the Cushing reflex, causing systemic hypertension to maintain cerebral perfusion. Hypertension increases the risk of stroke and posterior reversible encephalopathy syndrome (PRES), both of which exhibit signs of brain network disturbance and are difficult to differentiate from emergence agitation.
With regard to the management of the present case, we initially considered a Cushing reflex when the patient’s blood pressure rapidly increased in the PACU, given the potential intraoperative dural tear. However, the acute blood pressure fluctuation differed from the slow increase in blood pressure caused by elevated ICP, and we attributed the change partly to the decreased anesthesia depth at that time. Our treatment focused on reducing ICP, controlling blood pressure and heart rate. Notably, without addressing ICP, simple blood pressure reduction could lead to insufficient cerebral perfusion, potentially causing agitation and delayed recovery. Additionally, we could not rule out anesthesia emergence as a cause of the hypertension, even though additional analgesics were administered before the end of surgery. Differential diagnosis was indeed challenging. When we observed significantly increased muscle strength on the left side, we suspected the possibility of intracranial hemorrhage, despite the symmetric and reactive pupils.
A brain CT scan ultimately confirmed the diagnosis of pneumocephalus, which perfectly explained all the patient's symptoms. During surgery, the dural tear allowed air to enter the subarachnoid space through the dural defect, which also acts as a one-way valve and traps the air. This is the so-called ball valve theory, which may explain the pneumocephalus after lumbar spine surgery[15]. When the patient was repositioned from prone to supine, the air migrated upward due to gravity, entering the fourth ventricle via the central canal, thereby compressing the medulla oblongata. The pneumocephalus in this case was confined to the brainstem area, with no gas detected in other intracranial regions, which contrasted with the usual signs of elevated ICP induced by irrigation. Medullary compression not only altered blood pressure, heart rate, and respiratory frequency but also significantly affected the corticospinal tract, leading to muscle strength changes. Furthermore, we observed that the gas pressure on the left side was stronger than that on the right side, which correlated with the clinical finding of increased muscle strength on the left side. Although CT is believed to be superior to MRI for the detection of pneumocephalus, MRI might be more useful in ruling out hypertension-induced PRES[16].
Despite its rarity, there is still the risk of pneumocephalus in minimally invasive spinal surgery[17,18]. Symptoms of pneumocephalus vary and depend on the location and amount of air inside the skull. Gader et al[17] reported a patient with frontal interhemispheric pneumocephalus who presented with 3 generalized tonic-clonic seizures six hours after awakening with recovery of consciousness between the episodes and normal biologic findings. In the study by Yang et al[18], the patient exhibited intracranial hypotension symptoms such as headache, nausea and dizziness despite air dispersed in the bilateral ventricles and sub-arachnoid space on CT scan on post-operative 3 day. Our case presented as an acute attack immediately after surgery, which was different to the above cases. Therefore, we deem this to be clinically significant.
Our case illustrated the vital role of neuroimaging in the differential diagnosis of cerebral complications during the general anesthesia recovery period. CT is capable of detecting early cerebral hemorrhage and pneumocephalus, but not PRES. In contrast, MRI can identify the characteristic subcortical and cortical hyperintensity in the bilateral occipital lobes of patients with PRES. When confronted with the clinical predicament, a brain CT scan should be the initial choice. If it is negative, further MRI examination is necessary to rule out PRES.
Our case also offered a vivid lesson to surgeons. Dural injury is the most common complication in UBE surgery. Common causes encompassed the negligent utilization of surgical tools, inexperienced operator performing surgery, the anatomy of the central dural fold, and poor surgical vision[7]. In any event, meticulous operation and intraoperative examination of dural integrity are effective approaches to prevent complications.
Cerebral complications occurring during the general anesthesia awakening period following UBE surgery are not entirely the result of increased intracranial pressure. Pneumocephalus induced by dural injury may also be a potential cause. Definitive diagnostic imaging is essential to discriminate this special condition.
| 1. | Lin GX, Huang P, Kotheeranurak V, Park CW, Heo DH, Park CK, Park JY, Kim JS. A Systematic Review of Unilateral Biportal Endoscopic Spinal Surgery: Preliminary Clinical Results and Complications. World Neurosurg. 2019;125:425-432. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 95] [Article Influence: 15.8] [Reference Citation Analysis (0)] |
| 2. | Chu PL, Wang T, Zheng JL, Xu CQ, Yan YJ, Ma QS, Meng-Chen Y, Da-Sheng T. Global and Current Research Trends of Unilateral Biportal Endoscopy/Biportal Endoscopic Spinal Surgery in the Treatment of Lumbar Degenerative Diseases: A Bibliometric and Visualization Study. Orthop Surg. 2022;14:635-643. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 72] [Article Influence: 24.0] [Reference Citation Analysis (0)] |
| 3. | Hwa Eum J, Hwa Heo D, Son SK, Park CK. Percutaneous biportal endoscopic decompression for lumbar spinal stenosis: a technical note and preliminary clinical results. J Neurosurg Spine. 2016;24:602-607. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 177] [Article Influence: 19.7] [Reference Citation Analysis (0)] |
| 4. | Zhou H, Wang X, Chen Z, Liu W, Luo J. Unilateral biportal endoscopy versus microscopic decompression in the treatment of lumbar spinal stenosis: A meta-analysis. Medicine (Baltimore). 2023;102:e32756. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 5. | Choi DJ, Choi CM, Jung JT, Lee SJ, Kim YS. Learning Curve Associated with Complications in Biportal Endoscopic Spinal Surgery: Challenges and Strategies. Asian Spine J. 2016;10:624-629. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 54] [Cited by in RCA: 117] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 6. | Ju CI, Lee SM. Complications and Management of Endoscopic Spinal Surgery. Neurospine. 2023;20:56-77. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 55] [Reference Citation Analysis (0)] |
| 7. | Li YS, Chen CM, Hsu CJ, Yao ZK. Complications of Unilateral Biportal Endoscopic Lumbar Discectomy: A Systematic Review. World Neurosurg. 2022;168:359-368.e2. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Wang B, He P, Liu X, Wu Z, Xu B. Complications of Unilateral Biportal Endoscopic Spinal Surgery for Lumbar Spinal Stenosis: A Systematic Review of the Literature and Meta-analysis of Single-arm Studies. Orthop Surg. 2023;15:3-15. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 23] [Article Influence: 7.7] [Reference Citation Analysis (0)] |
| 9. | Wu J, Fang Y, Jin W. Seizures after percutaneous endoscopic lumbar discectomy: A case report. Medicine (Baltimore). 2020;99:e22470. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 5] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 10. | Kertmen H, Gürer B, Yilmaz ER, Sekerci Z. Postoperative seizure following transforaminal percutaneous endoscopic lumbar discectomy. Asian J Neurosurg. 2016;11:450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Kim HS, Wu PH, Jang IT. Lumbar Endoscopic Unilateral Laminotomy for Bilateral Decompression Outside-In Approach: A Proctorship Guideline With 12 Steps of Effectiveness and Safety. Neurospine. 2020;17:S99-S109. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 26] [Article Influence: 5.2] [Reference Citation Analysis (0)] |
| 12. | Kang MS, Park HJ, Hwang JH, Kim JE, Choi DJ, Chung HJ. Safety Evaluation of Biportal Endoscopic Lumbar Discectomy: Assessment of Cervical Epidural Pressure During Surgery. Spine (Phila Pa 1976). 2020;45:E1349-E1356. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 24] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 13. | Kim JE, Choi DJ, Park EJJ, Lee HJ, Hwang JH, Kim MC, Oh JS. Biportal Endoscopic Spinal Surgery for Lumbar Spinal Stenosis. Asian Spine J. 2019;13:334-342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 81] [Cited by in RCA: 92] [Article Influence: 15.3] [Reference Citation Analysis (0)] |
| 14. | Choi CM. Biportal endoscopic spine surgery (BESS): considering merits and pitfalls. J Spine Surg. 2020;6:457-465. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 39] [Article Influence: 7.8] [Reference Citation Analysis (0)] |
| 15. | Abu-Hamdiyah OJ, Al Sharie S, Awadi S, Khamees A, Athamneh MJ. Pneumocephalus secondary to a spinal surgery: A literature review and a case report. Int J Surg Case Rep. 2021;86:106342. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 1.0] [Reference Citation Analysis (0)] |
| 16. | Triplett JD, Kutlubaev MA, Kermode AG, Hardy T. Posterior reversible encephalopathy syndrome (PRES): diagnosis and management. Pract Neurol. 2022;22:183-189. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 43] [Article Influence: 14.3] [Reference Citation Analysis (0)] |
| 17. | Gader G, Karmeni N, Ben Saïd I, Jemel H. Symptomatic pneumocephalus: A rare complication of discal herniation's surgery. J Spinal Cord Med. 2019;42:810-812. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Yang CT, Chiu CD, Wu CY. Diffuse symptomatic pneumocephalus after biportal endoscopic spinal surgery: illustrative case. J Neurosurg Case Lessons. 2022;3:CASE22168. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |