Published online Jan 6, 2025. doi: 10.12998/wjcc.v13.i1.99884
Revised: September 19, 2024
Accepted: October 23, 2024
Published online: January 6, 2025
Processing time: 97 Days and 13 Hours
Monkeypox (Mpox), is a disease of global public health concern, as it does not affect only countries in western and central Africa.
To assess Burundi healthcare workers (HCWs)s’ level of knowledge and confidence in the diagnosis and management of Mpox.
We conducted a cross-sectional study via an online survey designed mainly from the World Health Organization course distributed among Burundi HCWs from June-July 2023. The questionnaire comprises 8 socioprofessional-related questions, 22 questions about Mpox disease knowledge, and 3 questions to assess confidence in Mpox diagnosis and management. The data were analyzed via SPSS software version 25.0. A P value < 0.05 was considered to indicate statistical significance.
The study sample comprised 471 HCWs who were mainly medical doctors (63.9%) and nurses (30.1%). None of the 22 questions concerning Mpox knowledge had at least 50% correct responses. A very low number of HCWs (17.4%) knew that Mpox has a vaccine. The confidence level to diagnose (21.20%), treat (18.00%) or prevent (23.30%) Mpox was low among HCWs. The confidence level in the diagnosis of Mpox was associated with the HCWs’ age (P value = 0.009), sex (P value < 0.001), work experience (P value = 0.002), and residence (P value < 0.001). The confidence level to treat Mpox was significantly associated with the HCWs’ age (P value = 0.050), sex (P value < 0.001), education (P value = 0.033) and occupation (P value = 0.005). The confidence level to prevent Mpox was associated with the HCWs’ education (P value < 0.001), work experience (P value = 0.002), residence (P value < 0.001) and type of work institution (P value = 0.003).
This study revealed that HCWs have the lowest level of knowledge regarding Mpox and a lack of confidence in the ability to diagnose, treat or prevent it. There is an urgent need to organize continuing medical education programs on Mpox epidemiology and preparedness for Burundi HCWs. We encourage future researchers to assess potential hesitancy toward Mpox vaccination and its associated factors.
Core Tip: On August 14, 2024, the World Health Organization director-general declared that the upsurge of Monkeypox (Mpox) cases in the Democratic Republic of Congo (DRC) and in Africa constitute a public health emergency of international concern. Burundi, which borders the DRC to the east, declared a Mpox outbreak on July 25, 2024 and had just over 500 confirmed cases of Mpox, classifying Burundi as the second most affected country in Africa after the DRC. This study revealed that Burundi healthcare workers have the lowest level of knowledge regarding Mpox and a lack of confidence in the ability to diagnose, treat or prevent Mpox.
- Citation: Ntawuyamara E, Ingabire T, Yandemye I, Ndayikeza P, Bhandari B, Liang YH. Assessing healthcare workers’ knowledge and confidence in the diagnosis, management and prevention of Monkeypox. World J Clin Cases 2025; 13(1): 99884
- URL: https://www.wjgnet.com/2307-8960/full/v13/i1/99884.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i1.99884
Monkeypox (Mpox) is a viral zoonosis with symptoms similar to those seen in the past in smallpox patients[1]. Mpox primarily occurs in central and western Africa, often in proximity to tropical rainforests, and has increasingly appeared in urban areas. Mpox was discovered in 1958 when two outbreaks of a pox-like disease occurred in group of monkeys in a lab. Despite being named “monkeypox,” the source of the disease remains unknown. The first human case of Mpox was recorded in 1970, and the first Mpox outbreak outside Africa occurred in 2003[2]. Cases were also documented in the United States of America and was linked to contact with infected pet prairie dogs[3].
Mpox was also reported in travelers from Nigeria to Israel in September 2018, to the United Kingdom in September 2018, December 2019, May 2021 and May 2022, to Singapore in May 2019, and to the United States of America in July and November 2021[4]. In China, an Mpox epidemic was declared on September 16, 2022, when an imported case was found in Chongqing Municipality[5]. In May 2022, multiple cases of Mpox were identified in several nonendemic countries. Since January 2023, the Democratic Republic of Congo (DRC) has reported more than 22000 suspected cases of Mpox and 1200 deaths[6]. On August 14, 2024, the World Health Organization (WHO) director-general declared that the increase in Mpox in the DRC and the increasing number of countries in Africa constitute a public health emergency of international concern under the International Health Regulations[7]. Burundi, which borders the DRC to the East, declared an Mpox outbreak on July 25, 2024. By September 13, 2024, Burundi had 516 Mpox confirmed cases, classifying it as the second most affected country in Africa after the DRC[8]. Mpox is a disease of global public health importance, as it affects not only countries in western and central Africa but also the rest of the world.
Burundi is located in the East African Community (EAC), a region with a tropical climate where some epidemics begin. It shares borders with DRC, Tanzania and Rwanda, which have faced many viral epidemics of Ebola, Marburg fever, coronavirus disease 2019 (COVID-19) and Mpox[9,10]. Burundi has a fragile health system and is facing an enormous burden of infectious diseases such as malaria, HIV/AIDS, tuberculosis, hepatitis B and C and the most recent strain of COVID-19. Currently, it is facing an outbreak of cholera, and poliomyelitis outbreaks were announced more than 30 years ago[11,12]. Considering the important role played by healthcare workers (HCWs) in mitigating and preventing emerging diseases and outbreaks, we aimed to evaluate the level of knowledge and confidence that physicians and nurses have in diagnosing, treating, and managing Mpox.
We conducted a cross-sectional study in which an online questionnaire was distributed to assess Mpox knowledge and confidence levels in the management of Mpox among HCWs in Burundi. An online survey with questions designed mainly from the WHO course “Mpox: Epidemiology, preparedness and response for African outbreak contexts” was conducted among Burundian HCWs from June-July 2023. The occupational categories that fit our definition of HCWs include medical doctor (MD), allied professions (laboratory, radiology technicians, physiotherapists, anesthesiologists, and pharmacists), nurses and midwives.
We used diverse authors’ professional backgrounds to guarantee a representative sample that covers different healthcare groups. The sample size (n) was calculated according to the formula[13].
n = [z2 × p × (1 - p)/e2]/[1 + (z2 × p × (1 - p)/(e2 × N))] where Z = 1.96 for a confidence level (α) of 95%, p = proportion (expressed as a decimal), N = population size, e = margin of error. Overall, we collected data from a total sample of 471 HWCs, including 301 MDs, 128 HWCs from allied professions, and 142 nurses and midwives.
A questionnaire translated into French, the official language in Burundi, was distributed online via the Kobo toolbox. The questionnaire comprises 8 socioprofessional-related items, 22 questions about Mpox disease knowledge, and 3 questions to assess confidence in Mpox management (Supplementary material). Participants were required to answer all questions to avoid item nonresponse bias. We used a random sampling method based on chain referrals that targeted mainly HCW groups online. To maximize the chance of questionnaire distribution and avoid selection bias, we started with the authors’ contacts and other online platforms, such as Facebook, Twitter, Instagram and direct messaging on WhatsApp, Gmail and Messenger. The last method helped to include a large number of older HCWs who may be not comfortable with online surveys. We analyzed the data via IBM SPSS, version 25.0. Chi-square tests and logistic regression analyses were used as appropriate. The statistical significance level was set at a P value < 0.05.
The study participants were mainly male (83.7%) and relatively young, with 72.6% being under 40 years old. They are mainly MDs (63.9%) and nurses (30.1%) working in the capital (60.9%). Many of them work in public health facilities (63.3%) (Table 1).
| Variable | Frequency | Percentage (%) | |
| Gender | Female | 77 | 16.3 |
| Male | 394 | 83.7 | |
| Age (years) | < 40 | 342 | 72.6 |
| ≥ 40 | 129 | 27.4 | |
| Experience in (years) | ≤ 5 | 165 | 35.03 |
| > 5 | 306 | 64.97 | |
| Residence | Capital | 287 | 60.9 |
| Out of capital | 184 | 39.1 | |
| Profession | Nurses and midwives | 142 | 30.1 |
| Allied professions | 28 | 5.9 | |
| Medical doctor | 301 | 63.9 | |
| Affiliation | Clinical facility | 298 | 63.3 |
| Administrative facility | 173 | 36.7 | |
| Health facility type | Public | 352 | 74.7 |
| Private | 66 | 14.0 | |
| NGO | 53 | 11.3 | |
| Education level | Secondary | 60 | 12.7 |
| Graduate | 310 | 65.8 | |
| Postgraduate | 101 | 21.4 | |
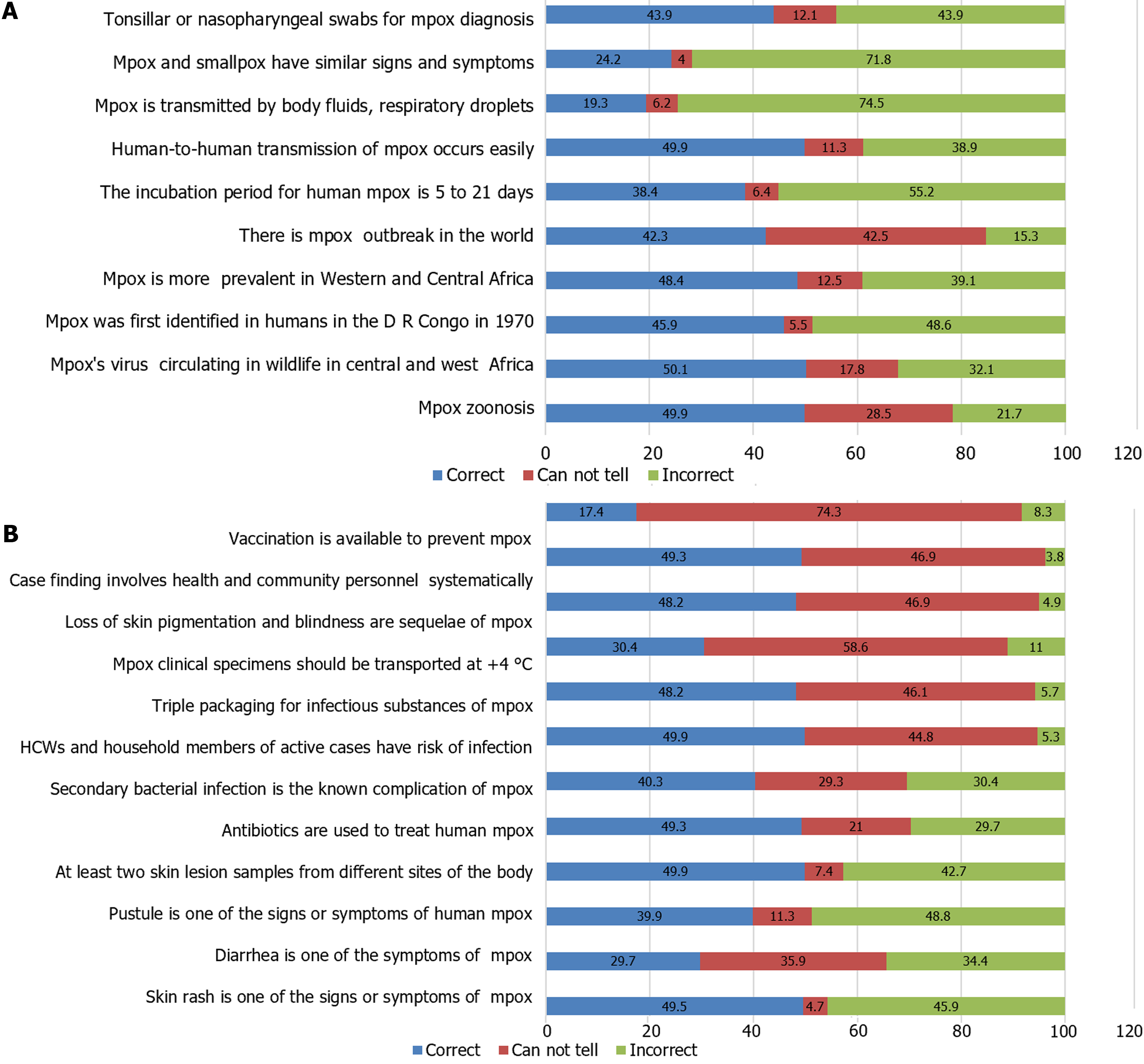
None of the 22 questions concerning Mpox knowledge had at least 50% correct responses. Some questions related to whether Mpox and smallpox have similar signs and symptoms received a high percentage of incorrect responses (71.8%). Many participants in this study were not aware of Mpox vaccination (74.3%) or of how Mpox specimens are transported after sampling (58.6%), as shown in Figure 1.
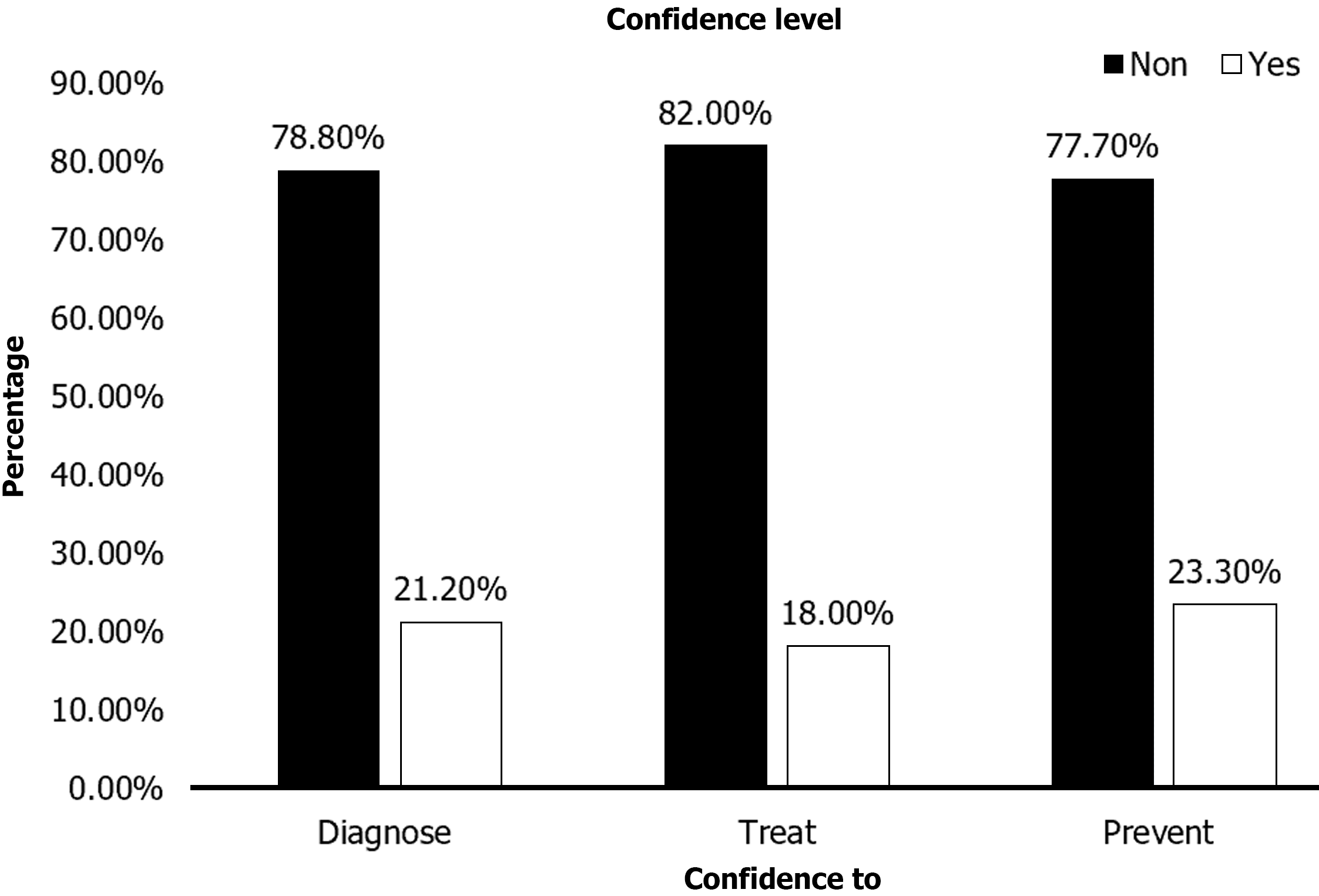
The confidence level to diagnose (21.20%), treat (18.00%) or prevent (23.30%) Mpox was low among Burundi HCWs (Figure 2).
Overall, confidence in diagnosing, treating or preventing Mpox was greater in young (< 40 years old) HCWs than in HCWs who were more than 40 years old (17.3% vs 3.6% for diagnosis, 14.6% vs 3.4% for treatment and 17.6% vs 4.7% for prevention).
As shown in Table 2, the confidence level in diagnosing Mpox was associated with the HCWs’ age (χ2 = 6.889, P value = 0.009), sex (χ2 = 12.603; P value < 0.001), work experience (χ2 = 9.381; P value = 0.002), and residence (χ2 = 13.766; P value < 0.001). The confidence level in managing Mpox was significantly associated with the HCWs’ age (χ2 = 3.826; P = 0.050), sex (χ2 = 18.025; P value < 0.001), education (χ2 = 6.833; P value = 0.033) and occupation (χ2 = 10.723; P value = 0.005). The confidence level in preventing Mpox was significantly associated with the HCWs’ education (χ2 = 18.396; P value < 0.001), work experience (χ2 = 9.406; P value = 0.002), residence (χ2 = 14.913; P value < 0.001) and type of work institution (χ2 = 11.889; P value = 0.003).
| Variables | Confidence to diagnose | Confidence to treat | Confidence to prevent | ||||
| No n (%) | Yes n (%) | No n (%) | Yes n (%) | No n (%) | Yes n (%) | ||
| Age | < 40 | 259 (55.0) | 83 (17.3) | 273 (58.0) | 69 (14.6) | 259 (55.0) | 83 (17.6) |
| ≥ 40 | 112 (23.8) | 17 (3.6) | 113 (24.0) | 16 (3.4) | 107 (22.7) | 22 (4.7) | |
| χ2 = 6.889; aP = 0.009 | χ2 = 3.826; aP = 0.050 | χ2 = 2.815; P = 0.093 | |||||
| Education | Secondary | 50 (10.5) | 10 (2.1) | 42 (8.9) | 18 (3.8) | 52 (11.0) | 8 (1.7) |
| Graduate | 239 (50.7) | 71 (15.1) | 258 (54.8) | 52 (11) | 251 (53.3) | 59 (12.5) | |
| Postgraduate | 82 (17.4) | 19 (4.0) | 86 (22.3) | 15 (17.6) | 63 (17.2) | 38 (21.4) | |
| χ2 = 1.619; P = 0.445 | χ2 = 6.833; aP = 0.033 | χ2 = 18.396; aP < 0.001 | |||||
| Occupation | Nurse | 114 (24.2) | 28 (5.9) | 110 (23.4) | 32 (6.8) | 115 (24.4) | 27 (5.7) |
| AS | 17 (3.6) | 11 (23.0) | 18 (3.8) | 10 (2.1) | 18 (3.8) | 10 (2.1) | |
| MD | 240 (51.0) | 61 (13.0) | 258 (54.8) | 43 (9.1) | 233 (49.5) | 68 (14.4) | |
| χ2 = 5.820; P = 0.054 | χ2 = 10.723; aP = 0.005 | χ2 = 3.108; P = 0.149 | |||||
| Experience | ≤ 5 years | 117 (24.8) | 48 (10.2) | 135 (28.7) | 30 (6.4) | 115 (24.4) | 50 (10.6) |
| > 5 years | 254 (53.9) | 52 (11.0) | 251 (53.3) | 55 (11.7) | 251 (53.3) | 55 (11.7) | |
| χ2 = 9.381; aP = 0.002 | χ2 = 0.003; P = 0.955 | χ2 = 9.406; aP = 0.002 | |||||
| Gender | Female | 49 (10.4) | 28 (5.9) | 50 (10.6) | 27 (5.7) | 61 (13.0) | 16 (3.4) |
| Male | 322 (68.4) | 72 (15.3) | 336 (71.3) | 58 (12.3) | 305 (64.8) | 89 (18.9) | |
| χ2 = 12.603; aP < 0.001 | χ2 = 18.025; aP < 0.001 | χ2 = 0.122; P = 0.727 | |||||
| Residence | Capital | 210 (44.6) | 77 (16.3) | 230 (48.8) | 57 (12.1) | 206 (43.7) | 81 (17.2) |
| Out capital | 161 (34.2) | 23 (4.9) | 156 (33.1) | 28 (5.9) | 160 (34.0) | 24 (5.1) | |
| χ2 = 13.766; aP < 0.001 | χ2 = 1.634; P = 0.201 | χ2 = 14.913; aP < 0.001 | |||||
| Affiliation | Clinical facility | 237 (50.3) | 61 (13.0) | 240 (51.0) | 58 (12.3) | 233 (49.5) | 65 (13.8) |
| Administrative | 134 (28.5) | 39 (8.3) | 146 (31.0) | 27 (5.7) | 133 (28.2) | 40 (8.5) | |
| χ2 = 0.281; P = 0.596 | χ2 = 1.100; P = 0.294 | χ2 = 0.108; P = 0.742 | |||||
| Institution | Public | 283 (60.1) | 69 (14.6) | 286 (60.7) | 66 (14.0) | 260 (55.2) | 92 (19.5) |
| Private | 48 (10.2) | 18 (3.8) | 54 (11.5) | 12 (2.5) | 59 (12.5) | 7 (1.5) | |
| ONGs | 40 (8.5) | 13 (2.8) | 46 (9.8) | 7 (1.5) | 47 (10.0) | 6 (1.3) | |
| χ2 = 2.343; P = 0.310 | χ2 = 0.958; P = 0.619 | χ2 = 11.889; aP = 0.003 | |||||
| Total | 371 | 100 | 386 | 85 | 366 | 105 | |
All factors that were correlated with confidence in diagnosing, treating or preventing Mpox (P value < 0.05) were included in the binary logistic regression analysis model as explanatory variables, with their corresponding P values, odds ratios and 95% confidence intervals. The confidence in diagnosing Mpox in males was significantly greater than that in females (P = 0.001, OR = 0.350), almost two times greater in AS than in MD (P value = 0.040, OR = 2.827) and two times greater in HCWs from the capital than in those from out of the capital (P value = 0.003, OR = 2.337). The confidence level in treating Mpox was significantly greater in male HCWs than in female HCWs (P value = 0.001, OR = 0.328) and almost three times greater in MD HCWs than in other HCWs (P value = 0.028, OR = 3.118). Additionally, confidence in preventing Mpox was significantly greater in HCWs with postgraduate education levels than in those with other education levels (P value = 0.032, OR = 3.556), in HCWs working in the capital than in those working outside the capital (P value = 0.001, OR = 2.611), in HCWs with more than 5 years of work experience than in those with no more than 5 years of experience (P value = 0.012, OR = 0.514), and in HCWs working in public health institutions than in those working in private or nongovernment health institutions (P value = 0.017, OR = 0.300) (Table 3).
| Independent Variables | Dependent variables | ||||||||
| Confidence to diagnose | Confidence to treat | Confidence to prevent | |||||||
| P | OR | CI | P | OR | CI | P | OR | CI | |
| Age | 0.149 | 0.637 | 0.345-0.176 | 0.275 | 0.703 | 0.374-1.323 | 0.425 | 0.787 | 0.436-1.419 |
| Gender | a0.001 | 0.350 | 0.186-0.660 | a0.001 | 0.328 | 0.173-0.621 | 0.935 | 0.971 | 0.480-1.963 |
| Education | 0.743 | 1.179 | 0.440-3.158 | 0.789 | 0.855 | 0.271-2.701 | a0.032 | 3.556 | 1.118-11.313 |
| Occupation | a0.040 | 2.827 | 1.046-7.39 | a0.028 | 3.118 | 0.128-8.615 | 0.165 | 0.632 | 0.331-1.208 |
| Residence | a0.003 | 2.337 | 1.335-4.090 | 0.102 | 1.624 | 0.909-2.904 | a0.001 | 2.611 | 1.481-4.605 |
| Experience | 0.117 | 0.660 | 0.393-1.109 | 0.768 | 1.090 | 0.614-1.937 | a0.012 | 0.514 | 0.305-0.864 |
| Affiliation | 0.979 | 1.008 | 0.557-1.826 | 0.672 | 0.871 | 0.459-1.652 | 0.799 | 1.075 | 0.617-1.873 |
| Institution | 0.525 | 1.298 | 0.582-2.896 | 0.608 | 0.778 | 0.299-2.026 | a0.017 | 0.300 | 0.112-0.805 |
A deep cause analysis of factors that independently influence confidence levels in diagnosing, treating, and preventing Mpox among Burundi HCWs revealed that sex was a significant factor for confidence in both diagnosing and treating Mpox, with males having higher confidence level. Residence in the capital was a strong predictor of confidence in both diagnosing and preventing Mpox. Education level plays a critical role in HCWs’ confidence in preventing Mpox, particularly for those with postgraduate education. Experience and type of institution were important for having confidence in preventing Mpox, with more experienced HCWs and those in public health institutions showing higher confidence levels.
Since 2005, thousands of suspected cases of Mpox have been reported in the DRC every year. Before the 2022 outbreak, Mpox was reported in people in several central and western African countries. Previously, almost all Mpox cases in people outside Africa were linked to international travel to countries where the disease commonly occurs or through imported animals. These cases occurred on multiple continents[14]. From January 1, 2022 through November 30, 2023, a cumulative total of 92783 Laboratory-confirmed cases of Mpox, including 171 deaths, were reported to the WHO from 116 countries/territories/areas in all six WHO regions. The DRC is a country in East Africa Community that shares borders with Burundi. A high level of transmission occurs in the country, as reflected by the high number of suspected (clinically compatible) cases reported[15].
Considering the crucial role played by HCWs in the prevention and management of emerging infectious diseases, this study aimed to assess Burundi HCWs’ knowledge of and confidence in diagnosing, treating, and preventing Mpox. It also aimed to understand conspiracy beliefs about emerging viral diseases among Burundi HCWs. The sample included 471 HCWs who were mainly male (83.7%) and relatively young, 72.6% of whom were under 40 years old. Many of them were MDs (63.9%) and nurses (30.1%) working in the capital (60.9%) or public health facilities (63.3%).
To assess the level of knowledge about Mpox, we chose 22 knowledge questions about Mpox epidemiology, diagnosis, treatment and prevention from the WHO course on Mpox[16]. None of the 22 questions concerning Mpox knowledge had at least 50% correct responses. Some questions related to whether Mpox and smallpox have similar signs and symptoms received a high percentage of incorrect responses (71.8%). Many participants (74.3%) in this study were not aware of Mpox vaccination or of how Mpox specimens are transported after sampling (58.6%). A similar result was reported by Riccò et al[17] in Italy and Sahin et al[18] in Turkey, stating that knowledge status was quite unsatisfactory, with substantial knowledge gaps in all aspects of Mpox. Our results are revealed even more substantial knowledge gaps compared to the results reported in the Middle East, where four out of 11 Mpox knowledge questions had more than 70% correct responses and 33.3% of the study respondents knew that vaccination is available to prevent Mpox, and those of Dong et al[19] in China, where 53.9% of participants were categorized as having greater knowledge of Mpox. However, the knowledge level in our study was greater than that in the study conducted by Harapan et al[20] in Indonesia, where only 10% of the study respondents had good knowledge of Mpox use. This difference in knowledge level may be because our study was conducted during the Mpox outbreak, which is not the case for the above-cited study. In addition, a very low number of HCWs (17.3%) knew that Mpox had a vaccine. For the prevention of smallpox and Mpox disease in adults 18 years of age and older, who are at high risk for smallpox or Mpox infection, JYNNEOS is an Food and Drug Administration-approved vaccine[21,22]. These findings suggest that the JYNNECOS vaccine is effective in preventing Mpox disease and that two doses provide better protection[23].
The confidence level to diagnose, treat or prevent Mpox was generally low among our study participants (21.20%, 18.00%, and 23.30%, respectively). In contrast, it is more common in young HCWs (17.3% vs 3.6% for diagnosis, 14.6% vs 3.4% for treatment and 17.6% vs 4.7% for prevention), although they were born and have lived in the postsmallpox eradication era, with a declining focus on poxviruses in education and training[17,20,24,25]. A low confidence level was also observed in Indonesia by Harapan et al[20]. Only a small percentage (10.1%) of general practitioners had good confidence in the ability to diagnose and treat Mpox in a clinical setting[20]. Confidence level in diagnosing Mpox was associated with the HCWs’ age (χ2 = 6.889, P value = 0.009), sex (χ2 = 12.603; P value < 0.001), work experience (χ2 = 9.381; P value = 0.002), and residence (χ2 = 13.766; P < 0.001). The confidence level in managing Mpox was significantly associated with the HCWs’ age (χ2 = 3.826; P value = 0.050), sex (χ2 = 18.025; P value < 0.001), education (χ2 = 6.833; P value = 0.033) and occupation (χ2 = 10.723; P value = 0.005). The confidence level in preventing Mpox was significantly associated with the HCWs’ education (χ2 = 18.396; P value < 0.001), work experience (χ2 = 9.406; P value = 0.002), residence (χ2 = 14.913; P value < 0.001) and type of work institution (χ2 = 11.889; P value = 0.003). In the studies performed by Sallam et al[26] in Jordan and Harapan et al[20] in Indonesia, low confidence levels in the diagnosis and management of Mpox were attributed to the relatively young age of HCWs, with subsequent lower confidence in medical practice.
We further conducted a logistic regression analysis model of factors associated with confidence level to diagnose, treat and prevent Mpox. Our results revealed that confidence in the ability to diagnose and treat Mpox was significantly greater in males than in females. The confidence level in diagnosing and preventing Mpox was significantly greater in HCWs working in capital than in those working out in capital. This may be due not only to differences in access to medical information but also to the fact that the capital, Bujumbura, directly shares borders with RDCs where Mpox began and faced many Mpox outbreaks[17,27,28]. The confidence in diagnosing Mpox is almost two times greater in medical allied sciences professionals than in MD professionals and nurses (P value = 0.040, OR = 2.827). This is because HCW workers are included in this category and most of them are laboratory technologists who may possess more information on disease laboratory diagnosis, including Mpox. The confidence level for treating Mpox was almost three times greater in the MD than in the other HCWs (P value = 0.028, OR = 3.118). This is related to their occupation, as in the Burundi health system, decisions to treat and treatment protocols are made by the MD. Additionally, the confidence level for preventing Mpox was significantly greater in HCWs with a postgraduate education level than in those with other education levels (P value = 0.032, OR = 3.556), in HCWs working in the capital than in those working outside capital (P value = 0.001, OR = 2.611), in HCWs with more than 5 years of work experience than in those with no more than 5 years of experience (P value = 0.012, OR = 0.514), and in HCWs working in public health institutions than in private or nongovernment health institutions (P value = 0.017, OR = 0.300). This is due to more opportunities to participate in seminars or continuing medical education (CME) that involve HCWs in public health facilities. These seminars are funded by the government itself via the Ministry of Health or its partners, such as the WHO and Family Health International (FHI 360)[27,28]. A previous study has shown that attending conferences and receiving data during CME helps with better confidence acquisition[20,29].
Most positive Mpox cases during the 2022/2023 outbreak were identified among gay, bisexual, and other men who have sex with men (GBMSM)[30]. Our study did not analyze conspiracy beliefs among HCWs about GBMSM. This phenomenon should be evaluated further, especially in the EAC region, where it has been shown that stigma for the GBMSM community can have a negative impact on the management of other emerging viral diseases, such as HIV/AIDS and COVID-19[31-33]. Hesitancy toward the COVID-19 vaccine was observed in Burundi, as in other African countries, whereas the Chinese population has demonstrated a willingness to receive the Mpox vaccine[34]. This study evaluated Burundi HCWs’ level of knowledge and confidence in the diagnosis and management of Mpox, which are considerations of subjective perception. We encourage further studies to assess potential hesitancy toward Mpox vaccination and its associated factors as well as objective analysis of the diagnostic and management capacity of Mpox, such as institutional setup, staffing, medical conditions, emergency response, or the fragility of the health system.
To the best of our knowledge, this study was conducted in a region that has faced many deadly epidemics of viral diseases, such as Ebola, Marburg, HIV, and COVID-19. The results revealed a low level of knowledge and confidence in the ability to diagnose, treat and prevent Mpox. It will then constitute a first scientific database for researchers, health system partners, and policymakers to prepare EAC and the international community to mitigate an eventual Mpox epidemic. Finally, we encourage future studies to assess potential causes of stigma to populations at high risk of emerging infectious diseases and hesitancy toward Mpox vaccination and its associated factors.
| 1. | van Nispen C, Reffett T, Long B, Gottlieb M, Frawley TC. Diagnosis and Management of Monkeypox: A Review for the Emergency Clinician. Ann Emerg Med. 2023;81:20-30. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 14] [Reference Citation Analysis (0)] |
| 2. | Kuppalli K, Dunning J, Damon I, Mukadi-Bamuleka D, Mbala P, Ogoina D. The worsening mpox outbreak in Africa: a call to action. Lancet Infect Dis. 2024;. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 3. | Reed KD, Melski JW, Graham MB, Regnery RL, Sotir MJ, Wegner MV, Kazmierczak JJ, Stratman EJ, Li Y, Fairley JA, Swain GR, Olson VA, Sargent EK, Kehl SC, Frace MA, Kline R, Foldy SL, Davis JP, Damon IK. The detection of monkeypox in humans in the Western Hemisphere. N Engl J Med. 2004;350:342-350. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 706] [Cited by in RCA: 677] [Article Influence: 32.2] [Reference Citation Analysis (0)] |
| 4. | Soheili M, Nasseri S, Afraie M, Khateri S, Moradi Y, Mahdavi Mortazavi SM, Gilzad-Kohan H. Monkeypox: Virology, Pathophysiology, Clinical Characteristics, Epidemiology, Vaccines, Diagnosis, and Treatments. J Pharm Pharm Sci. 2022;25:297-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 38] [Reference Citation Analysis (0)] |
| 5. | Zhao H, Wang W, Zhao L, Ye S, Song J, Lu R, Zong H, Wu C, Huang W, Huang B, Deng Y, A R, Xie W, Qi L, Xu W, Ling H, Tan W. The First Imported Case of Monkeypox in the Mainland of China - Chongqing Municipality, China, September 16, 2022. China CDC Wkly. 2022;4:853-854. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 37] [Reference Citation Analysis (0)] |
| 6. | Mbala-Kingebeni P, Rimoin AW, Kacita C, Liesenborghs L, Nachega JB, Kindrachuk J. The time is now (again) for mpox containment and elimination in Democratic Republic of the Congo. PLOS Glob Public Health. 2024;4:e0003171. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 7. | Parums DV. Editorial: Reasons for Increasing Global Concerns for the Spread of Mpox. Med Sci Monit. 2024;30:e946343. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 8. | Gehre F, Nzeyimana E, Lagu HI, Achol E, Nguinkal JA, Kezakarayagwa E, Ihorimbere T, Nzoyikorera N, Kabatesi F, Uwineza MN, Roba A, Ndia MN, Kiiru JN, Nykwec GA, Chot Moun IG, Aguer MA, Maror JA, Dumo GW, Losuba M, Deng LL, Omari N, Ochido G, Melo AM, Mtesigwa Mkama PB, Mgimba E, Francis MF, Mapunda LA, Magesa A, Moremi N, Pimundu G, Muyigi T, Nabadda SN, Kabalisa E, Mukagatare I, Mukadi-Bamuleka D, Kamangu EN, May J, Affara M. Rapid regional mobile laboratory response and genomic monkeypox virus (MPXV) surveillance in seven East African Community partner states, August 2024: preparedness activities for the ongoing outbreak. Euro Surveill. 2024;29. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 9. | Petersen BW, Kabamba J, McCollum AM, Lushima RS, Wemakoy EO, Muyembe Tamfum JJ, Nguete B, Hughes CM, Monroe BP, Reynolds MG. Vaccinating against monkeypox in the Democratic Republic of the Congo. Antiviral Res. 2019;162:171-177. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 110] [Cited by in RCA: 116] [Article Influence: 19.3] [Reference Citation Analysis (0)] |
| 10. | Carter SE, Ahuka-Mundeke S, Pfaffmann Zambruni J, Navarro Colorado C, van Kleef E, Lissouba P, Meakin S, le Polain de Waroux O, Jombart T, Mossoko M, Bulemfu Nkakirande D, Esmail M, Earle-Richardson G, Degail MA, Umutoni C, Anoko JN, Gobat N. How to improve outbreak response: a case study of integrated outbreak analytics from Ebola in Eastern Democratic Republic of the Congo. BMJ Glob Health. 2021;6. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 11. | Hounmanou YMG, Njamkepo E, Rauzier J, Gallandat K, Jeandron A, Kamwiziku G, Porten K, Luquero F, Abedi AA, Rumedeka BB, Miwanda B, Michael M, Okitayemba PW, Saidi JM, Piarroux R, Weill FX, Dalsgaard A, Quilici ML. Genomic Microevolution of Vibrio cholerae O1, Lake Tanganyika Basin, Africa. Emerg Infect Dis. 2023;29:149-153. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 12. | Tegally H, San JE, Cotten M, Moir M, Tegomoh B, Mboowa G, Martin DP, Baxter C, Lambisia AW, Diallo A, Amoako DG, Diagne MM, Sisay A, Zekri AN, Gueye AS, Sangare AK, Ouedraogo AS, Sow A, Musa AO, Sesay AK, Abias AG, Elzagheid AI, Lagare A, Kemi AS, Abar AE, Johnson AA, Fowotade A, Oluwapelumi AO, Amuri AA, Juru A, Kandeil A, Mostafa A, Rebai A, Sayed A, Kazeem A, Balde A, Christoffels A, Trotter AJ, Campbell A, Keita AK, Kone A, Bouzid A, Souissi A, Agweyu A, Naguib A, Gutierrez AV, Nkeshimana A, Page AJ, Yadouleton A, Vinze A, Happi AN, Chouikha A, Iranzadeh A, Maharaj A, Batchi-Bouyou AL, Ismail A, Sylverken AA, Goba A, Femi A, Sijuwola AE, Marycelin B, Salako BL, Oderinde BS, Bolajoko B, Diarra B, Herring BL, Tsofa B, Lekana-Douki B, Mvula B, Njanpop-Lafourcade BM, Marondera BT, Khaireh BA, Kouriba B, Adu B, Pool B, McInnis B, Brook C, Williamson C, Nduwimana C, Anscombe C, Pratt CB, Scheepers C, Akoua-Koffi CG, Agoti CN, Mapanguy CM, Loucoubar C, Onwuamah CK, Ihekweazu C, Malaka CN, Peyrefitte C, Grace C, Omoruyi CE, Rafaï CD, Morang'a CM, Erameh C, Lule DB, Bridges DJ, Mukadi-Bamuleka D, Park D, Rasmussen DA, Baker D, Nokes DJ, Ssemwanga D, Tshiabuila D, Amuzu DSY, Goedhals D, Grant DS, Omuoyo DO, Maruapula D, Wanjohi DW, Foster-Nyarko E, Lusamaki EK, Simulundu E, Ong'era EM, Ngabana EN, Abworo EO, Otieno E, Shumba E, Barasa E, Ahmed EB, Ahmed EA, Lokilo E, Mukantwari E, Philomena E, Belarbi E, Simon-Loriere E, Anoh EA, Manuel E, Leendertz F, Taweh FM, Wasfi F, Abdelmoula F, Takawira FT, Derrar F, Ajogbasile FV, Treurnicht F, Onikepe F, Ntoumi F, Muyembe FM, Ragomzingba FEZ, Dratibi FA, Iyanu FA, Mbunsu GK, Thilliez G, Kay GL, Akpede GO, van Zyl GU, Awandare GA, Kpeli GS, Schubert G, Maphalala GP, Ranaivoson HC, Omunakwe HE, Onywera H, Abe H, Karray H, Nansumba H, Triki H, Kadjo HAA, Elgahzaly H, Gumbo H, Mathieu H, Kavunga-Membo H, Smeti I, Olawoye IB, Adetifa IMO, Odia I, Ben Boubaker IB, Muhammad IA, Ssewanyana I, Wurie I, Konstantinus IS, Halatoko JWA, Ayei J, Sonoo J, Makangara JC, Tamfum JM, Heraud JM, Shaffer JG, Giandhari J, Musyoki J, Nkurunziza J, Uwanibe JN, Bhiman JN, Yasuda J, Morais J, Kiconco J, Sandi JD, Huddleston J, Odoom JK, Morobe JM, Gyapong JO, Kayiwa JT, Okolie JC, Xavier JS, Gyamfi J, Wamala JF, Bonney JHK, Nyandwi J, Everatt J, Nakaseegu J, Ngoi JM, Namulondo J, Oguzie JU, Andeko JC, Lutwama JJ, Mogga JJH, O'Grady J, Siddle KJ, Victoir K, Adeyemi KT, Tumedi KA, Carvalho KS, Mohammed KS, Dellagi K, Musonda KG, Duedu KO, Fki-Berrajah L, Singh L, Kepler LM, Biscornet L, de Oliveira Martins L, Chabuka L, Olubayo L, Ojok LD, Deng LL, Ochola-Oyier LI, Tyers L, Mine M, Ramuth M, Mastouri M, ElHefnawi M, Mbanne M, Matsheka MI, Kebabonye M, Diop M, Momoh M, Lima Mendonça MDL, Venter M, Paye MF, Faye M, Nyaga MM, Mareka M, Damaris MM, Mburu MW, Mpina MG, Owusu M, Wiley MR, Tatfeng MY, Ayekaba MO, Abouelhoda M, Beloufa MA, Seadawy MG, Khalifa MK, Matobo MM, Kane M, Salou M, Mbulawa MB, Mwenda M, Allam M, Phan MVT, Abid N, Rujeni N, Abuzaid N, Ismael N, Elguindy N, Top NM, Dia N, Mabunda N, Hsiao NY, Silochi NB, Francisco NM, Saasa N, Bbosa N, Murunga N, Gumede N, Wolter N, Sitharam N, Ndodo N, Ajayi NA, Tordo N, Mbhele N, Razanajatovo NH, Iguosadolo N, Mba N, Kingsley OC, Sylvanus O, Femi O, Adewumi OM, Testimony O, Ogunsanya OA, Fakayode O, Ogah OE, Oludayo OE, Faye O, Smith-Lawrence P, Ondoa P, Combe P, Nabisubi P, Semanda P, Oluniyi PE, Arnaldo P, Quashie PK, Okokhere PO, Bejon P, Dussart P, Bester PA, Mbala PK, Kaleebu P, Abechi P, El-Shesheny R, Joseph R, Aziz RK, Essomba RG, Ayivor-Djanie R, Njouom R, Phillips RO, Gorman R, Kingsley RA, Neto Rodrigues RMDESA, Audu RA, Carr RAA, Gargouri S, Masmoudi S, Bootsma S, Sankhe S, Mohamed SI, Femi S, Mhalla S, Hosch S, Kassim SK, Metha S, Trabelsi S, Agwa SH, Mwangi SW, Doumbia S, Makiala-Mandanda S, Aryeetey S, Ahmed SS, Ahmed SM, Elhamoumi S, Moyo S, Lutucuta S, Gaseitsiwe S, Jalloh S, Andriamandimby SF, Oguntope S, Grayo S, Lekana-Douki S, Prosolek S, Ouangraoua S, van Wyk S, Schaffner SF, Kanyerezi S, Ahuka-Mundeke S, Rudder S, Pillay S, Nabadda S, Behillil S, Budiaki SL, van der Werf S, Mashe T, Mohale T, Le-Viet T, Velavan TP, Schindler T, Maponga TG, Bedford T, Anyaneji UJ, Chinedu U, Ramphal U, George UE, Enouf V, Nene V, Gorova V, Roshdy WH, Karim WA, Ampofo WK, Preiser W, Choga WT, Ahmed YA, Ramphal Y, Bediako Y, Naidoo Y, Butera Y, de Laurent ZR; Africa Pathogen Genomics Initiative (Africa PGI)‡, Ouma AEO, von Gottberg A, Githinji G, Moeti M, Tomori O, Sabeti PC, Sall AA, Oyola SO, Tebeje YK, Tessema SK, de Oliveira T, Happi C, Lessells R, Nkengasong J, Wilkinson E. The evolving SARS-CoV-2 epidemic in Africa: Insights from rapidly expanding genomic surveillance. Science. 2022;378:eabq5358. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 39] [Cited by in RCA: 89] [Article Influence: 29.7] [Reference Citation Analysis (0)] |
| 13. | Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol Bed Bench. 2013;6:14-17. [PubMed] |
| 14. | Su S, Zou HC, Qiao HM. [Research progress of monkeypox epidemic in multiple countries]. Zhonghua Jie He He Hu Xi Za Zhi. 2022;45:1135-1140. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 15. | McQuiston JH, Luce R, Kazadi DM, Bwangandu CN, Mbala-Kingebeni P, Anderson M, Prasher JM, Williams IT, Phan A, Shelus V, Bratcher A, Soke GN, Fonjungo PN, Kabamba J, McCollum AM, Perry R, Rao AK, Doty J, Christensen B, Fuller JA, Baird N, Chaitram J, Brown CK, Kirby AE, Fitter D, Folster JM, Dualeh M, Hartman R, Bart SM, Hughes CM, Nakazawa Y, Sims E; CDC 2024 Clade I Mpox Response Team, Christie A, Hutson CL. U.S. Preparedness and Response to Increasing Clade I Mpox Cases in the Democratic Republic of the Congo - United States, 2024. MMWR Morb Mortal Wkly Rep. 2024;73:435-440. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 26] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 16. | Selvaraj N, Shyam S, Dhurairaj P, Thiruselvan K, Thiruselvan A, Kancherla Y, Kandamaran P. Mpox: epidemiology, clinical manifestations and recent developments in treatment and prevention. Expert Rev Anti Infect Ther. 2023;21:641-653. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Riccò M, Ferraro P, Camisa V, Satta E, Zaniboni A, Ranzieri S, Baldassarre A, Zaffina S, Marchesi F. When a Neglected Tropical Disease Goes Global: Knowledge, Attitudes and Practices of Italian Physicians towards Monkeypox, Preliminary Results. Trop Med Infect Dis. 2022;7. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 103] [Cited by in RCA: 99] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 18. | Sahin TK, Erul E, Aksun MS, Sonmezer MC, Unal S, Akova M. Knowledge and Attitudes of Turkish Physicians towards Human Monkeypox Disease and Related Vaccination: A Cross-Sectional Study. Vaccines (Basel). 2022;11. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 41] [Cited by in RCA: 36] [Article Influence: 12.0] [Reference Citation Analysis (0)] |
| 19. | Dong C, Yu Z, Zhao Y, Ma X. Knowledge and vaccination intention of monkeypox in China's general population: A cross-sectional online survey. Travel Med Infect Dis. 2023;52:102533. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 37] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 20. | Harapan H, Setiawan AM, Yufika A, Anwar S, Wahyuni S, Asrizal FW, Sufri MR, Putra RP, Wijayanti NP, Salwiyadi S, Maulana R, Khusna A, Nusrina I, Shidiq M, Fitriani D, Muharrir M, Husna CA, Yusri F, Maulana R, Utomo PS, Andalas M, Wagner AL, Mudatsir M. Confidence in managing human monkeypox cases in Asia: A cross-sectional survey among general practitioners in Indonesia. Acta Trop. 2020;206:105450. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 47] [Cited by in RCA: 52] [Article Influence: 10.4] [Reference Citation Analysis (0)] |
| 21. | Desai AN, Malani PN. JYNNEOS Vaccine for Mpox. JAMA. 2023;329:1995. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 22. | Deputy NP, Deckert J, Chard AN, Sandberg N, Moulia DL, Barkley E, Dalton AF, Sweet C, Cohn AC, Little DR, Cohen AL, Sandmann D, Payne DC, Gerhart JL, Feldstein LR. Vaccine Effectiveness of JYNNEOS against Mpox Disease in the United States. N Engl J Med. 2023;388:2434-2443. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 217] [Cited by in RCA: 167] [Article Influence: 83.5] [Reference Citation Analysis (0)] |
| 23. | Cohn H, Bloom N, Cai GY, Clark JJ, Tarke A, Bermúdez-González MC, Altman DR, Lugo LA, Lobo FP, Marquez S; PVI study group, Chen JQ, Ren W, Qin L, Yates JL, Hunt DT, Lee WT, Crotty S, Krammer F, Grifoni A, Sette A, Simon V, Coelho CH. Mpox vaccine and infection-driven human immune signatures: an immunological analysis of an observational study. Lancet Infect Dis. 2023;23:1302-1312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 52] [Article Influence: 26.0] [Reference Citation Analysis (0)] |
| 24. | Harapan H, Setiawan AM, Yufika A, Anwar S, Wahyuni S, Asrizal FW, Sufri MR, Putra RP, Wijayanti NP, Salwiyadi S, Maulana R, Khusna A, Nusrina I, Shidiq M, Fitriani D, Muharrir M, Husna CA, Yusri F, Maulana R, Andalas M, Wagner AL, Mudatsir M. Knowledge of human monkeypox viral infection among general practitioners: a cross-sectional study in Indonesia. Pathog Glob Health. 2020;114:68-75. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 100] [Cited by in RCA: 113] [Article Influence: 22.6] [Reference Citation Analysis (0)] |
| 25. | Al-Tammemi AB, Albakri R, Alabsi S. The Outbreak of Human Monkeypox in 2022: A Changing Epidemiology or an Impending Aftereffect of Smallpox Eradication? Front Trop Dis. 2022;3:1-5. [RCA] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 26. | Sallam M, Al-Mahzoum K, Al-Tammemi AB, Alkurtas M, Mirzaei F, Kareem N, Al-Naimat H, Jardaneh L, Al-Majali L, AlHadidi A, Al-Salahat K, Al-Ajlouni E, AlHadidi NM, Bakri FG, Harapan H, Mahafzah A. Assessing Healthcare Workers' Knowledge and Their Confidence in the Diagnosis and Management of Human Monkeypox: A Cross-Sectional Study in a Middle Eastern Country. Healthcare (Basel). 2022;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 61] [Cited by in RCA: 56] [Article Influence: 18.7] [Reference Citation Analysis (0)] |
| 27. | Cailhol J, Gilson L, Lehmann U. A decade of aid coordination in post-conflict Burundi's health sector. Global Health. 2019;15:25. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 28. | Rimmer S, Barnacle J, Gibani MM, Wu MS, Dissanayake O, Mehta R, Herdman T, Gilchrist M, Muir D, Ebrahimsa U, Mora-Peris B, Dosekun O, Garvey L, Peters J, Davies F, Cooke G, Abbara A. The clinical presentation of monkeypox: a retrospective case-control study of patients with possible or probable monkeypox in a West London cohort. Int J Infect Dis. 2023;126:48-53. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 29. | Sherman L, Kuang M, Yang DD, Chappell K. An Overview of Continuing Medical Education/Continuing Professional Development Systems in China: A Mixed Methods Assessment. J CME. 2024;13:2363855. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 30. | Layland EK, Carter JA, Perry NS, Cienfuegos-Szalay J, Nelson KM, Bonner CP, Rendina HJ. A systematic review of stigma in sexual and gender minority health interventions. Transl Behav Med. 2020;10:1200-1210. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 80] [Article Influence: 16.0] [Reference Citation Analysis (0)] |
| 31. | Mumtaz G, Hilmi N, McFarland W, Kaplan RL, Akala FA, Semini I, Riedner G, Tawil O, Wilson D, Abu-Raddad LJ. Are HIV epidemics among men who have sex with men emerging in the Middle East and North Africa?: a systematic review and data synthesis. PLoS Med. 2010;8:e1000444. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 117] [Cited by in RCA: 109] [Article Influence: 7.3] [Reference Citation Analysis (0)] |
| 32. | Akour A, AlMuhaissen SA, Nusair MB, Al-Tammemi AB, Mahmoud NN, Jalouqa S, Alrawashdeh MN. The untold story of the COVID-19 pandemic: perceptions and views towards social stigma and bullying in the shadow of COVID-19 illness in Jordan. SN Soc Sci. 2021;1:240. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 11] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 33. | Mboussou F, Farham B, Nsasiirwe S, Atagbaza A, Oyaole D, Atuhebwe PL, Alegana V, Osei-Sarpong F, Bwaka A, Paluku G, Petu A, Efe-Aluta O, Kalu A, Bagayoko MM, Impouma B. COVID-19 Vaccination in the WHO African Region: Progress Made in 2022 and Factors Associated. Vaccines (Basel). 2023;11. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 34. | Huang X, Lin Z, Qin J, Yu D, Zhang F, Fang G, Chen X, He J, Cen P, Li M, Zhang R, Luo T, Jiang J, An S, Liang H, Ye L, Liang B. Willingness to accept monkeypox vaccine and its correlates among men who have sex with men in Southern China: a web-based online cross-sectional study. Front Public Health. 2024;12:1289918. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 7.0] [Reference Citation Analysis (0)] |