Published online Mar 16, 2024. doi: 10.12998/wjcc.v12.i8.1530
Peer-review started: December 21, 2023
First decision: January 10, 2024
Revised: February 7, 2024
Accepted: February 21, 2024
Article in press: February 21, 2024
Published online: March 16, 2024
Processing time: 82 Days and 3.3 Hours
The role of primary-level medical pharmacists in medical institutions in China is limited; therefore, it is necessary to explore the role of pharmacists in the process of drug treatment.
A Chinese pharmacist participated in the complete treatment of a patient with a duodenal ulcer. The rationale for drug treatment was evaluated, and adjustments were made to the antacid and anti-infective regimen, as well as the dose and frequency of administration. Body temperature, routine blood examination, and adverse drug reactions were strictly monitored. During treatment, the pharmacist recommended anti-infective therapy with ampicillin–sulbactam, which effectively controlled the infection. Additionally, the pharmacist suggested changing famotidine to lansoprazole for acid suppression and gastroprotective treatment, combined with Chinese patent medicine such as Kangfuxin Liquid. This is the first case report of a pharmacist in primary-level medical institutions adjusting drug use for patients with duodenal ulcer and pulmonary infection.
A pharmacist participated in the treatment process, provided individualized medication adjustment, and achieved good clinical results.
Core Tip: Duodenal ulcer is a common digestive disease in clinical practice. The main treatment methods are to heal the ulcer, prevent recurrence and avoid complications. For the first time, we report a case of pharmacist in a medical institution participating in the treatment process of a patient with duodenal ulcer and pulmonary infection. It is worth noting that the drug combined with Kangfuxin Liquid had a good effect, which reminds us that individualized treatment is necessary and combination with Kangfuxin Liquid is a valuable research direction.
- Citation: Gou YP, Huang Y, Chen L, Zheng W, Zheng YH. Analysis and monitoring of drug therapy in a patient with peptic ulcer complicated by infection: A case report. World J Clin Cases 2024; 12(8): 1530-1535
- URL: https://www.wjgnet.com/2307-8960/full/v12/i8/1530.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i8.1530
Peptic ulcer is a heterogeneous disease caused by an imbalance between invasive factors and mucosal defense and repair in the gastric and duodenal mucosa, often resulting from gastric acid, drugs, Helicobacter pylori (H. pylori), and other etiological factors. It is most commonly found in the stomach and duodenum[1]. Duodenal ulcer accounts for approximately 70% of cases, gastric ulcer for approximately 25%, and combination of the two for approximately 5%[2]. Currently, the main treatment strategies for duodenal ulcer include eliminating the cause, relieving symptoms, promoting ulcer healing, preventing recurrence, and avoiding complications[3]. The primary prevention strategies involve preventing H. pylori infection, and reducing the use of harmful drugs and other risk factors in order to decrease the occurrence or recurrence of ulcers[4].
Ampicillin–sulbactam is composed of sulbactam, a β-lactam inhibitor, and ampicillin, a β-lactam antibiotic, which can protect β-lactam antibiotics (ampicillin) from enzymatic destruction and enhance their antibacterial action[5]. The incidence of adverse reactions to this drug is < 10%, and there are occasional gastrointestinal symptoms such as diarrhea and nausea. In addition, it may cause liver adverse reactions such as elevated aminotransferase[6]. Lansoprazole is a proton pump inhibitor (PPI) in the class of benzimidazole compounds. The activated metabolites of lansoprazole under the influence of gastric acid can specifically inhibit the H+/K+-ATPase system in gastric parietal cells and block gastric acid secretion[7]. It is currently the drug of choice for the treatment of acid secretion. Common adverse reactions to lansoprazole include constipation, diarrhea, thirst, and abdominal distension[8]. Other adverse reactions include leukopenia, abnormal liver function, and allergic reactions. Studies have shown that older patients taking lansoprazole have a higher risk of adverse reactions[9]. Kangfuxin Liquid is often used to treats improper diet, emotional disorders, drug damage, spleen and stomach hormone deficiency, and promotes blood circulation and strengthens the spleen and kidneys by acting on the disease[10]. PPIs combined with Kangfuxin Liquid have a good therapeutic effect on ulcers accompanied by bleeding, and improve stomach pain[11]. Moreover, Kangfuxin Liquid in combination with PPIs for the treatment of gastric ulcer improved overall gastroscopy efficiency and effectiveness, and reduced adverse events and recurrence rates[12].
In this report, we describe a case in which a pharmacist advised a clinician to change his medication regimen and present the results of a 17 d analysis of medication use monitoring. After the intervention drug use program, the patient’s nocturnal abdominal pain was significantly relieved and his condition was controlled. We also review for the first time similar case reports of Kangfuxin Liquid combined with PPIs.
A 68-year-old male patient was admitted to the Gastroenterology Department of our hospital on December 23, 2022, due to abdominal pain, abdominal distension, low back pain, and poor appetite accompanied by cough and phlegm for 1 wk.
The patient had a history of gastric disease for > 30 years. A duodenal ulcer was observed by gastroscopy.
One week before admission, the patient had cough and sputum, which was slightly viscous and not easy to spit out; pain in the upper abdomen, especially under the xiphoid process; obvious abdominal distension immediately after eating, accompanied by bilateral lumbago and discomfort, fever, poor appetite, and significantly reduced food intake. After infusion treatment in the Emergency Department of our hospital, fever symptoms were relieved, but cough, sputum, and other symptoms did not improve significantly. He was admitted to the outpatient department of our hospital with abdominal pain waiting for diagnosis.
The patient had a 40-year history of smoking and smoked about 20 cigarettes a day. He had a history of drinking, 500 g a day. He denied any family history.
The patient’s temperature was 36.3 °C, heart rate was 79 bpm, respiratory rate was 21 breaths/min, blood pressure was 137/86 mmHg, and weight was 60 kg. Tenderness in the upper abdomen, especially under xiphoid process. Other measures were normal.
Routine blood examination showed that the absolute leukocyte count was 5.36 × 109/L, the percentage of neutrophilic granulocytes was 76.7%↑, the percentage of lymphocytes was 15.3%↓, and the absolute lymphocyte count was 0.82 × 109/L↓. Hepatic and renal function tests showed that alanine aminotransferase was 26 IU/L, aspartate aminotransferase was 25 IU/L, total bilirubin was 14.0 μmol/L, and creatinine was 75.3 μmol/L. 13C breath test was positive.
Contrast-enhanced computed tomography (CT) showed signs of double emphysema, bulla formation in both lungs, scattered inflammatory changes, and interstitial changes in both lungs.
The patient was discharged with a diagnosis of duodenal ulcer, chronic gastritis, pulmonary infection, acute upper res
After admission, the relevant examinations were completed, and the patient received routine and primary care. On December 24, 2022, the patient was given a famotidine injection for acid suppression and to protect the gastric mucosa, papaverine hydrochloride injection, rotundine sulfate injection to relieve symptoms and pain, amino acid and fat milk nutritional support. The main therapeutic drugs are shown in Table 1.
| Date of administration | Name of drug | Dosage |
| December 23, 2022-January 3, 2023 | Famotidine Injection | 20 mg bid ivgtt |
| January 4, 2023-January 8, 2023 | Lansoprazole for Injection | 30 mg bid ivgtt |
| December 25, 2022-December 31, 2022 | Ampicillin-Sulbactam | 1.5 mg q8h ivgtt |
| December 23, 2022-January 8, 2023 | Papaverine Hydrochloride Injection | 60 mg qd ivgtt |
| December 23, 2022-January 3, 2023 | Rotundine Sulfate Injection | 60 mg qd im |
| December 23, 2022-January 8, 2023 | Rotundine Sulfate Injection | 1 g bid po |
| December 23, 2022-January 8, 2023 | Kangfuxin Liquid | 10 mL tid po |
| December 23, 2022-January 8, 2023 | Zinc Acexamate Capsules | 0.3 g qd po |
On December 25, 2022, chest CT indicated pulmonary infection, procalcitonin (PCT) was 0.45 ng/mL, C-reactive protein was 4.2 mg/L, and the patient was given anti-infective therapy with ampicillin–sulbactam sodium injection. Sputum culture identified normal flora, routine stool examination was normal, and stool occult blood was weakly positive. The patient underwent painless gastroscopy on January 1, 2023, and the examination report showed a duodenal bulb ulcer (A1). On the same day, the patient was treated by oral administration of sucralfate suspensoid gel and zinc acexamate capsules. Famotidine was changed to lansoprazole for acid preservation. The patient’s condition improved and he was discharged from hospital on January 8, 2023. Blood biochemistry and infection-related indicators at admission are shown in Table 2.
| Project name | Result |
| WBC (/μL) | 5.36 |
| TBIL (μmol/L) | 14.0 |
| AST (IU/L) | 25 |
| ALT (IU/L) | 26 |
| NEUT (%) | 76.7 |
| Na (mmoL/L) | 141 |
| K (mmoL/L) | 4.6 |
| CR (μmol/L) | 75.3 |
| PCT (μmol/L) | 0.45 |
| CRP (mg/L) | 4.2 |
The patient had repeated symptoms of abdominal pain, abdominal distension, and lower back pain. According to the guidelines for peptic ulcer[13], middle and upper abdominal pain and acid reflux are typical symptoms of peptic ulcer disease. Treatment norms point out that for the treatment of duodenal ulcer, mainly by speeding up ulcer healing, further preventing complications and recurrence, the commonly used therapeutic drugs are mucosal protective agents, drugs to inhibit gastric acid secretion, and gastrointestinal motility drugs. PPIs are the preferred drugs, and the decrease in gastric acidity is directly related to ulcer healing. Comparison of the efficacy of the two drugs has been seen in several clinical trials. Some studies have compared the efficacy of famotidine and lansoprazole for treatment of peptic ulcer and their impact on the oxidative stress index of patients. Lansoprazole is faster-acting and more effective than famotidine for treatment of gastric ulcer[14]. Nema and Kato[15] analyzed the efficacy of PPIs and H2 receptor antagonists for treatment of gastroduodenal ulcers with sustained low-dose aspirin. In the PPI-treated group, 23 cases (88.5%) healed and three did not. In the H2 receptor antagonist group, 22 cases (84.6%) healed and four did not[15]. Therefore, after ward rounds, the pharmacist found that the patient had repeated symptoms. Considering that H2 receptor antagonists have inferior acid inhibition than PPIs, and that PPIs can reduce adverse drug reactions[16], she suggested that the clinician should replace famotidine with lansoprazole 30 mg bid, which was adopted by the physician.
It is worth noting that the therapeutic effect of Kangfuxin Liquid combined with PPI is significantly better than that of PPI monotherapy, and combination of Kangfuxin Liquid and quadruple therapy is more beneficial in reducing inflammation in patients with H. pylori-positive gastric ulcer[12]. A study on the mechanism of action showed that this may be attributed to the enhancement of neovascularization, inhibition of inflammation, and enhancement of growth factor expression[17]. The pharmacist believed that lansoprazole combined with Kangfuxin Liquid was effective in treating ulcers accompanied by bleeding, and the combination could effectively reduce gastric pain. Therefore, she suggested that the clinician add Kangfuxin Liquid to the order when the patient was admitted to hospital, and the clinician adopted the suggestion.
According to the Guidelines to Manage Community-Acquired Pneumonia, it is crucial for a patient with community-acquired pneumonia to choose the appropriate treatment site, empirical anti-infective drugs, and adjuvant therapy according to the disease severity[18]. The patient had a risk score of 1 for confusion, urea, respiratory rate, blood pressure, age 65[19]. On December 25, 2022, the sputum culture results showed normal flora, routine stool examination was normal, and stool occult blood was weakly positive. Therefore, the pharmacist recommended that the clinician use ampicillin–sulbactam.
The adverse effects of lansoprazole include constipation, diarrhea, thirst and bloating. Therefore, after the pharmacist recommended that the clinicians changed the drug on January 4, 2023, continuous medication monitoring was conducted, during which no lansoprazole-related adverse reactions were reported, and the formulation of the protocol was considered safe and effective.
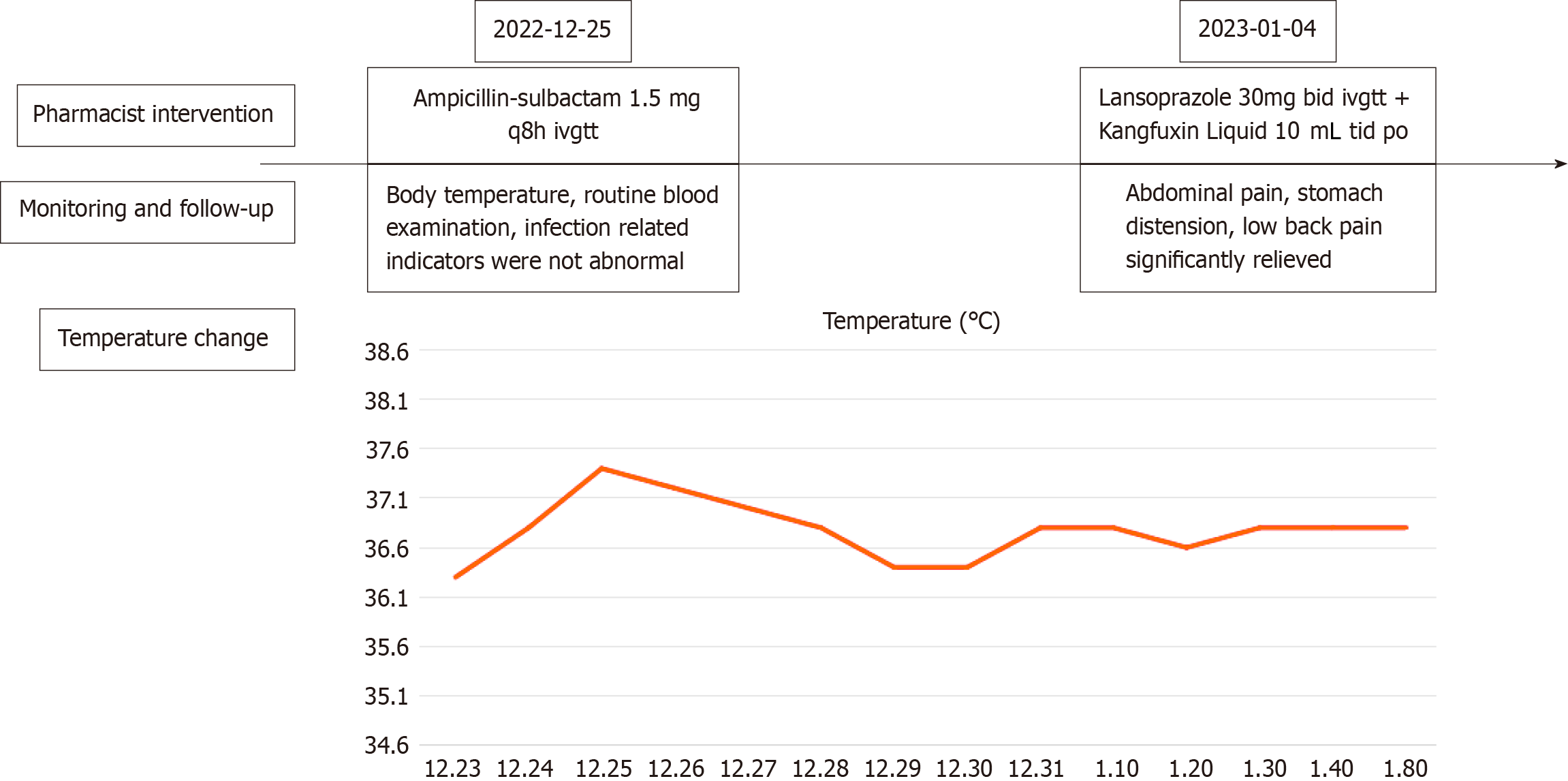
Antibiotic-associated diarrhea is most commonly caused by lincomycin, azithromycin, broad-spectrum penicillins (especially ampicillin), and second- and third-generation cephalosporins[20]. In addition, for this time-dependent antibiotic, administration according to its half-life can achieve better efficacy[21]. Therefore, in order to avoid causing diarrhea and achieve better efficacy, the dose and administration frequency of 1.5 mg q8h were selected. Pharmacists also monitored drug-related adverse reactions. Our drug monitoring showed that the patient did not have a fever during hospitalization, and there were no abnormalities in routine blood examination, PCT, and other infection indicators. The intervention and follow-up results of the pharmacist are shown in Figure 1.
It should be noted that the fecal occult blood test on day 1 of admission was weakly positive, with hemoglobin of 155 g/L and platelet count 132 × 109/L. However, after the replacement of lansoprazole and combined treatment with Kangfuxin Liquid, the fecal occult blood test on day 14 of admission was negative. Our study proves that Kangfuxin Liquid is an effective PPI combination drug and deserves further study.
There were some limitations to this study. Due to the limited medical capacity of primary medical institutions, the adjustment of drug dose based on genetic test results was not applicable in this case. In the future, we should strengthen pharmaceutical management and supervision so as to benefit more patients.
To the best of our knowledge, this is the first case report that demonstrates the important role of pharmacists in making therapeutic decisions. The experience of pharmacists can be an important aid in determining the dose of antibiotics and the use of traditional Chinese medicine such as Kangfuxin Liquid. More importantly, our case provides a clinical basis for further research on Kangfuxin Liquid combined with other drugs.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Moshref L, Saudi Arabia S-Editor: Zhang L L-Editor: A P-Editor: Zhao YQ
| 1. | Jacob TV, Doshi GM. New promising routes in peptic ulcers: Toll-like receptors and semaphorins. Endocr Metab Immune Disord Drug Targets. 2023;. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 2. | Duggan JM, Duggan AE. The possible causes of the pandemic of peptic ulcer in the late 19th and early 20th century. Med J Aust. 2006;185:667-669. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 8] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 3. | Alsahafi M, Mosli M, Alkhowaiter S, Donnellan F. Decision-Utility Analysis of Empiric Treatment Versus Test and Treat Strategies for Helicobacter pylori in Patients With Duodenal Ulcer. Value Health Reg Issues. 2024;39:1-5. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 4. | Talebi Bezmin Abadi A. Helicobacter pylori treatment: New perspectives using current experience. J Glob Antimicrob Resist. 2017;8:123-130. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 32] [Cited by in RCA: 26] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 5. | Fong ZV, McMillan MT, Marchegiani G, Sahora K, Malleo G, De Pastena M, Loehrer AP, Lee GC, Ferrone CR, Chang DC, Hutter MM, Drebin JA, Bassi C, Lillemoe KD, Vollmer CM, Fernández-Del Castillo C. Discordance Between Perioperative Antibiotic Prophylaxis and Wound Infection Cultures in Patients Undergoing Pancreaticoduodenectomy. JAMA Surg. 2016;151:432-439. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 72] [Cited by in RCA: 98] [Article Influence: 12.3] [Reference Citation Analysis (0)] |
| 6. | LiverTox: Clinical and Research Information on Drug-Induced Liver Injury [Internet]. Bethesda (MD): National Institute of Diabetes and Digestive and Kidney Diseases; 2012– . [PubMed] |
| 7. | Garnett WR. Lansoprazole: a proton pump inhibitor. Ann Pharmacother. 1996;30:1425-1436. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 11] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 8. | Debsharma S, Pramanik S, Bindu S, Mazumder S, Das T, Saha D, De R, Nag S, Banerjee C, Siddiqui AA, Ghosh Z, Bandyopadhyay U. Honokiol, an inducer of sirtuin-3, protects against non-steroidal anti-inflammatory drug-induced gastric mucosal mitochondrial pathology, apoptosis and inflammatory tissue injury. Br J Pharmacol. 2023;180:2317-2340. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 12] [Reference Citation Analysis (0)] |
| 9. | Dipasquale V, Cicala G, Laganà F, Cutroneo P, Trimarchi G, Spina E, Romano C. Spontaneous reporting of adverse reactions related to proton pump inhibitors. Dig Liver Dis. 2023;55:595-600. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Reference Citation Analysis (0)] |
| 10. | Sun H, Yang C, Liu X, Liang J, Geng H. Effectiveness of Negative Pressure Wound Therapy of Diabetic Foot Ulcers Using Periplaneta Americana (Kangfuxin Liquid) Irrigation. Int J Low Extrem Wounds. 2023;15347346231176917. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Lin M, Zhang S, Zhang M, Shi J, Zhang C, Luo R, You J, Sun J, Zhang J, Gao F. Therapeutic efficacy and safety of Kangfuxin in combination with rabeprazole in the treatment of peptic ulcer: A systematic review and meta-analysis. Medicine (Baltimore). 2020;99:e23103. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 4] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 12. | Zou JB, Zhang XF, Shi YJ, Tai J, Wang Y, Liang YL, Wang F, Cheng JX, Wang J, Guo DY. Therapeutic Efficacy of Kangfuxin Liquid Combined with PPIs in Gastric Ulcer. Evid Based Complement Alternat Med. 2019;2019:1324969. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 12] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 13. | Kamada T, Satoh K, Itoh T, Ito M, Iwamoto J, Okimoto T, Kanno T, Sugimoto M, Chiba T, Nomura S, Mieda M, Hiraishi H, Yoshino J, Takagi A, Watanabe S, Koike K. Evidence-based clinical practice guidelines for peptic ulcer disease 2020. J Gastroenterol. 2021;56:303-322. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 149] [Cited by in RCA: 142] [Article Influence: 35.5] [Reference Citation Analysis (0)] |
| 14. | Okai T, Sawabu N, Songür Y, Motoo Y, Watanabe H. Comparison of lansoprazole and famotidine for gastric ulcer by endoscopic ultrasonography: a preliminary trial. J Clin Gastroenterol. 1995;20 Suppl 2:S32-S35. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 15. | Nema H, Kato M. Comparative study of therapeutic effects of PPI and H2RA on ulcers during continuous aspirin therapy. World J Gastroenterol. 2010;16:5342-5346. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 13] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 16. | Begg M, Tarhuni M, N Fotso M, Gonzalez NA, Sanivarapu RR, Osman U, Latha Kumar A, Sadagopan A, Mahmoud A, Khan S. Comparing the Safety and Efficacy of Proton Pump Inhibitors and Histamine-2 Receptor Antagonists in the Management of Patients With Peptic Ulcer Disease: A Systematic Review. Cureus. 2023;15:e44341. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 8] [Reference Citation Analysis (0)] |
| 17. | Tian M, Dong J, Wang Z, Lu S, Geng F. The effects and mechanism of Kangfuxin on improving healing quality and preventing recurrence of gastric ulcer. Biomed Pharmacother. 2021;138:111513. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 17] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 18. | Wunderink RG. Guidelines to Manage Community-Acquired Pneumonia. Clin Chest Med. 2018;39:723-731. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 13] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 19. | Patel S. Calculated decisions: CURB-65 score for pneumonia severity. Emerg Med Pract. 2021;23:CD1-CD2. [PubMed] |
| 20. | Mekonnen SA, Merenstein D, Fraser CM, Marco ML. Molecular mechanisms of probiotic prevention of antibiotic-associated diarrhea. Curr Opin Biotechnol. 2020;61:226-234. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 45] [Cited by in RCA: 122] [Article Influence: 24.4] [Reference Citation Analysis (0)] |
| 21. | Owens RC Jr, Ambrose PG. Antimicrobial stewardship and the role of pharmacokinetics-pharmacodynamics in the modern antibiotic era. Diagn Microbiol Infect Dis. 2007;57:77S-83S. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 30] [Article Influence: 1.7] [Reference Citation Analysis (0)] |