Published online Mar 16, 2024. doi: 10.12998/wjcc.v12.i8.1497
Peer-review started: December 12, 2023
First decision: December 21, 2023
Revised: January 7, 2024
Accepted: February 18, 2024
Article in press: February 18, 202
Published online: March 16, 2024
Processing time: 90 Days and 13.6 Hours
Patients rarely develop complicated infections in thyroid cysts. Here, we describe a patient with chronic infected unilateral giant thyroid cyst related to diabetes mellitus (DM).
A 66-year-old male was admitted due to an evident neck lump for 5 d after approximately 40 years of gradually progressive neck mass and 7 years of DM. Doppler ultrasound and computed tomography scan showed a giant lump in the left thyroid gland lobe. He was diagnosed with a large thyroid nodule complicated by tracheal dislocation and had surgical indications. Surgical exploration revealed evident inflammatory edema and exudation between the left anterior neck muscles, the nodule and glandular tissue. Fortunately, inflammatory lesions did not affect major neck vessels. Finally, a left partial thyroidectomy was performed. Macroscopic observation showed that the cystic thyroid mass consisted of extensive cystic wall calcification and was rich in massive rough sand-like calculi content and purulent matter. Postoperative pathology confirmed benign thyroid cyst with chronic infection.
The progression of this chronic infectious unilateral giant thyroid cyst may have been related to DM, and identifying blood vessels involvement can prevent serious complications during operation.
Core Tip: When encountering a huge thyroid mass with coinfection in the clinical setting, comprehensive examination is required to confirm the cause of its formation and subsequent individualized treatment strategies. With carefully applied surgical procedures, complications such as severe intraoperative and postoperative hemorrhage can be avoided or reduced. This report may provide clinicians with perspectives for the diagnosis and treatment of giant thyroid cysts complicated by infection under diabetes mellitus conditions.
- Citation: Liu JB, Zhang SL, Jiang WL, Sun HK, Yang HC. Chronic infectious unilateral giant thyroid cyst related to diabetes mellitus: A case report. World J Clin Cases 2024; 12(8): 1497-1503
- URL: https://www.wjgnet.com/2307-8960/full/v12/i8/1497.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i8.1497
Benign thyroid cysts usually do not need to receive therapeutic intervention; however, if thyroid cysts grow too large and cause compressive symptoms, such as dysphagia, dyspnea, and local discomfort, therapeutic intervention is required[1]. Because the thyroid gland has a complete capsule, rich blood supply, good lymphatic drainage, and high iodine concentration as well as an association with other special physiological structures, the thyroid gland does not easily develop infection[2]. When the patient’s local and systemic ability to fight infection is reduced, thyroid infection is prone to occur. A systematic review reported that diabetes mellitus (DM) causes 13% of bacterial thyroid abscesses[2]. DM may make the thyroid gland relatively susceptible to infection by increasing the permeability of connective tissue and the activity of hyaluronidase, subsequently allowing bacteria and toxins to pass easily through the tissue and facilitating the spread of infection[3]. However, based on the current published research literature and case reports, it is difficult to conclude that DM results in infection of the thyroid nodule with intact physical capsule and immunity. Therefore, there is a need to explore the specific mechanism and collect more typical cases in support of this hypothesis. Herein, this report presents a special case of a unilateral giant cystic thyroid mass with repeated chronic infection attributed to accompanying DM.
A 66-year-old male was admitted due to an evident neck lump for 5 d after approximately 40 years of gradually progressive neck mass.
On August 24, 2021, the patient experienced a 40-year history of a slowly progressive neck mass accompanied by gradually aggravated dyspnea and dysphagia. Due to sudden rapid enlargement for 5 d, he was admitted to our hospital thyroid and breast surgery department for diagnosis and treatment and was not treated before admission.
The patient had a 7-year history of type 2 DM and usually took metformin for treatment; his blood glucose was well controlled. The patient also had a history of left humeral fracture 20 years prior, underwent surgery and recovered well after treatment.
The patient had no history of family illness.
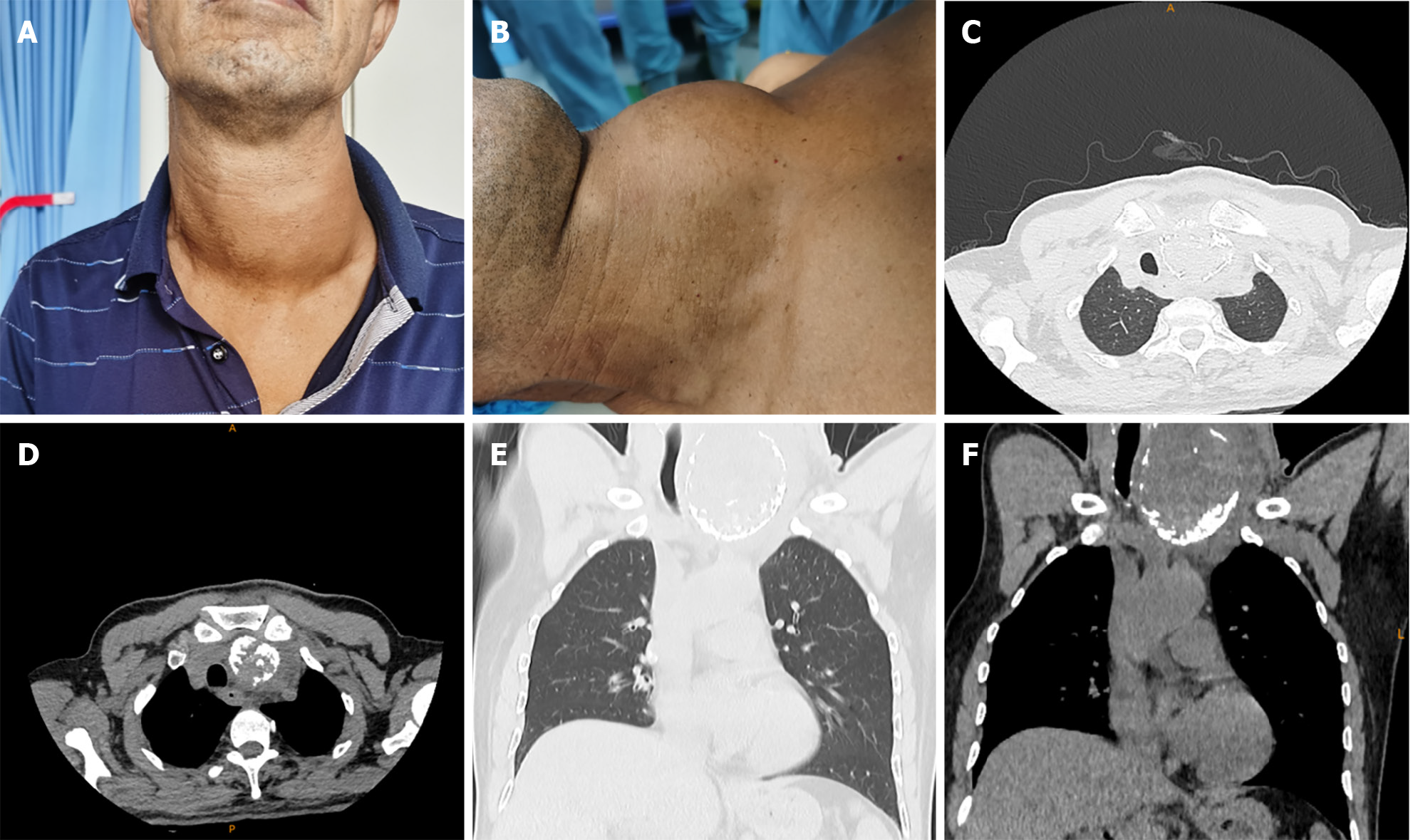
A third-degree enlargement of the left lateral lobe of the thyroid; the enlargement was palpated as an approximately 11 cm (upper and lower diameter) × 9 cm (transverse diameter) × 6 cm (anteroposterior diameter) tough thyroid mass of unclear contour that exhibited very limited movement up and down with deglutition. The trachea deviated obviously to the right and backward (Figure 1A and B). Due to the large mass, neck movement was also limited.
Preadmission DM follow-up visit in June 2021 showed that hemoglobin A1c (HbA1c) was 7%. Routine blood examination showed hemoglobin 92 g/L and red blood cells 3.2 × 1012/L, and the other indexes were basically normal. Abnormal blood biochemistry results included albumin 31.4 g/L and glucose 8.51 mmol/L. Thyroid function tests showed thyrotropin 0.48 μIU/mL, and the other indexes were normal.
Preadmission ultrasonography in June 2021 revealed that a hypoechoic solid nodule was in the lower left lobe of the thyroid gland. After hospitalization, preoperative neck and chest plain and contrast enhanced computed tomography (CT) scans showed that in abnormally enlarged left lobe of the thyroid gland, a mixed-density mass (9.0 cm × 6.7 cm × 6.5 cm) containing extensively arc-shaped edge calcification and patchy calcification shadows within the mass, with mild to moderate inhomogeneous enhancement and blurred borders, were observed. The trachea, laryngeal cavity, esophagus, and right cervical blood vessels were compressed and shifted to the right side posteriorly, while the left common carotid artery and internal jugular vein and other surrounding tissues were obviously compressed and moved backward to the left lower side of the left thyroid gland, but no evidence of vascular involvement (Figure 1C-F). Additionally, multiple enhanced enlarged lymph nodes were seen in the upper mediastinum and left neck.
The patient was diagnosed with the following: (1) (Huge) nontoxic single thyroid nodule; (2) Dislocation of the trachea; (3) Tracheal collapse; (4) Esophageal compression; (5) Type 2 DM; (6) Mild iron deficiency anemia; (7) Hypoproteinemia; (8) Subclinical hyperthyroidism; and (9) Personal history of humerus fracture surgery (left) (ICD-11). According to medical history, clinical manifestations, and CT features, the patient necessitated diagnostic differentiation between a malignant thyroid tumor and other occupied lesions of the thyroid gland.
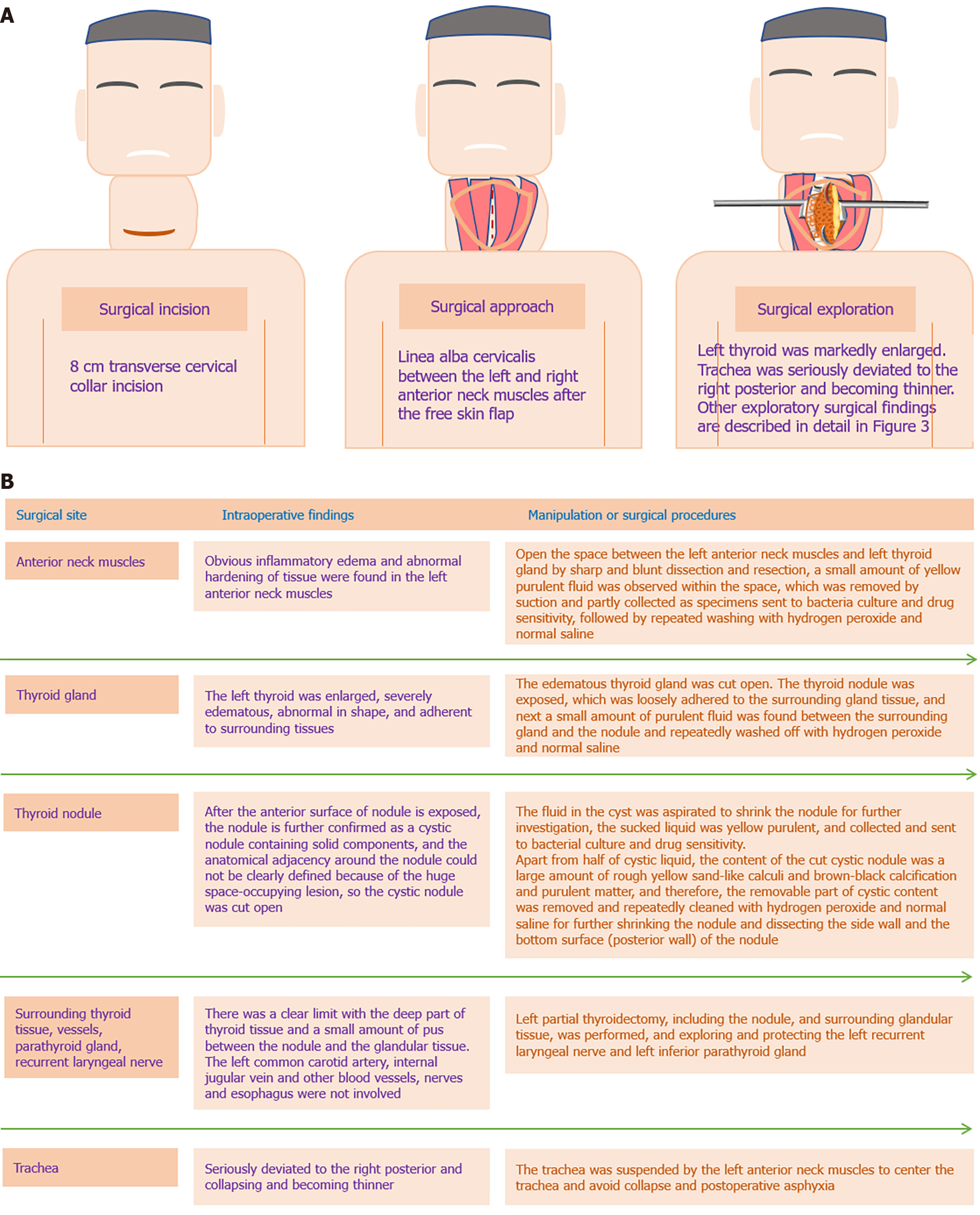
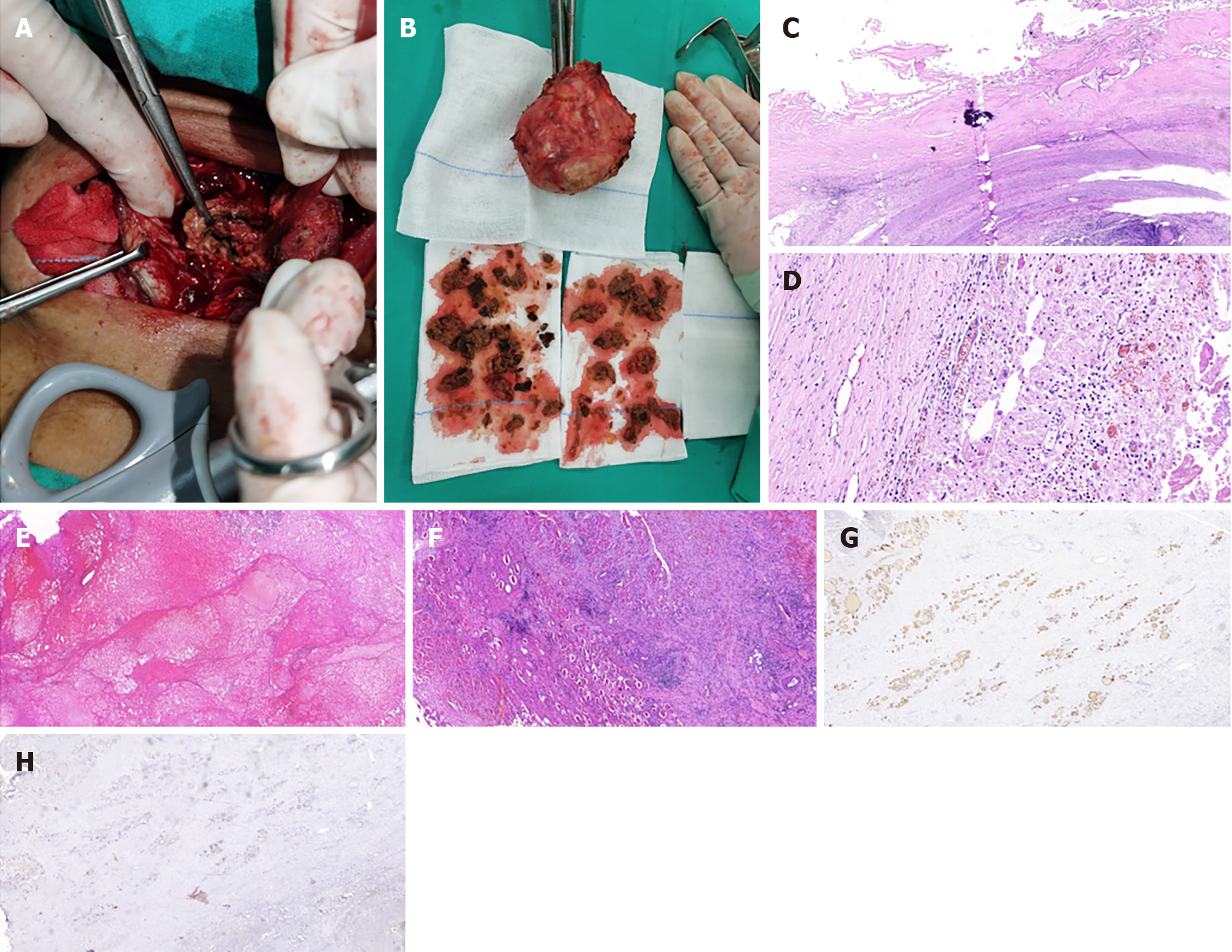
To treat and differentiate the diseases described in the diagnostic results, exploration and resection of the left thyroid nodule (and surrounding glands) were planned under general anesthesia. Accordingly, the indications for surgery were as follows: (1) Huge thyroid nodule; (2) Symptoms of tracheal and esophageal compression; (3) Restricted neck movement; and (4) Suspected thyroid malignancy. On August 25, 2021, exploration and resection of the left thyroid nodule and small amounts of surrounding gland tissues were performed under general anesthesia. The surgical procedure and intraoperative findings are described in detail in Figure 2A and B. After removal, the nodule was carefully examined by inspection and palpation. Macroscopic and palpation characteristics of the removed nodule were as follows: Size 10.0 cm × 9.0 cm × 8.0 cm; a thick wall cyst lesion containing solid cystic contents with smooth surface and clear separation from surrounding gland tissue; and a feeling of crushing eggshells during the palpation examination. There was massive necrotic tissue containing calcification within the thyroid cyst (Figure 3A and B). Additionally, intraoperative frozen section assessment pathological examination ruled out malignant lesion (pathological findings similar to postoperative pathological assessment) (Figure 3C-F). The operation went smoothly. After the operation, tracheal intubation was maintained until the patient was fully awake and spontaneous breathing movement was recovered.
The microbial culture of the submitted purulent matter failed to grow pathogenic bacteria and fungi. Postoperative routine pathological examination and immunohistochemistry (IHC) results confirmed that the nodule was a benign tumor (Figure 3G and H). The patient recovered uneventfully without postoperative complications. The symptoms of dyspnea and dysphagia were greatly relieved after the operation. During the 2 years of regular outpatient reexamination or telephone follow-up (to August 31, 2023), the patient was able to breathe and swallow easily, no new goiter was found, thyroid function was normal, and the HbA1c level improved (6%) after periodic insulin treatment; thus, the patient was not administered thyroid hormone therapy.
Thyroid infection is an uncommon but serious infectious disease that may have underlying anatomical or iatrogenic causes; if left untreated, it can be life-threatening[4]. Patients with preexisting structural abnormalities of the thyroid gland (e.g., multinodular goiter, malignancy) may be more prone to thyroid infection[5]. Diseases affecting systemic immunity including tuberculosis[6], DM[7], and human immunodeficiency virus infection[8] could increase the risk of thyroid abscess. To the best of our knowledge, there have been no reports of infected large thyroid cysts combined with DM.
Most cases of thyroid cysts combined with infection reported in the literature have a clear cause of infection. Sun et al[9] reported a case of thyroid cyst after fine needle aspiration biopsy (FNAB) complicated by anaerobic bacterial thyroid abscess, surmising that the abscess could have been caused by bacterial contamination from the FNAB process. Igarashi et al[10] reported a case of acute purulent infection of a thyroid cyst in a hemodialysis patient, speculating that the infection was closely related to bacterial contamination and low systemic immunity during hemodialysis. DM can increase the risk of infection[11]. In addition to many infections being more common and more severe among people with diabetes, certain infections occur almost exclusively in patients with DM[12]. Thyroid infections are less common in diabetic patients. Liu et al[13] reported a case of thyroid abscess as the first symptom of diabetes, suggesting that DM played a key role in thyroid infection. The patient described in this report had no previous history of thyroid puncture or vascular invasive operation, so there was no clear extrinsic cause of thyroid cyst infection in this case. Therefore, it is speculated that the patient’s thyroid cyst infection may have been related to the influence of DM on systemic and local immunity. Moreover, repeated chronic infection consumption in thyroid cyst due to DM could be involved in causing patient’s mild anemia and hypoproteinemia, which also in turn aggravated systemic immunity of the patient.
Compared with the above-mentioned cases, this case presented more complicated infections and underwent difficult differential diagnosis. According to medical history, clinical manifestations, and CT features, the patient was initially suspected of having a malignant thyroid tumor. The collected findings demonstrated that surgical exploration should be performed and that there were no absolute contradictions to thyroid surgery. Finally, intraoperative pathology ruled out that the nodule was a malignant tumor, and postoperative pathological and IHC results further confirmed that the nodule was a benign cystic-solid lesion complicated with chronic infection. The reasons for the difference between the suspected malignant imaging findings and the benign histology, making preoperative diagnosis difficult, may be that the patient had a long history of progressive thyroid tumors, accompanied by repeated chronic infection. As a result, there were special calcification changes, fibrosis of the cyst wall, and development of extensive necrotic cystic content as well as enlargement of surrounding lymph nodes.
Because the patient with this special condition had a 40-year history of progressive thyroid mass, understanding the complexity of the disease progression process may be interesting and have enlightening value. After detailed inquiry of the medical history, the family members of the patient provided front-view photos of the patient in 2008 and 2018, and side-view photos in 2021 before hospitalization (data not shown). According to the photos, the thyroid tumor did not affect the appearance of the neck in 2008. In 2018, however, a local bulge was seen on the left side of the neck, but the thyroid notch was still in the middle, suggesting that the thyroid tumor had not yet compressed the trachea and caused considerable deviation in the trachea. Five days before admission in 2021, the neck tumor was substantially enlarged compared with the 2018 photo, but the frontal contour of the neck slightly exceeded the line connecting the thyroid notch and the upper edge of the sternal manubrium. However, during the 5 d before hospitalization, the neck mass had further enlarged, and upon admission, it clearly extended beyond the line connecting the thyroid notch and the upper edge of the sternal manubrium.
According to a 7-year medical history of DM, the occurrence of thyroid nodules and cystic degeneration may not be related to DM in this patient. However, after the patient developed DM, DM may have influenced the progression of the thyroid nodule and the onset of spontaneous infection. At first, the infection remained within the cyst, causing massive fibrosis, necrosis deposition and calcification of the cyst wall and cyst content. Furthermore, the reduced systemic and local immunity due to DM caused the spread of infection, resulting in infection of glandular tissue, anterior neck muscles, and other soft tissue outside the cyst. Finally, the neck mass was greatly enlarged within 5 d before admission, which may be considered the acute onset of combined infection inside and outside the cyst. However, the patient had no obvious signs of infection, possibly due to the limitation of infection caused by the pus wrapping in the cyst and the fibrous septum formed by repeated infection outside the cyst. Therefore, DM is closely related to the infection and later evolution of the thyroid nodule in this case. Thus, the possibility of infection should not be ignored in thyroid nodule patients with DM, and the occurrence of thyroid infection should be identified early to prevent misdiagnosis and delay in treatment.
Infected cysts of the thyroid should be differentiated from other common thyroid disorders such as nodular goiter, thyroid adenoma, and cystic degeneration of thyroid malignancy. For patients who need surgery, a complete examination must be carried out before the operation, and the morphological situation must be carefully analyzed to understand whether the thyroid lesion has involved important tissues such as the trachea and adjacent blood vessels. During the operation, the nodule should be carefully separated and dissected to avoid damage to the surrounding blood vessels and recurrent laryngeal nerves and to protect the parathyroid glands. For thyroid cysts with tracheal compression, the trachea should be suspended and fixed to the anterior neck muscles to avoid asphyxiation caused by tracheal collapse at the end of surgery. Regardless of whether unilateral or bilateral giant cystic tumors of the thyroid are subjected to surgery, thyroid function should be routinely tested to avoid postoperative hypothyroidism[14].
In this case, the continuous enlargement of the thyroid cyst and the accumulation of infected content in the cyst may have been caused by repeated chronic infection due to comorbid DM. However, the sudden enlargement was likely related to an acute exacerbation of infection in and around the cyst. When encountering such a huge thyroid mass with coinfection in the clinical setting, comprehensive examination is required to confirm the diagnosis and treatment. With carefully applied surgical procedures, complications such as severe intraoperative and postoperative hemorrhage can be avoided or reduced. This report may provide clinicians with perspectives for the diagnosis and treatment of giant thyroid cysts complicated by infection under DM conditions.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Cabezuelo AS, Spain; Ciarambino T, Italy S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Yu HG
| 1. | Stan MN, Castro MR. Nonsurgical treatment of thyroid cysts - "seal them up". Endocr Pract. 2020;26:573-575. [PubMed] [DOI] [Full Text] |
| 2. | Lafontaine N, Learoyd D, Farrel S, Wong R. Suppurative thyroiditis: Systematic review and clinical guidance. Clin Endocrinol (Oxf). 2021;95:253-264. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 3. | Ikegami-Kawai M, Okuda R, Nemoto T, Inada N, Takahashi T. Enhanced activity of serum and urinary hyaluronidases in streptozotocin-induced diabetic Wistar and GK rats. Glycobiology. 2004;14:65-72. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 28] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 4. | Falhammar H, Wallin G, Calissendorff J. Acute suppurative thyroiditis with thyroid abscess in adults: clinical presentation, treatment and outcomes. BMC Endocr Disord. 2019;19:130. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 24] [Cited by in RCA: 33] [Article Influence: 5.5] [Reference Citation Analysis (0)] |
| 5. | Paes JE, Burman KD, Cohen J, Franklyn J, McHenry CR, Shoham S, Kloos RT. Acute bacterial suppurative thyroiditis: a clinical review and expert opinion. Thyroid. 2010;20:247-255. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 160] [Cited by in RCA: 106] [Article Influence: 7.1] [Reference Citation Analysis (0)] |
| 6. | Nieuwland Y, Tan KY, Elte JW. Miliary tuberculosis presenting with thyrotoxicosis. Postgrad Med J. 1992;68:677-679. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 21] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 7. | Li CC, Wang CH, Tsan KW. Graves' disease and diabetes mellitus associated with acute suppurative thyroiditis: a case report. Zhonghua Yi Xue Za Zhi (Taipei). 1997;59:59-64. [PubMed] |
| 8. | Lecuit M, Caumes E, Bricaire F, Gatineau M, Ménégaux F, Gentilini M. Acute suppurative Salmonella enteritidis thyroiditis associated with thyrotoxicosis in a patient infected with the human immunodeficiency virus. Clin Infect Dis. 1995;20:196. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 12] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 9. | Sun JH, Chang HY, Chen KW, Lin KD, Lin JD, Hsueh C. Anaerobic thyroid abscess from a thyroid cyst after fine-needle aspiration. Head Neck. 2002;24:84-86. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 21] [Cited by in RCA: 18] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Igarashi H, Yoshino H, Hijikata M, Kumashiro N, Ando Y, Uchino H, Tsuboi K, Hirose T. Acute suppurative thyroiditis in infected thyroid cyst in an adult patient under hemodialysis. Clin Case Rep. 2017;5:570-573. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 11. | Carey IM, Critchley JA, DeWilde S, Harris T, Hosking FJ, Cook DG. Risk of Infection in Type 1 and Type 2 Diabetes Compared With the General Population: A Matched Cohort Study. Diabetes Care. 2018;41:513-521. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 272] [Cited by in RCA: 419] [Article Influence: 59.9] [Reference Citation Analysis (0)] |
| 12. | Joshi N, Caputo GM, Weitekamp MR, Karchmer AW. Infections in patients with diabetes mellitus. N Engl J Med. 1999;341:1906-1912. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 672] [Cited by in RCA: 709] [Article Influence: 27.3] [Reference Citation Analysis (0)] |
| 13. | Liu Y, Yu S, Ren X, Qiao Y, Sun G. Klebsiella pneumoniae thyroid abscess complicated with esophagitis in a woman with newly diagnosed diabetes mellitus: A case report. J Diabetes Investig. 2016;7:127-129. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Jariyawattanarat V, Chantharit P, Sritara C, Chansoon T, Sriphrapradang C. A case of acute suppurative thyroiditis caused by Streptococcus suis infection. Germs. 2021;11:592-596. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |