Published online Mar 26, 2024. doi: 10.12998/wjcc.v12.i9.1560
Peer-review started: October 5, 2023
First decision: January 9, 2024
Revised: February 2, 2024
Accepted: February 26, 2024
Article in press: February 26, 2024
Published online: March 26, 2024
Processing time: 171 Days and 21.9 Hours
Unicompartmental knee arthroplasty (UKA) has great advantages in the treatment of unicompartmental knee osteoarthritis, but its revision rate is higher than that of total knee arthroplasty.
To summarize and analyse the causes of revision after UKA.
This is a retrospective case series study in which the reasons for the first revision after UKA are summarized. We analysed the clinical symptoms, medical histories, laboratory test results, imaging examination results and treatment processes of the patients who underwent revision and summarized the reasons for primary revision after UKA.
A total of 13 patients, including 3 males and 10 females, underwent revision surgery after UKA. The average age of the included patients was 67.62 years. The prosthesis was used for 3 d to 72 months. The main reasons for revision after UKA were improper suturing of the surgical opening (1 patient), osteophytes (2 patients), intra-articular loose bodies (2 patients), tibial prosthesis loosening (2 patients), rheumatoid arthritis (1 patient), gasket dislocation (3 patients), anterior cruciate ligament injury (1 patient), and medial collateral ligament injury with residual bone cement (1 patient).
The causes of primary revision after UKA were gasket dislocation, osteophytes, intra-articular loose bodies and tibial prosthesis loosening. Avoidance of these factors may greatly reduce the rate of revision after UKA, improve patient satisfaction and reduce medical burden.
Core Tip: Despite the many advantages of unicompartmental knee arthroplasty (UKA), the long-term survival rate of implants and the rate of UKA revision remain controversial. Therefore, clarifying the reasons that may cause UKA revision can further reduce the revision rate of UKA surgery. We found that the main reasons for the initial revision of UKA were gasket dislocation, osteophytes, intra-articular loose bodies and tibial prosthesis loosening. Avoiding these factors may greatly reduce the revision rate after UKA surgery, improve patient satisfaction, and reduce medical burden.
- Citation: Zhao JL, Jin X, Huang HT, Yang WY, Li JH, Luo MH, Liu J, Pan JK. Analysis of the causes of primary revision after unicompartmental knee arthroplasty: A case series. World J Clin Cases 2024; 12(9): 1560-1568
- URL: https://www.wjgnet.com/2307-8960/full/v12/i9/1560.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i9.1560
Joint arthroplasty, such as total knee arthroplasty (TKA) or unicompartmental knee arthroplasty (UKA), is often used to treat end-stage unicompartmental knee osteoarthritis[1,2]. Compared with patients who undergo TKA, those who undergo UKA have smaller surgical wounds, recover faster postoperatively, have less blood loss, are more likely to have the anterior and posterior cruciate ligament preserved, as well as proprioception, a lower osteotomy rate, a shorter hospital stay, and lower costs[3-5]. Although UKA has many advantages, the long-term prosthesis survival rate and rate of revision after UKA are still controversial[6,7]. Many existing studies show that the rate of revision after UKA is much higher than that after TKA, and the main reason is aseptic loosening[8,9]. In this context, exploring and summarizing the causes that may lead to revision after UKA would be conducive to further reducing the UKA revision rate, which is highly valuable for orthopaedic surgeons and patients.
Although the rate of revision after UKA is higher than that after TKA, the total number of revisions after UKA is still relatively low; therefore, summarizing the causes of revision among UKA patients is necessary. By reviewing and analysing the causes of revision after UKA, we established references for the early detection of risk factors for revision in clinical practice and for formulating surgical strategies and rehabilitation programmes.
This was a retrospective case series study in which the reasons for primary revision after UKA were summarized. The inclusion criteria were as follows: (1) Indications for revision after UKA in the Department of Orthopaedics of Guangdong Provincial Hospital of Traditional Chinese Medicine from November 2016 to December 2020; and (2) First revision treatment after UKA (same side) (patients who underwent revision after the primary revision were not included). There were no restrictions regarding age, weight, race, activity or surgical materials used for UKA.
We used the electronic medical records system to extract and analyse the baseline data of the included patients, such as age, sex, surgical side and prosthesis use time. In addition, we comprehensively analysed the reasons for revision after UKA among the included patients according to their medical histories, imaging data, physical and chemical test results, intraoperative conditions and pathological results. We also followed up on the recovery of the included patients after revision.
We used SPSS 25.0 software for the statistical analysis of the counts and descriptive statistics. The measurement data are expressed as the mean ± SD.
This retrospective case series study was approved by the Ethics Committee of Guangdong Provincial Hospital of Traditional Chinese Medicine, No. YE2021-370-01.
From November 2016 to December 2020, a total of 13 patients (13 knees), 3 males (23.08%) and 10 females (76.92%), underwent primary revision after UKA in our hospital (Table 1). The minimum age of the 13 patients included was 59 years, the maximum age was 76 years, and the average age was 67.62 years (standard deviation 5.88 years). There were 5 (38.46%) and 8 (61.54%) left and right knees, respectively, that underwent revision surgery after UKA. The prosthesis was used for 3 d to 72 months. The main causes of revision in 13 patients were improper suturing of the surgical opening (1 patient), osteophytes (2 patients), articular cavity free bodies (2 patients), tibial prosthesis loosening (2 patients), rheumatoid arthritis (RA) (1 patient), pad dislocation (3 patients), anterior cruciate ligament (ACL) injury (1 patient), and medial collateral ligament injury with residual bone cement (1 patient). As of February 2021, we have followed up all 13 patients who underwent revision surgery after UKA for at least half a year, and all patients have achieved good joint function.
| Case | Sex | Age (yr) | Side of knee | Year of revision | Duration of prosthesis | Cause for UKA revision | Outcome of UKA revision |
| Patient 1 | Female | 61 | Right | 2017 | 1 month | Improper suture | Cured |
| Patient 2 | Male | 69 | Right | 2018 | 4 months | Osteophyte | Cured |
| Patient 3 | Male | 67 | Right | 2017 | 5 months | Osteophyte | Cured |
| Patient 4 | Female | 59 | Left | 2018 | 20 months | Intra-articular loose body | Cured |
| Patient 5 | Female | 70 | Left | 2020 | 36 months | Intra-articular loose body | Cured |
| Patient 6 | Male | 75 | Right | 2018 | 8 months | Tibial prosthesis loosening | Cured |
| Patient 7 | Female | 70 | Left | 2018 | 23 months | Tibial prosthesis loosening | Cured |
| Patient 8 | Female | 76 | Right | 2017 | 72 months | Rheumatoid arthritis | Cured |
| Patient 9 | Female | 76 | Right | 2018 | 15 months | ACL injury | Cured |
| Patient 10 | Female | 63 | Right | 2019 | 7 months | Gasket dislocation | Cured |
| Patient 11 | Female | 63 | Right | 2016 | 48 months | Gasket dislocation | Cured |
| Patient 12 | Female | 69 | Left | 2018 | 10 months | Gasket dislocation | Cured |
| Patient 13 | Female | 61 | Left | 2018 | 3 d | Medial collateral ligament injury and bone cement residue | Cured |
Improper suture: Patient 1, a 61-year-old female, underwent right-knee mobile-bearing UKA. She sought medical help because her right knee was red, swollen, hot and painful for 3 d. The lower part of the surgical opening of the right knee in Patient 1 was ulcerated and exuded, and the ulceration was round, measuring 0.5 cm × 0.5 cm. After the patient was admitted to the hospital, wound secretions and joint fluids were immediately collected for bacterial culture. No obvious abnormalities were found in the joint fluid test, and X-ray showed that the prosthesis was in a good position. Based on the above medical history and examination results, we ruled out intra-articular infection and decided to administer debridement treatment. During the operation, we found that the lower part of the original incision in the right knee had obvious inflammatory hyperplasia and subcutaneous soft tissue necrosis, and the wound was not connected to the joint cavity. Tissues near the surgical opening were sent for pathological examination. We thoroughly debrided- the necrotic incision during the operation. Postoperative pathology revealed hyperplasia of fibres and small vessels and infiltration of lymphocytes and neutrophils in the local area in the subcutaneous tissue of the right knee, which was consistent with inflammatory changes and multinuclear giant cell reactions. No bacteria were found in the preoperative wound secretion, joint fluid or intraoperative joint fluid culture. Based on the UKA surgical records of the patient and what we observed during the revision, we found that the original surgeon used bidirectional barbed suture, which is not suitable for suturing subcutaneous tissue. We believe that the application of knot-free sutures is the reason for the revision after UKA in Patient 1 (Figure 1).
Osteophytes: Patient 2, a 69-year-old male, underwent mobile-bearing UKA. He was admitted to the hospital because of pain in the upper lateral region of the right knee 4 months after UKA. Before revision, X-ray imaging revealed osteophytes on the lateral condyle of the right knee. We used a small incision to remove the osteophyte from the lateral condyle of the right knee. Postoperative X-ray showed that the osteophytes of the lateral condyle of the right knee had been removed (Supplementary Figure 1).
Patient 3, a 67-year-old male, underwent right-knee mobile-bearing UKA. He was admitted to the hospital due to postoperative pain in the right knee for 5 months. This patient underwent right-knee UKA at an external hospital 5 months prior and continued to experience medial anterior pain in the right knee after UKA. X-ray imaging showed that the tibial prosthesis was placed excessively inwards. Dual computed tomography (CT) showed osteophytes in front of the femoral prosthesis, and we confirmed this in the revision. During the knee joint activity test during revision, we found that the osteophyte collided with the tibial platform and that the bone cement at the lower front of the tibial platform prosthesis was broken, which seriously affected the stability of the tibial platform prosthesis. We cleaned the osteophytes, removed the tibial platform prosthesis, renovated it, and finally installed a new tibial platform prosthesis (Figure 2).
Intra-articular loose body: Two patients needed revision because of the presence of a free body in the joint cavity, and the clinical symptoms of both patients were obvious interlocking symptoms. We performed an arthroscopic downstream extracorporeal surgery.
Patient 4, a 59-year-old female, underwent mobile-bearing UKA of the left knee. She was hospitalized due to pain and locked symptoms for 1 month on the medial side of the left knee. After preoperative imaging and surgical exploration, we confirmed that the mass was free of residual bone cement.
Patient 5, a 70-year-old female, underwent fixed-bearing UKA. The patient was hospitalized due to swelling and pain in the left knee for 2 years. Dual CT showed that there was a bone-free body between the tibial prosthesis and the femoral prosthesis (Figure 3).
Tibial prosthesis loosening: Two patients underwent fixed-bore UKA. The tibial platform prosthesis became loose, so we revised the operation to TKA.
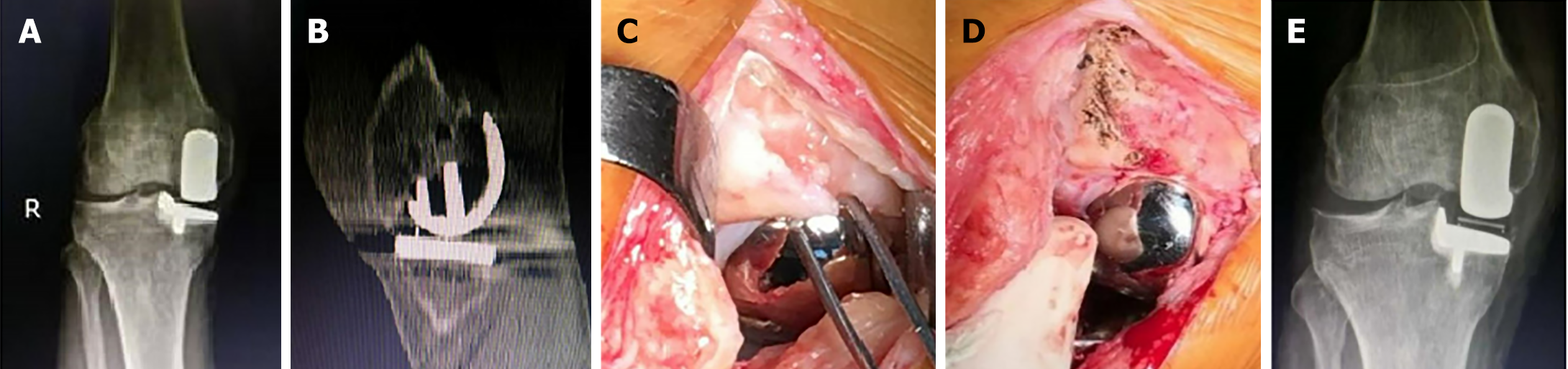
Patient 6, a 75-year-old male, was admitted to the hospital due to walking pain for 8 months after right-knee UKA. X-ray imaging revealed an interface under the tibial platform prosthesis, and compared with the previous X-ray after UKA, we found a change in the tibial prosthesis position. The tibial plateau was easily removed with forceps during the operation (Figure 4).
Patient 7, a 70-year-old female, sought medical help because of weakness in the medial side of the left knee for 16 months. The X-ray and intraoperative conditions were similar to those of Patient 6.
RA: Patient 8, a 76-year-old female, underwent mobile-bearing UKA of the right knee. She sought medical help because of swelling and pain in the right knee and ankle for one year after UKA. The patient had undergone right-knee UKA 6 years prior and recovered well after the operation. Afterwards, she suffered from repeated swelling and pain in the right knee and ankle for one year. The rheumatoid antibody test confirmed RA, and a large amount of inflammatory synovium in the suprapatellar bursa and cartilage degeneration damage in the lateral compartment of the knee joint were observed during the revision. The prosthesis was easily and completely removed during the operation, and the knee joint was rebuilt during TKA (Figure 5).
ACL injury: Patient 9, a 76-year-old female, underwent fixed-bearing UKA of the right knee. She sought medical help because of postoperative pain in the right knee and limited mobility. Imaging before UKA indicated that the patient's right knee ACL was broken. X-ray imaging revealed that the right-knee tibia was moved forward, so fixed-bearing UKA was performed. Half a year after UKA, the patient developed instability of the knee joint and repeated pain, and the X-ray showed that the right-knee tibia had moved forward significantly. Following the patient's wishes, TKA was performed after conservative treatment failed (Figure 6).
Gasket dislocation: Three patients underwent mobile-bearing UKA.
Patient 10, a 63-year-old female, developed knee joint pain and limited activity 7 months after right-knee UKA. The X-ray image indicated that the gasket was dislocated forward. We performed knee flexion and extension tests with the original 3-mm pad. At the buckling position, the 3-mm gasket became loose, the 4-mm gasket was under proper tension, and the 5-mm gasket was too tight. The 3-mm gasket was in good condition, the 4-mm gasket was slightly tight, and the 5-mm gasket was very tight and straight. After the above tests, we replaced the gasket with a 4-mm gasket (Supplementary Figure 2).
Patient 11, a 63-year-old female, suffered from pain in the right knee and walking instability after UKA, which persisted for 4 months. The X-ray images indicated that the gasket was dislocated both backwards and downwards. We tested the range of motion of the knee joint and the position of the spacer during the revision, and the results showed that the uneven flexion extension space and poor placement of the femoral prosthesis led to a poor trajectory of the spacer. Finally, the case was revised to TKA (Supplementary Figure 3).
Patient 12, a 69-year-old female, underwent one-stage double-knee UKA at another hospital. She suffered from dislocation of the right knee pad half a year after UKA and returned to the external hospital for revision by TKA. Two months later, the patient had another anterior dislocation of the left knee pad. We compared the postoperative X-ray data of the patient with those of a patients whose prosthesis was placed in the Oxford Monocondyle Course[10] and found that the patient's bilateral femoral prostheses were close to the femur without overhang, which indicated residual osteophytes behind the femur and that the selected femoral prostheses were small. We found two problems at the same time during the operation: first, when the knee joint was in extreme flexion, the pad was moved forward, indicating that there was a rear impact; second, there were residual osteophytes of the femoral medial condyle, leading to the operator's incorrect assessment of the left and right diameters of the femoral medial condyle, and the femoral prosthesis being placed inwards, causing poor tracking of the spacer when the knee joint moved. We completely removed the osteophytes and placed the femoral prosthesis laterally. In addition, we replaced a larger femoral prosthesis and thickened pads (Figure 7).
Injury to the medial collateral ligament and residual bone cement: Patient 13, a 61-year-old female, underwent mobile-bearing UKA of her left knee. The patient was unable to walk and had pain in his left knee. Patient 13 underwent reoperation due to postoperative genu valgus with medial collateral ligament injury and residual bone cement. X-ray showed that the vertical osteotomy of the tibia was inwards, there was more medial suspension of the tibial prosthesis, and there was remaining bone cement. Physical examination revealed grade II damage to the medial collateral ligament. We performed bone cement cleaning+medial collateral ligament repair+shim (small 1) revision 3 d after UKA (Figure 8). This patients underwent revision due to the inexperience of the operator and technical failure.
In this study, we summarized the causes of 13 cases of revision after UKA, which we believe can provide a valuable reference for orthopaedic surgeons evaluating patient conditions and selecting surgical methods. Owing to the large advantages of UKA for the treatment of unicompartmental knee osteoarthritis, it is extremely important to reduce or even eliminate the risk of revision after UKA. Circumventing the risk factors leading to revision after UKA summarized in this study may be beneficial for selecting UKA for the treatment of unicompartmental knee osteoarthritis and achieving better clinical outcomes.
In this study, gasket dislocation (3/13) was the main cause of revision after UKA. Compared with fixed-bearing prostheses, movable prostheses are more prone to dislocation. The 3 patients with spacer dislocation included in this study were all treated with mobile-bearing UKA. Pad dislocation occurs in 0.9% to 4.0% of cases[11], almost all of which occur in movable platform-type single condyle prostheses. We believe that the most common cause of iatrogenic gasket dislocation is insufficient gasket containment, which is often related to surgical errors. We believe that it is very important to fully evaluate and select the correct thickness of the shims and appropriate prostheses before or during UKA. For the treatment of dislocation of the pad after UKA, the operator needs to fully evaluate the position of the femoral and tibial prosthesis components, the balance of the knee joint space, and the state of the soft tissue and accurately determine the cause of dislocation to select the replacement pad model or revision. According to the results of the revision of Patient 12, we believe that the technical focus should be on the selection of a femoral prosthesis, which should be greater than or equal to the original prosthesis.
The proportion of UKA revisions caused by osteophytes, articular cavity free bodies and tibial prosthesis loosening was 15.35%. We believe that osteophytes, bone cement or bone residue caused by technical reasons should be considered by bone surgeons. The presence of osteophytes and an intra-articular loose body is likely to cause an impact between the prosthesis and the bone structure, which may lead to loosening of the prosthesis, fracture around the prosthesis, dislocation of the pad, degeneration or tearing of the cruciate ligament[12-14]. Therefore, the operator should be familiar with the technical needs of UKA. During the operation, the osteophyte and bone cement residue at risk of impact should be completely removed, and the hyperplastic synovium of the joint should be removed if necessary. When osteophytes or loose bodies in the joint cavity are found early after UKA without causing serious impact, we believe that cleaning up the hyperplastic osteophytes, synovium, and residual or fallen bone cement under arthroscopy is appropriate, which was also verified in our follow-up. If severe impact complications occur, orthopaedic surgeons should choose to perform pad replacement, single condylar prosthesis replacement or TKA revision according to the type of complication.
There were 1 case of improper suture, 1 case of RA, 1 case of ACL injury, and 1 case of medial collateral ligament injury with residual bone cement. Generally, UKA results in a smaller incision and less soft tissue damage, and the infection risk associated with UKA is lower than that associated with TKA. Therefore, UKA should be performed under strict aseptic conditions, and standardized surgical suturing procedures should be upheld. The medial collateral ligament and the ACL are important for maintaining joint stability and participating in flexion and extension activities, and their functional integrity is one of the necessary conditions for selecting UKA. Therefore, we carefully evaluated the function of the lateral collateral ligament and the ACL before the operation, especially the location and direction of the vertical osteotomy of the tibial plateau. The orthopaedic surgeon should focus on protecting the medial collateral ligament during horizontal osteotomy, which can reduce the risk of such complications. For patients with a family history of RA or who are considered susceptible patients, orthopaedic surgeons should fully communicate with patients before surgery and conduct corresponding RA screening tests, which may help reduce the rate of UKA revision due to RA. For elderly patients and those who are at high risk of RA, we think that TKA may be a more suitable choice.
This was a retrospective case study. The main defects of this study design are memory bias and nonresponse bias. Second, because a small number of patients were included, the representativeness of the data was poor. Therefore, the conclusions of this study should be considered in light of the above limitations.
This study revealed that the causes of revision after UKA were mainly gasket dislocation, osteophytes, intra-articular loose bodies and tibial prosthesis loosening. Circumventing these factors may greatly reduce the rate of UKA revision, improve patient satisfaction and reduce medical burden. In addition, UKA is critical for comprehensively and objectively assessing the knee ligament status and RA risk of patients to subsequently select the appropriate surgical method (UKA or TKA).
Unicompartmental knee arthroplasty (UKA) has great advantages in the treatment of unicompartmental knee osteoarthritis, but its revision rate is higher than that of total knee arthroplasty.
Providing a reference for orthopaedic surgeons to reduce the revision rate and improve patient satisfaction.
The study aims to summarize and analyse the causes of revision after UKA.
This is a retrospective case series summarizing the reasons for the first revision after UKA in the Department of Orthopedics of Guangdong Provincial Hospital of Traditional Chinese Medicine from November 2016 to December 2020. We analysed data on the clinical symptoms, medical history, laboratory tests, imaging examinations and treatment process of the revision cases and summarized the reasons for primary revision after UKA among all cases.
Thirteen patients, including 3 males and 10 females, underwent revision surgery after UKA. The average age of the included patients was 67.62 years. The main reasons for revision after UKA were improper suturing of the surgical opening, osteophytes, intra-articular loose bodies, tibial prosthesis loosening, rheumatoid arthritis, gasket dislocation, anterior cruciate ligament injury, and medial collateral ligament injury with residual bone cement.
The causes of primary revision after UKA were gasket dislocation, osteophytes, intra-articular loose bodies and tibial prosthesis loosening.
Avoidance of these factors found in this study may greatly reduce the rate of revision after UKA, improve patient satisfaction and reduce medical burden.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ng BW, Malaysia S-Editor: Fan JR L-Editor: A P-Editor: Chen YX
| 1. | Casper DS, Fleischman AN, Papas PV, Grossman J, Scuderi GR, Lonner JH. Unicompartmental Knee Arthroplasty Provides Significantly Greater Improvement in Function than Total Knee Arthroplasty Despite Equivalent Satisfaction for Isolated Medial Compartment Osteoarthritis. J Arthroplasty. 2019;34:1611-1616. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 49] [Article Influence: 8.2] [Reference Citation Analysis (0)] |
| 2. | Kievit AJ, Kuijer PPFM, de Haan LJ, Koenraadt KLM, Kerkhoffs GMMJ, Schafroth MU, van Geenen RCI. Patients return to work sooner after unicompartmental knee arthroplasty than after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2020;28:2905-2916. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 18] [Cited by in RCA: 31] [Article Influence: 6.2] [Reference Citation Analysis (0)] |
| 3. | Haffar A, Ali R, Mehta N, Patel A, Fricka KB, Della Valle CJ, Gerlinger TL, Krueger CA, Lonner JH. Prior Anterior Cruciate Ligament Reconstruction Does Not Compromise the Functional Outcomes of Medial Unicompartmental Knee Arthroplasty Although Revision for Progressive Arthritis May Occur Earlier. J Arthroplasty. 2022;37:238-242. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Janssen SJ, van Oost I, Breugem SJM, van Geenen RCI. A structured evaluation of the symptomatic medial Oxford unicompartmental knee arthroplasty (UKA). EFORT Open Rev. 2021;6:850-860. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 5] [Reference Citation Analysis (0)] |
| 5. | Yang G, Jiao X, Li Q, Li Z, An S, Feng M, Gao G, Huang J, Cao G. Hybrid Oxford unicompartmental knee arthroplasty has lower residual cement extrusion than cemented arthroplasty in treating end-stage unicompartmental knee osteoarthritis. BMC Musculoskelet Disord. 2021;22:833. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW. Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res. 2012;470:84-90. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 181] [Cited by in RCA: 202] [Article Influence: 15.5] [Reference Citation Analysis (0)] |
| 7. | Lombardi AV Jr, Kolich MT, Berend KR, Morris MJ, Crawford DA, Adams JB. Revision of Unicompartmental Knee Arthroplasty to Total Knee Arthroplasty: Is It as Good as a Primary Result? J Arthroplasty. 2018;33:S105-S108. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 48] [Article Influence: 6.9] [Reference Citation Analysis (0)] |
| 8. | Ma J, Yan Y, Wang W, Wang B, Yue D, Guo W. Lower early revision rates after uncemented Oxford Unicompartmental Knee Arthroplasty (UKA) than cemented Oxford UKA: A meta-analysis. Orthop Traumatol Surg Res. 2021;107:102802. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 5] [Cited by in RCA: 13] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 9. | Arias-de la Torre J, Valderas JM, Evans JP, Martín V, Molina AJ, Muñoz L, Pons-Cabrafiga M, Espallargues M; Catalan Arthroplasty Register Steering Committee (RACat). Differences in Risk of Revision and Mortality Between Total and Unicompartmental Knee Arthroplasty. The Influence of Hospital Volume. J Arthroplasty. 2019;34:865-871. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 10] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 10. | Mukherjee K, Pandit H, Dodd CA, Ostlere S, Murray DW. The Oxford unicompartmental knee arthroplasty: a radiological perspective. Clin Radiol. 2008;63:1169-1176. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 27] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 11. | Saragaglia D, Estour G, Nemer C, Colle PE. Revision of 33 unicompartmental knee prostheses using total knee arthroplasty: strategy and results. Int Orthop. 2009;33:969-974. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 52] [Cited by in RCA: 50] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 12. | Cregar WM, Goodloe JB, Lu Y, Gerlinger TL. Increased Operative Time Impacts Rates of Short-Term Complications After Unicompartmental Knee Arthroplasty. J Arthroplasty. 2021;36:488-494. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 21] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 13. | Ji JH, Park SE, Song IS, Kang H, Ha JY, Jeong JJ. Complications of medial unicompartmental knee arthroplasty. Clin Orthop Surg. 2014;6:365-372. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 30] [Cited by in RCA: 35] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 14. | Siedlecki C, Beaufils P, Lemaire B, Pujol N. Complications and cost of single-stage vs. two-stage bilateral unicompartmental knee arthroplasty: A case-control study. Orthop Traumatol Surg Res. 2018;104:949-953. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 26] [Article Influence: 3.7] [Reference Citation Analysis (0)] |