Published online Apr 16, 2025. doi: 10.12998/wjcc.v13.i11.98570
Revised: October 28, 2024
Accepted: December 6, 2024
Published online: April 16, 2025
Processing time: 179 Days and 0.2 Hours
Internal hernia is a rare complication following abdominal surgery, primarily resulting from structural defects caused by anastomosis. We report a unique case of a late abdominal wall internal hernia highly suspected as resulting from insu
A 72-year-old woman presented with symptoms of intestinal obstruction 40 years after undergoing an abdominal hysterectomy. Abdominal computed tomography revealed a suspicious closed loop of intestine; then, a laparotomy was performed for suspected internal hernia. During the procedure, herniation of intestine into the preperitoneal space through a parietal peritoneal defect between rectus abdominis and sigmoid colon was identified. Intestinal reduction, resection of the ischemic segment and closure of the peritoneal defect were performed. The patient recovered well.
Non-closure of peritoneum might lead to late internal hernias. Meticulous peritoneal closure should be considered to prevent this potentially lethal complication.
Core Tip: We report a unique case of an abdominal wall internal hernia, a late complication that is highly suspected to be related to insufficient peritoneal closure. In the context of the current dominant practice of not closing the peritoneum, our case highlights a potential challenge in lower abdominal surgeries, particularly those involving organ resection or transabdominal preperitoneal inguinal herniorrhaphy. It emphasizes the need for heightened awareness among clinicians regarding long-term surgical outcomes, and advocates for meticulous peritoneal closure to prevent this potentially lethal issue, despite the limited existing evidence.
- Citation: Chou YC. Parietal peritoneal hernia after abdominal hysterectomy for forty years: A case report. World J Clin Cases 2025; 13(11): 98570
- URL: https://www.wjgnet.com/2307-8960/full/v13/i11/98570.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i11.98570
Internal hernia is a rare condition related to either natural or acquired defects, which can lead to intestinal obstruction, ischemia, necrosis and even mortality. As a surgical complication, it accounts for 0.5% to 6% of various operations, primarily resulting from anastomosis[1-5]. Internal hernias occurring through abdominal wall peritoneal defects are extremely rare and have predominantly been reported as acute complications[6-8]. We describe a case of such a condition as a late complication occurring 40 years after a hysterectomy.
A 72-year-old woman complained of abdominal distension for three days.
A 72-year-old female presented to the emergency room with abdominal distension lasting for three days. She also complained about vomiting and a lack of flatus and defecation, but denied having had similar discomfort in the past.
She had undergone a hysterectomy via lower midline laparotomy 40 years previously, although no documentation regarding the operation was available.
There is no relevant personal and family history.
Physical examination revealed mild abdominal distension with stable vital signs and no signs of peritoneal irritation.
Blood tests indicated dehydration (hemoconcentration, pre-renal azotemia and hyperlactatemia) and signs of intra-abdominal infection (leukocytosis with left shift and hyperlactatemia).
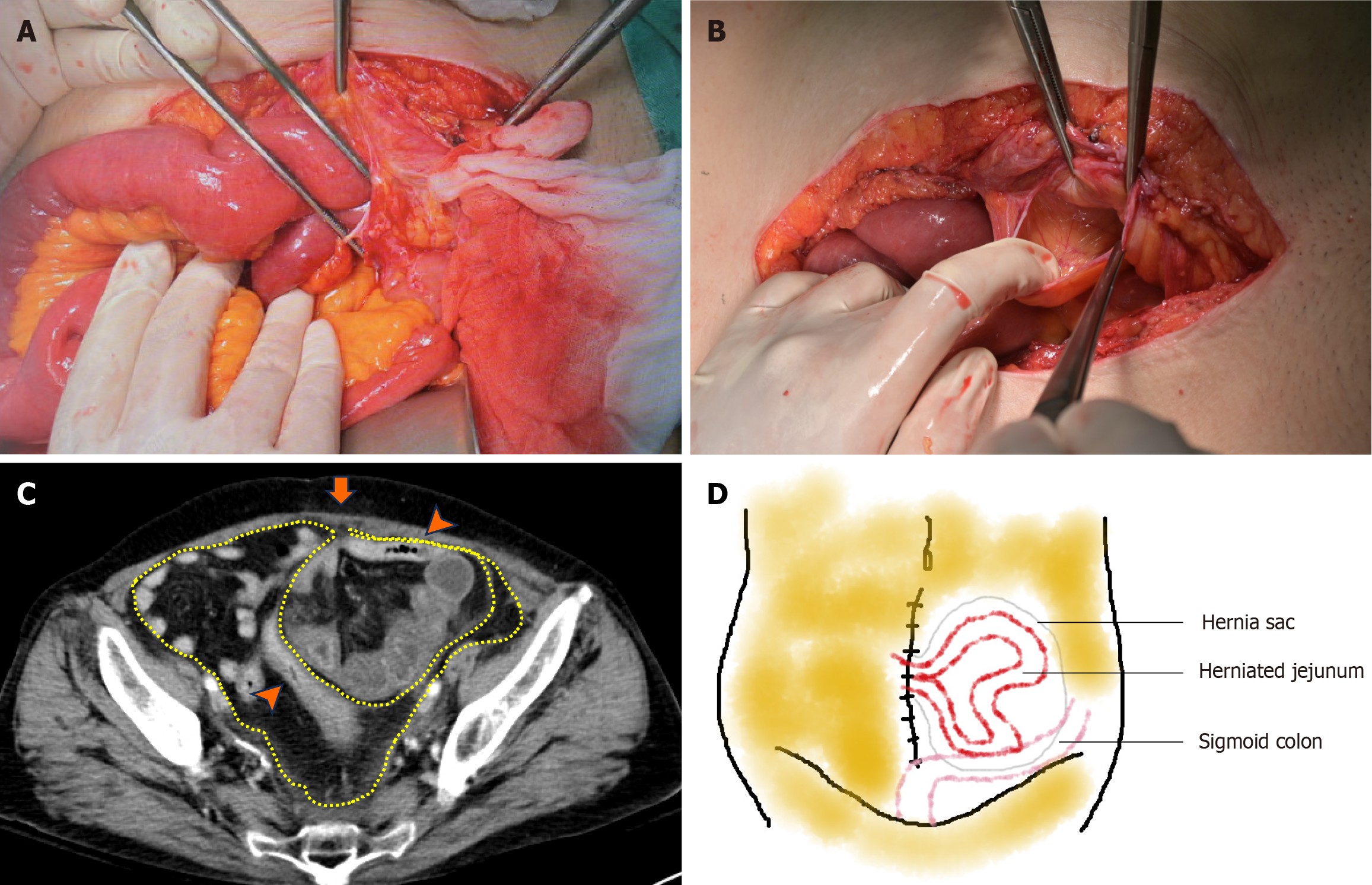
Abdominal computed tomography (CT) revealed segmental dilation of the small bowel with a transitional zone of mid-ileum in right lower quadrant, as well as a segment of suspicious closed loop of the small bowel with edematous change and focal ascites in the left lower quadrant (Figure 1).
The final diagnosis is high suspicion of internal herniation.
The CT scan indicated suspicious internal herniation. Although the patient did not exhibit signs of peritoneal irritation and her vital signs were relatively stable, clinical deterioration could have been delayed due to obstruction of venous return from internal herniation. Considering its high risk of morbidity and mortality, low likelihood of spontaneous reduction and the patient’s advanced age with limited compensatory ability, exploratory laparotomy was recommended. After a thorough explanation and discussion, the patient and her family consented to surgery.
An urgent exploratory laparotomy was performed. After incising along the previous hysterectomy scar, a large segment of distal jejunum was found herniated into the preperitoneal space in the pelvis through a peritoneal defect at the prior scar, located between the rectus abdominis and sigmoid colon. A complete hernia sac under intact muscular integrity was identified (Figure 2A and B). Upon reviewing CT, the situation was also documented (Figure 2C) in a perspective drawing illustrating the spatial relationship of the hernia in a simple way (Figure 2D). The herniated intestine was reduced, and a ten-centimeter segment of bowel resection was performed due to suspected partial wall ischemic changes. The peritoneal defect (hernia sac) was closed using continuous non-absorbable sutures.
The patient was transferred to intensive care unit for sepsis and atrial fibrillation with rapid ventricular response postoperatively. She had a smooth recovery from the sepsis, and her intake was gradually resumed with the postope
Internal hernia is a rare, surgery-related condition that can be potentially lethal, possibly resulting from congenital or postoperative defects or weak points. The incidence varies between surgical procedures and methods of anastomosis, with significantly higher rates observed in upper gastrointestinal surgeries (0.7% to 6%)[1,2,4], lower rates in lower gastrointestinal surgeries (0.5% to 0.65%)[3,5], and even lower rates in other types of surgery. Most cases are caused by ring-structured defects produced by anastomosis[1-5]. Diagnosis is challenging due to non-specific clinical symptoms and findings, with accurate diagnosis requiring a high level of awareness from physicians.
In our case, we report an extremely rare presentation of an incisional internal hernia. The exact cause of this hernia was unclear and there were no records regarding the hysterectomy, particularly concerning peritonealization. However, it was assumed that a peritoneal defect - whether peritonealized or not - was created by the prior abdominal hysterectomy, leading to chronic migration of the intestine. This is similar to the acute complication of intestinal herniation through a small peritoneal defect after abdominal hysterectomy, as proposed by Kwon et al[6]. Other similar cases in transabdominal preperitoneal (TAPP) herniorrhaphy have also demonstrated acute herniations due to improper peritoneal approximation[7,8].
Peritoneal closure remains a topic of controversy, with a trend towards non-closure in both obstetric and non-obstetric surgeries in recent decades. In the case of acute peritoneal hernia after hysterectomy mentioned above, the surgeons ultimately decided to leave the peritoneum open and only closed the fascial layer[6]. The reasons favoring non-closure included equivalent major complications - such as mortality, burst abdomen, incisional hernia, and length of hospitalization - as well as shorter surgical times and reduced anesthesia exposure[9-11]. Similar findings regarding postoperative pain and recurrence have been observed in TAPP surgeries[12]. Our case highlights the possibility of a significant late complication of internal herniation, which can lead to high morbidity. Despite the limited evidence, we propose that non-peritonealization could result in peritoneal herniation with acute onset associated with smaller defects and late onset with larger ones.
Accordingly, parietal peritoneal hernia emerges as a possibly delayed challenge in the context of current practices of non-peritonealization or large-distance closure of the peritoneum. It is anticipated that this type of hernia might occur in lower abdominal surgeries involving organ resection such as hysterectomy or cystectomy, where there is no fascial restriction and additional preperitoneal space. Inguinal hernias following TAPP repair could also represent a potential source, given the disease-related space, a relatively weak abdominal wall, and compromised peritoneal integrity due to absorbable tacks or non-closure. Given the high morbidity and mortality associated with internal hernias compared to their low primary detection rates, we advocate for more meticulous closure of the peritoneum in these situations, even in light of the limited available evidence. Further investigation is necessary.
Non-closure of the peritoneum may lead to internal hernia developing over time. This late complication may pose an increasing challenge, especially in lower abdominal surgeries; accordingly, when treating patients with a long history of lower abdominal surgery, awareness needs to be raised and meticulous peritonealization should be considered to avoid this potentially lethal problem, even in the absence of extensive evidence. Further research into the long-term outcomes of non-closure of the peritoneum is necessary.
| 1. | Geubbels N, Lijftogt N, Fiocco M, van Leersum NJ, Wouters MW, de Brauw LM. Meta-analysis of internal herniation after gastric bypass surgery. Br J Surg. 2015;102:451-460. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 94] [Cited by in RCA: 102] [Article Influence: 10.2] [Reference Citation Analysis (1)] |
| 2. | Muir D, Choi B, Clements C, Ratnasingham K, Irukulla S, Humadi S. Mesenteric Defect Closure and the Rate of Internal Hernia in Laparoscopic Roux-en-Y Gastric Bypass: A Systematic Review and Meta-analysis. Obes Surg. 2023;33:2229-2236. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 5.5] [Reference Citation Analysis (1)] |
| 3. | Portale G, Popescu GO, Parotto M, Cavallin F. Internal hernia after laparoscopic colorectal surgery: an under-reported potentially severe complication. A systematic review and meta-analysis. Surg Endosc. 2019;33:1066-1074. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 3.2] [Reference Citation Analysis (1)] |
| 4. | Apostolou KG, Lazaridis II, Kanavidis P, Triantafyllou M, Gkiala A, Alexandrou A, Ntourakis D, Delko T, Schizas D. Incidence and risk factors of symptomatic Petersen's hernias in bariatric and upper gastrointestinal surgery: a systematic review and meta-analysis. Langenbecks Arch Surg. 2023;408:49. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 4.0] [Reference Citation Analysis (1)] |
| 5. | Toh JW, Lim R, Keshava A, Rickard MJ. The risk of internal hernia or volvulus after laparoscopic colorectal surgery: a systematic review. Colorectal Dis. 2016;18:1133-1141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 43] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (1)] |
| 6. | Kwon CS, Dai J, Sauer MV. Peritoneal hernia following abdominal hysterectomy: A case report. Case Rep Womens Health. 2022;33:e00371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 7. | Agresta F, Mazzarolo G, Bedin N. Incarcerated internal hernia of the small intestine through a re-approximated peritoneum after a trans-abdominal pre-peritoneal procedure--apropos of two cases: review of the literature. Hernia. 2011;15:347-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 8. | Narayanan S, Davidov T. Peritoneal pocket hernia: A distinct cause of early postoperative small bowel obstruction and strangulation: A report of two cases following robotic herniorrhaphy. J Minim Access Surg. 2018;14:154-157. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (1)] |
| 9. | Gupta JK, Dinas K, Khan KS. To peritonealize or not to peritonealize? A randomized trial at abdominal hysterectomy. Am J Obstet Gynecol. 1998;178:796-800. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 18] [Article Influence: 0.7] [Reference Citation Analysis (1)] |
| 10. | Kucuk M, Okman TK. Non-closure of visceral peritoneum at abdominal hysterectomy. Int J Gynaecol Obstet. 2001;75:317-319. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.2] [Reference Citation Analysis (1)] |
| 11. | Gurusamy KS, Cassar Delia E, Davidson BR. Peritoneal closure versus no peritoneal closure for patients undergoing non-obstetric abdominal operations. Cochrane Database Syst Rev. 2013;2013:CD010424. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (1)] |
| 12. | Kane ED, Leduc M, Schlosser K, Parentela N, Wilson D, Romanelli JR. Comparison of peritoneal closure versus non-closure in laparoscopic trans-abdominal preperitoneal inguinal hernia repair with coated mesh. Surg Endosc. 2018;32:627-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.6] [Reference Citation Analysis (1)] |