Published online Jan 6, 2025. doi: 10.12998/wjcc.v13.i1.95046
Revised: September 5, 2024
Accepted: September 20, 2024
Published online: January 6, 2025
Processing time: 221 Days and 3.8 Hours
The surgical approach for patellar instability usually refers to reconstruction of the medial patellofemoral ligament associated with an osteotomy of the tibial tuberosity or a trochleoplasty when required. The medial patellotibial ligament and the medial patellomeniscal ligament are secondary stabilizers of the patella. Despite this, both the medial patellotibial and patellofemoral ligaments aid in patellar rotation and tilt when the knee is flexed beyond 45°. The medial patellotibial ligament plays a particularly important role in the final stages of stretching in extension and between 40 degrees to 90 degrees of flexion. The clinical relevance and surgical indications for medial patellotibial ligament reconstruction associated with medial patellofemoral ligament reconstruction are still controversial. This editorial explores the surgical indications and clinical results for medial patellotibial ligament reconstruction to improve readers’ understanding of this technique, especially because reported clinical outcomes have remained sparse.
Core Tip: Though the medial patellotibial ligament reconstruction technique was described in 1922, its indication remains limited. Surgical indications are still not precisely delineated. Regardless, it is a viable option for young patients experiencing recurrent patellar instability with osseous abnormalities or patients facing severe instabilities in both extension and flexion.
- Citation: Zicaro JP, Garcia-Mansilla I. Navigating medial patellotibial ligament reconstruction: Clinical perspectives and surgical strategies. World J Clin Cases 2025; 13(1): 95046
- URL: https://www.wjgnet.com/2307-8960/full/v13/i1/95046.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v13.i1.95046
Patellar dislocations account for 2% to 3% of all knee injuries and are frequently observed in young and athletic patients[1,2]. Surgery becomes necessary in cases of recurrent instability to restore patellar stability. When addressing patellar instability, several parameters must be considered to determine the appropriate type of surgery, including patellar height, tibial tuberosity - trochlear groove (TT/TG) distance, and the rotations of the hip and ankle. Additionally, the medial patellar complex plays a critical role as a patellar stabilizer[3,4]. This structure consists of a primary stabilizer, the medial patellofemoral ligament (MPFL), and two secondary restraints, the medial patellotibial ligament (MPTL) and the medial patellomeniscal ligament (MPML). While the MPFL is the primary stabilizer and has been extensively studied in terms of postoperative outcomes, recent years have seen a growing recognition of the MPTL's role in cases of severe instability. In this editorial, our aim is to emphasize the role and relevance of the MPTL in patellar stability.
There is significant anatomical variability in the literature regarding the presence of the MPTL[4-6]. The MPTL and MPML are located within the second layer of the knee, as originally described by Warren and Marshall[7]. Both the MPTL and MPML have variable insertion points on the patella or tibia. Kaleka et al[5] reported a mean MPTL length of 46 mm (SD 8.8 mm), with the origin and insertion points being larger than the body of the ligament. Regarding patellar insertion, Hinckel et al[2] defined it as 3.6 mm proximal to the distal border of the patella. However, they noted different anatomical variations in the patellar insertion between the MPTL and MPML. While most specimens showed a combined patellar insertion, the MPML was proximal to the MPTL in three cases and the MPTL was proximal to the MPML in one case. The mean tibial insertion for the MPTL was 13.7 mm (ranging from 5 mm to 22 mm) distal to the joint line and medial to patellar tendon insertion.
There is consensus in the literature regarding the importance of the MPFL as the primary medial stabilizer of the patella[3,4,8]. In 1993, one of the earliest studies on MPTL biomechanics[9] indicated that it contributes less than 5% to total medial restraining forces. In 2006, Panagiotopoulos et al[9,10] used a similar method and sequentially sectioned the medial patellar ligaments at 30 degrees of flexion. They found that the MPTL contributed 13% to patellar stabilization, while the MPML contributed 24%. In 2012, Philippot et al[11] determined that the MPTL contributed 46%, 72%, and 92% to patellar shift, tilt, and rotation respectively, between 30 degrees and 90 degrees of flexion. These findings suggest that the MPTL plays a significant role in patellar stability at higher degrees of flexion. Regarding stiffness, strength and rupture, Hinckel et al[2] compared the characteristics of the MPFL with those of the MPTL and found that the MPTL was stiffer and exhibited less deformation at the maximum tensile strength (MTS), but showed no differences in force, energy at MTS, or energy for complete rupture.
Although the MPTL and the MPML are traditionally considered secondary stabilizers of patellar stability, their role in maintaining patellofemoral joint stability is increasingly recognized[1,4]. Their primary function occurs in the final phase of extension, where they counteract the proximal lateral traction of the quadriceps. They also become taut at higher degrees of flexion, playing a significant role in restricting lateral translation of the patella. Furthermore, the MPTL and MPML are essential for preserving proper patellar tracking, helping to maintain normal patellar tilt and rotation. Recent proposals suggest that reconstructing the MPFL in conjunction with the MPTL may offer an effective solution for enhancing patellar stability, particularly near full extension.
There is considerable controversy regarding the specific surgical indications for MPTL reconstruction (MPTL-R)[2,4,8,12]. Among the initial reports, Zaffagnini et al[12] suggested performing an isolated MPTL-R in conjunction with distal realignment or trochleoplasty for patients with recurrent patellar instability. More recently, Hinckel et al[2] outlined specific indications for MPTL-R, including subluxation in extension, instability in flexion, knee hyperextension with ligamentous laxity, and skeletal immaturity with associated risk factors. Most authors concur that MPTL-R, whether performed in isolation or in combination with MPFL reconstruction (MPFL-R), can provide additional stability to the patella, especially in cases where anatomical factors such as TT/TG, patellar height, or trochlear dysplasia cannot be addressed, such as in skeletally immature patients[4,8,13,14].
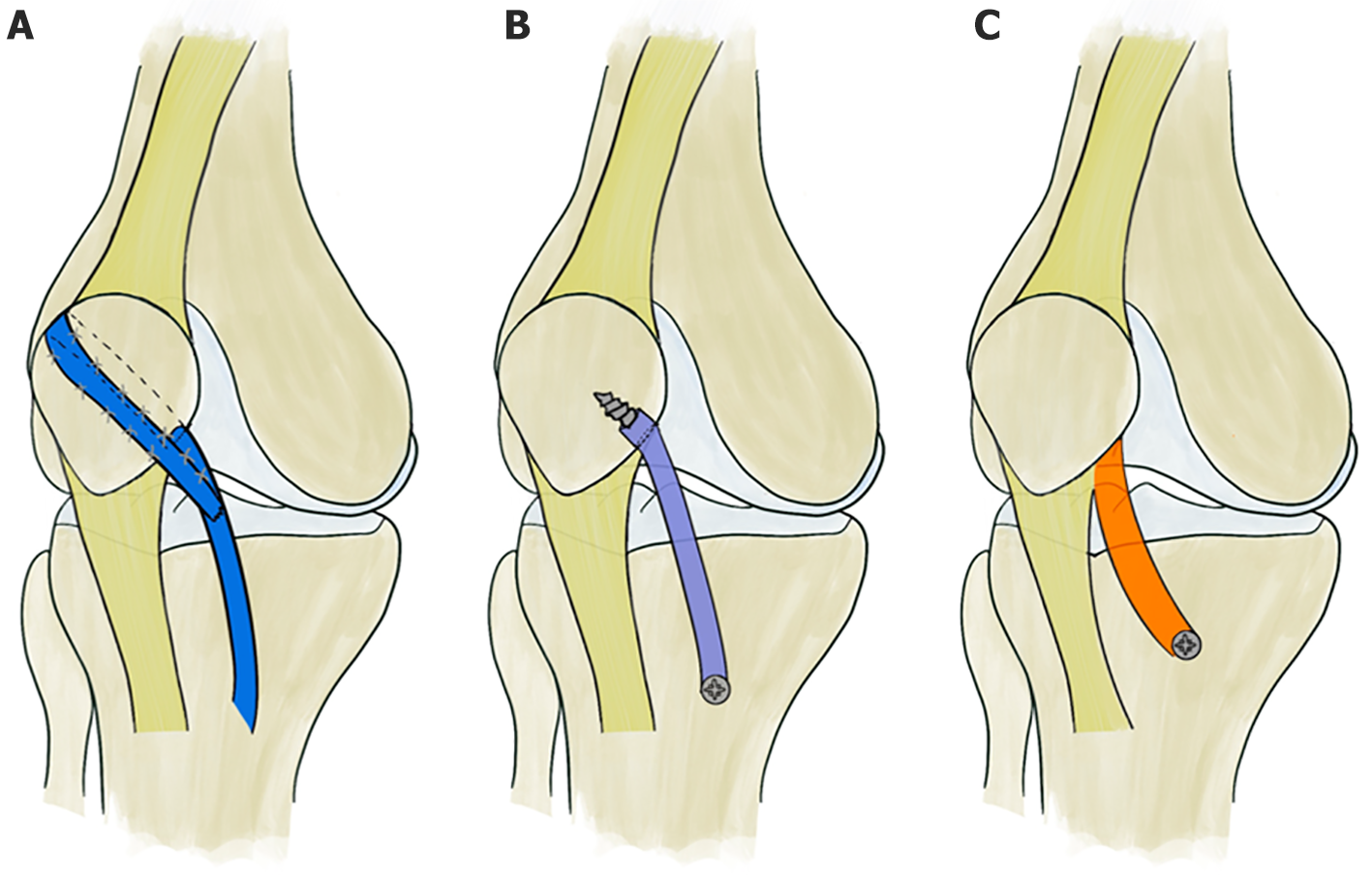
One of the most renowned techniques in MPTL-R is semitendinosus tenodesis[15-17], initially introduced by Galeazzi in 1922. This method was modified by Fiume in 1954[18], incorporating lateral retinacular release and medial retinacular reefing. Subsequently, in 1972, Baker et al[19] further refined this technique by creating an oblique tunnel across the patella along the line of the tenodesis, facilitating the passage of the semitendinosus tendon from the medial to the lateral side (Figure 1A).
An alternative to tenodesis is MPTL-R[20,21]. In such instances, patellar fixation is accomplished through a tunnel, resembling the technique delineated by Galeazzi. Concurrently, tibial fixation involves the utilization of either an anchor or a tenodesis screw (Figure 1B).
Some authors, such as Rillmann et al[22] and Zaffagnini et al[12] have utilized the medial segment of the patellar tendon along with a bone block sourced from the tibial tuberosity. In contrast, Myers et al[23] and Oliva et al[24] solely employed the patellar tendon (Figure 1C).
There is still limited data available, with only a few published series reporting on the outcomes of MPTL-R. Zaffagnini et al[12] indicated isolated MPTL-R using the medial third of the patellar tendon, relocating the distal insertion next to the medial collateral ligament, with 10% of cases associated with distal realignment and 21% with trochleoplasty. Out of 32 patients with a mean follow-up of 6.1 years, they reported a 14% failure rate. In contrast to these results, Ambra et al[25] performed a biomechanical study comparing MPFL-R and MPTL-R and concluded that isolated MPTL-R fails to restore lateral patellar stability when compared to MPFL-R.
The combination of MPFL-R and MPTL-R has shown more promising outcomes. Leite et al[13] found that MPFL-R combined with MPTL-R in skeletally immature patients with additional uncorrected anatomical patellofemoral abnormalities leads to acceptable clinical outcomes within a minimum of 5 years follow-up, although it has a high failure rate of 24.1%. The addition of MPTL-R to the MPFL may result in decreased patellar laxity on physical exams, as demonstrated by improved patellar glide, patellar tilt test, and reduced subluxation in extension. Finally, Abbaszadeh et al[4] in a systematic review and meta-analysis evaluated five prospective series and found it to be an effective method for patients with patella alta or trochlea dysplasia, where no bony procedures such as TTO and trochleoplasty could be performed. However, none of the studies were comparative with isolated MPFL or combined with bony procedures.
In conclusion, MPTL-R remains a relatively underexplored area in the literature, with limited published series reporting outcomes. Current studies suggest that MPTL-R, whether performed in isolation or in combination with MPFL-R, can provide additional patellar stability, particularly in cases where anatomical factors cannot be addressed. While isolated MPTL-R has shown some success, it may not fully restore lateral patellar stability compared to MPFL-R. Further research is necessary to gain better understanding of the role of MPTL-R in patellar stability and to refine surgical indications.
The figure was made by Dr. Hernan Sanchez Mele.
| 1. | Baumann CA, Pratte EL, Sherman SL, Arendt EA, Hinckel BB. Reconstruction of the medial patellotibial ligament results in favorable clinical outcomes: a systematic review. Knee Surg Sports Traumatol Arthrosc. 2018;26:2920-2933. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 24] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 2. | Hinckel BB, Lipinski L, Arendt EA. Concepts of the Distal Medial Patellar Restraints: Medial Patellotibial Ligament and Medial Patellomeniscal Ligament. Sports Med Arthrosc Rev. 2019;27:143-149. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 5] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 3. | Felli L, Alessio-Mazzola M, Lovisolo S, Capello AG, Formica M, Maffulli N. Anatomy and biomechanics of the medial patellotibial ligament: A systematic review. Surgeon. 2021;19:e168-e174. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 15] [Article Influence: 3.8] [Reference Citation Analysis (0)] |
| 4. | Abbaszadeh A, Saeedi M, Hoveidaei AH, Dadgostar H, Razi S, Razi M. Combined medial patellofemoral ligament and medial patellotibial ligament reconstruction in recurrent patellar instability: A systematic review and meta-analysis. World J Clin Cases. 2023;11:4625-4634. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Reference Citation Analysis (0)] |
| 5. | Kaleka CC, Aihara LJ, Rodrigues A, de Medeiros SF, de Oliveira VM, de Paula Leite Cury R. Cadaveric study of the secondary medial patellar restraints: patellotibial and patellomeniscal ligaments. Knee Surg Sports Traumatol Arthrosc. 2017;25:144-151. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 20] [Cited by in RCA: 18] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 6. | Hinckel BB, Gobbi RG, Demange MK, Pereira CAM, Pécora JR, Natalino RJM, Miyahira L, Kubota BS, Camanho GL. Medial Patellofemoral Ligament, Medial Patellotibial Ligament, and Medial Patellomeniscal Ligament: Anatomic, Histologic, Radiographic, and Biomechanical Study. Arthroscopy. 2017;33:1862-1873. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 44] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 7. | Warren LF, Marshall JL. The supporting structures and layers on the medial side of the knee: an anatomical analysis. J Bone Joint Surg Am. 1979;61:56-62. [PubMed] |
| 8. | Hetsroni I, Mann G, Dolev E, Nyska M. Combined reconstruction of the medial patellofemoral and medial patellotibial ligaments: outcomes and prognostic factors. Knee Surg Sports Traumatol Arthrosc. 2019;27:507-515. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 11] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 9. | Conlan T, Garth WP Jr, Lemons JE. Evaluation of the medial soft-tissue restraints of the extensor mechanism of the knee. J Bone Joint Surg Am. 1993;75:682-693. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 619] [Cited by in RCA: 548] [Article Influence: 17.1] [Reference Citation Analysis (0)] |
| 10. | Panagiotopoulos E, Strzelczyk P, Herrmann M, Scuderi G. Cadaveric study on static medial patellar stabilizers: the dynamizing role of the vastus medialis obliquus on medial patellofemoral ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:7-12. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 186] [Cited by in RCA: 164] [Article Influence: 8.6] [Reference Citation Analysis (0)] |
| 11. | Philippot R, Boyer B, Testa R, Farizon F, Moyen B. The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports Traumatol Arthrosc. 2012;20:331-336. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 118] [Cited by in RCA: 134] [Article Influence: 10.3] [Reference Citation Analysis (0)] |
| 12. | Zaffagnini S, Grassi A, Marcheggiani Muccioli GM, Luetzow WF, Vaccari V, Benzi A, Marcacci M. Medial patellotibial ligament (MPTL) reconstruction for patellar instability. Knee Surg Sports Traumatol Arthrosc. 2014;22:2491-2498. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 40] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 13. | Leite CBG, Hinckel BB, Ribeiro GF, Giglio PN, Santos TP, Bonadio MB, Arendt E, Gobbi RG. Medial patellofemoral ligament reconstruction in skeletally immature patients without correction of bony risk factors leads to acceptable outcomes but higher failure rates. J ISAKOS. 2023;8:189-196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Aicale R, Maffulli N. Combined medial patellofemoral and medial patellotibial reconstruction for patellar instability: a PRISMA systematic review. J Orthop Surg Res. 2020;15:529. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 14] [Cited by in RCA: 12] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 15. | Grannatt K, Heyworth BE, Ogunwole O, Micheli LJ, Kocher MS. Galeazzi semitendinosus tenodesis for patellofemoral instability in skeletally immature patients. J Pediatr Orthop. 2012;32:621-625. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 36] [Cited by in RCA: 28] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 16. | Letts RM, Davidson D, Beaule P. Semitendinosus tenodesis for repair of recurrent dislocation of the patella in children. J Pediatr Orthop. 1999;19:742-747. [PubMed] |
| 17. | Moyad TF, Blakemore L. Modified Galeazzi technique for recurrent patellar dislocation in children. Orthopedics. 2006;29:302-304. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 18. | Fiume M. [Galeazzi's patellapexy in recurrent dislocation of the patella]. Minerva Ortop. 1954;5:171-174. [PubMed] |
| 19. | Baker RH, Carroll N, Dewar FP, Hall JE. The semitendinosus tenodesis for recurrent dislocation of the patella. J Bone Joint Surg Br. 1972;54:103-109. [PubMed] |
| 20. | Drez D Jr, Edwards TB, Williams CS. Results of medial patellofemoral ligament reconstruction in the treatment of patellar dislocation. Arthroscopy. 2001;17:298-306. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 253] [Cited by in RCA: 226] [Article Influence: 9.4] [Reference Citation Analysis (0)] |
| 21. | Hinckel BB, Gobbi RG, Bonadio MB, Demange MK, Pécora JR, Camanho GL. Reconstruction of medial patellofemoral ligament using quadriceps tendon combined with reconstruction of medial patellotibial ligament using patellar tendon: initial experience. Rev Bras Ortop. 2016;51:75-82. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 8] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 22. | Rillmann P, Dutly A, Kieser C, Berbig R. Modified Elmslie-Trillat procedure for instability of the patella. Knee Surg Sports Traumatol Arthrosc. 1998;6:31-35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 35] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 23. | Myers P, Williams A, Dodds R, Bülow J. The three-in-one proximal and distal soft tissue patellar realignment procedure. Results, and its place in the management of patellofemoral instability. Am J Sports Med. 1999;27:575-579. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 55] [Cited by in RCA: 43] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 24. | Oliva F, Ronga M, Longo UG, Testa V, Capasso G, Maffulli N. The 3-in-1 procedure for recurrent dislocation of the patella in skeletally immature children and adolescents. Am J Sports Med. 2009;37:1814-1820. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 62] [Cited by in RCA: 67] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 25. | Ambra LF, Franciozi CE, Phan A, Faloppa F, Gomoll AH. Isolated MPTL reconstruction fails to restore lateral patellar stability when compared to MPFL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2021;29:793-799. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |