Published online Mar 16, 2024. doi: 10.12998/wjcc.v12.i8.1461
Peer-review started: November 19, 2023
First decision: December 27, 2023
Revised: January 6, 2024
Accepted: February 18, 2024
Article in press: February 18, 2024
Published online: March 16, 2024
Processing time: 110 Days and 17.1 Hours
Appendiceal intussusception is a pathological condition in which the appendix is inverted into the cecum, which may cause symptoms that resemble those of other gastrointestinal disorders and may induce intestinal obstruction. The rarity of this case presentation is the co-occurrence of appendiceal intussusception and cecal adenocarcinoma, a combination that to our knowledge has not previously been reported in the medical literature. This case provides new insights into the complexities of diagnosing and managing overlapping pathologies.
A 25-year-old woman presented with persistent periumbilical pain and bloody stools. An initial biopsy showed cecal cancer; however, subsequent colonoscopy and computed tomography findings raised the suspicion of appendiceal intussusception, which was later confirmed postoperatively. This unique case was characterized by a combination of intussusception and adenocarcinoma of the cecum. The intervention included a laparoscopic right hemicolectomy, which led to the histopathological diagnosis of mucinous adenocarcinoma with appendiceal intussusception. The patient recovered well postoperatively and was advised to initiate adjuvant chemotherapy. This case highlights not only the importance of considering appendiceal intussusception in the differential diagnosis, but also the possibility of appendicitis and the atypical presentation of neoplastic lesions.
Physicians should consider the possibility of appendiceal intussusception in cases of atypical appendicitis, particularly when associated with neoplastic presenta
Core tip: This report presents a unique case of appendiceal intussusception associated with cecal adenocarcinoma, which has rarely been reported in medical literature. This case highlights the diagnostic challenges posed by unconventional polyps and the complexity of the radiological findings in which malignancies and signs of intussusception coexist. This report emphasizes the need for thorough clinical and radiological evaluation and illustrates the potential of integrating various diagnostic tools to achieve accuracy. In addition, cecal tumors may extend into the appendix, complicating the presentation of standard appendiceal intussusception and requiring careful review of preoperative imaging to guide surgical intervention and subsequent treatment strategies.
- Citation: Long Y, Xiang YN, Huang F, Xu L, Li XY, Zhen YH. Appendiceal intussusception complicated by adenocarcinoma of the cecum: A case report. World J Clin Cases 2024; 12(8): 1461-1466
- URL: https://www.wjgnet.com/2307-8960/full/v12/i8/1461.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i8.1461
Intussusception is a rare clinical condition in which the appendix prolapses into the cecum, which may lead to intestinal obstruction, requiring prompt diagnosis and intervention. This case report documents an occurrence of appendiceal intussusception with cecal adenocarcinoma, a manifestation rarely described in the available medical literature. This report aimed to highlight the diagnostic challenges posed by concurrent pathological conditions and discuss the complexities of distinguishing benign and malignant lesions in preoperative evaluations.
In preparing this case report, we critically reviewed the literature using databases such as PubMed. Search terms included “intussusception”, “cecal adenocarcinoma” and “intussusception with malignancy”. Despite extensive investigation, there was a clear absence of reports of similar cases in which these circumstances occurred simultaneously, supporting the merits and novelty of this case. Therefore, this report aimed to increase the body of knowledge of this manifestation by detailing the diagnostic process and surgical findings that led to the discovery of this rare clinical condition.
Herein, we described a patient with recurrent abdominal pain and gastrointestinal bleeding that prompted a referral for suspected cecal cancer. This case highlights the urgent need to combine radiological signs and clinical symptoms in developing a comprehensive diagnostic approach. These clinical problems are addressed: the complexity of managing intussusception symptoms and signs of malignancy and the subsequent implications for surgical decisions. Based on our experiences in this case, we hypothesized that vigilance and multifaceted diagnostic strategies are essential for identifying such rare and complex cases, potentially improving patient outcomes through tailored interventions.
A 25-year-old woman presented with persistent abdominal pain and bloody stools. The patient had experienced recurrent periumbilical pain for 20 d, accompanied by bloody stools, diarrhea, nausea, and vomiting. During colonoscopy at another hospital, lesions were found in the ileocecal area, suggesting cecal cancer.
The patient had no pertinent current medical history.
The patient had no family history of intestinal disease.
The patient had no pertinent personal or family history.
On examination, the patient was visibly distressed by abdominal pain. The most striking finding on physical examination was marked tenderness of the right lower quadrant of the abdomen. No visible or palpable mass was noted, and there were no signs of peritoneal irritation such as rebound tenderness or guarding.
Laboratory tests showed a red blood cell concentration of 2.72 × 1012/L and a hemoglobin concentration of 78 g/L; there were no other significant abnormalities.
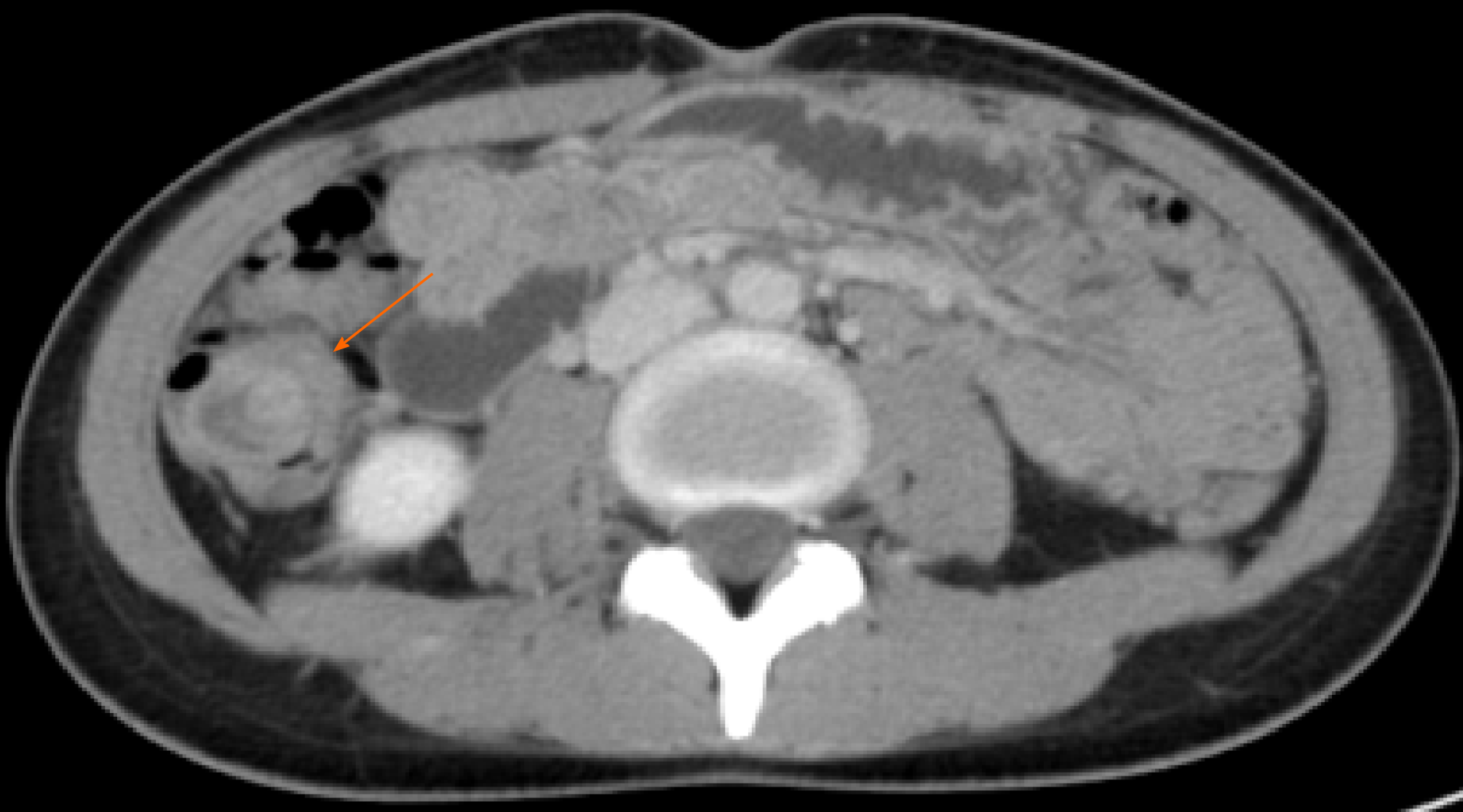
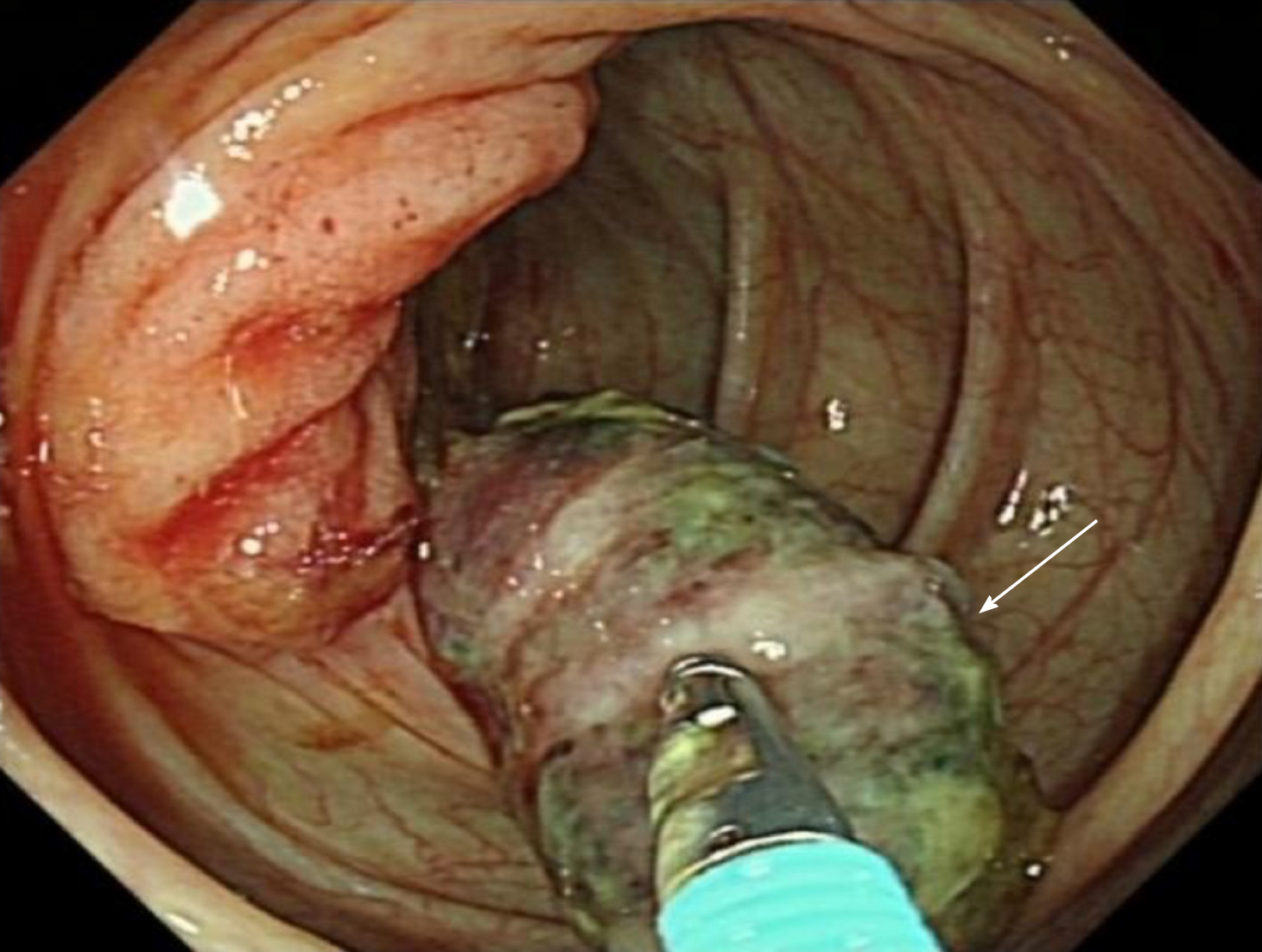
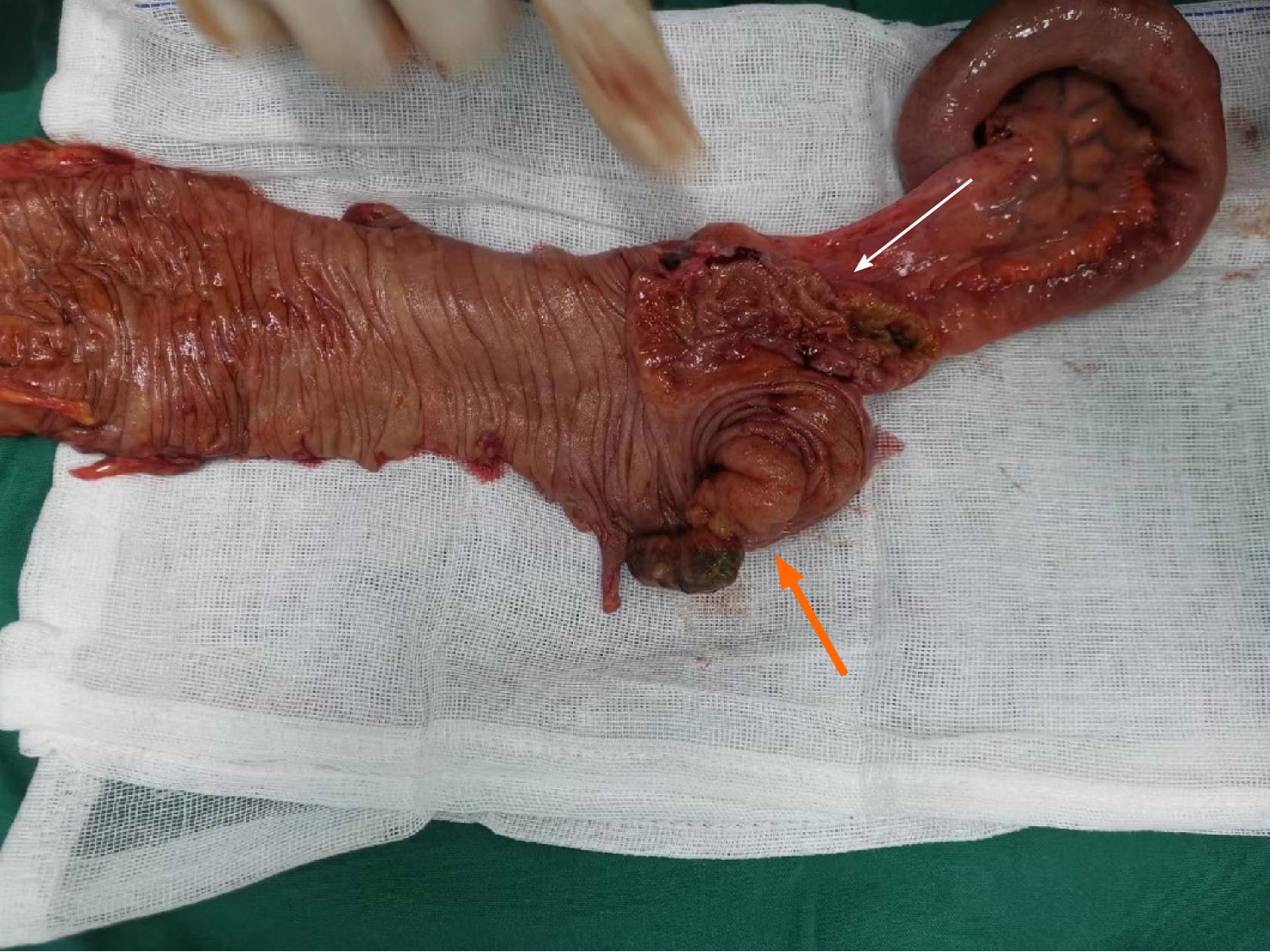
A colonoscopy was performed at the referral hospital ten days prior to admission at our institution; that colonoscopy revealed a lesion in the ileocecal region. A biopsy was performed which revealed high-grade adenomatous dysplasia with focal malignant transformation, and the initial diagnosis was cecal cancer. After the patient was admitted to our institution, we performed an abdominal computed tomography (CT) with contrast, which showed significant thickening of the ileocecal wall. However, the appendix was not clearly visible, and the diagnosis of intussusception was ultimately missed. Retrospective analysis of the CT images revealed target signs, suggesting intussusception (Figure 1). A subsequent colonoscopy performed at our institution revealed a "finger-shaped" tumor in the cecal lumen (Figure 2). The patient underwent a biopsy of the tumor and the adjacent mucosa of the cecal wall. The pathology report of the tumor was initially misinterpreted as a hyperplastic polyp. Postoperatively, an examination led to the identification of an intussusception ischemic appendix (Figure 3). Simultaneously, a biopsy of the mucosa adjacent to the cecum wall confirmed the presence of a mucinous adenocarcinoma.
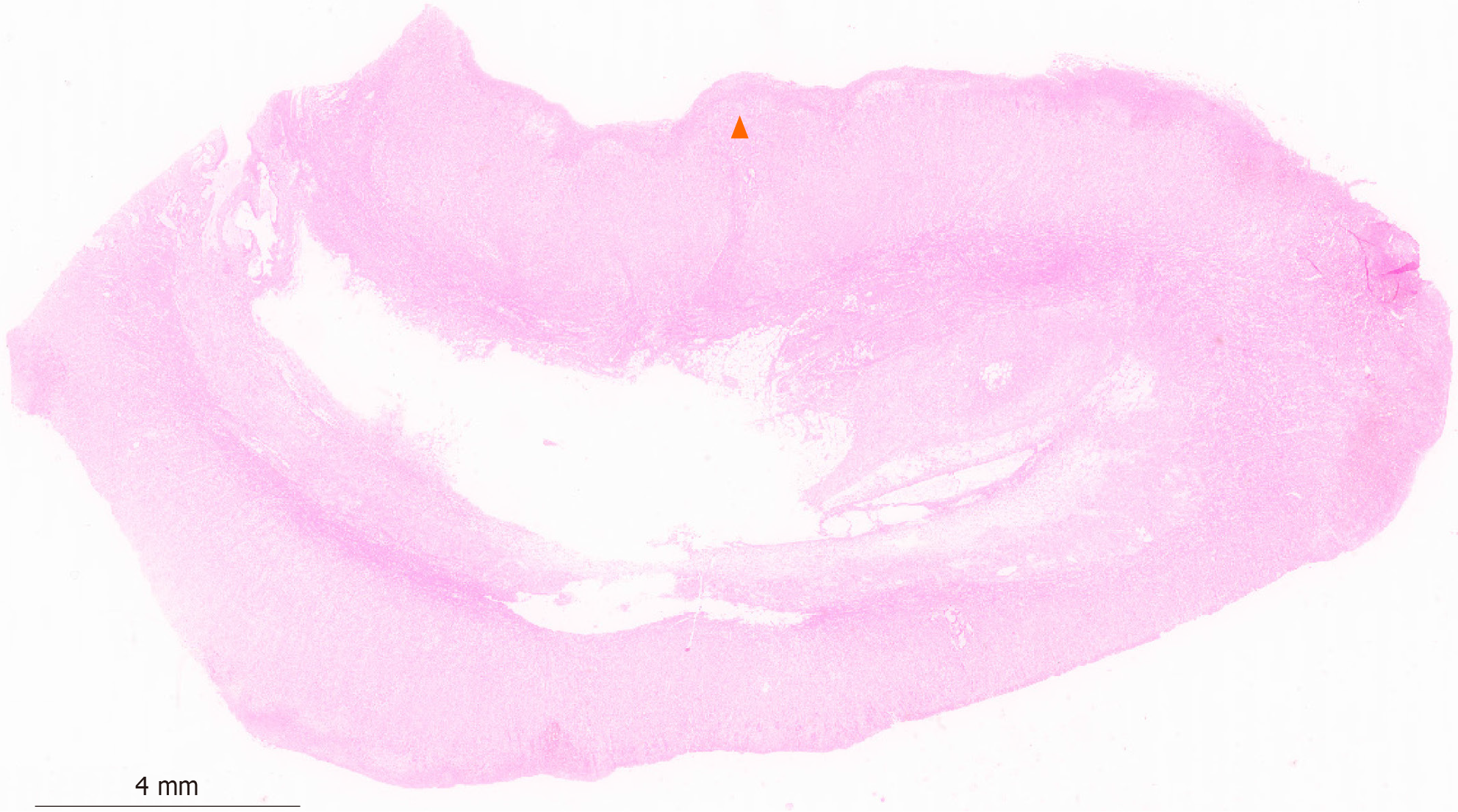
A diagnosis of appendiceal cecal intussusception with cecal mucinous adenocarcinoma was confirmed by postoperative histopathological examination. Tumor invasion into the muscle and subserous layers such as that seen in this case indicates locally advanced cancer, classified as pT3N1M0 or pIII. Phase A (Figure 4).
The patient underwent laparoscopic right hemicolectomy on the fifth day after admission. Surgical procedures included resection of the involved ileocecal region and lymph node dissection. A total of 15 lymph nodes were collected, three of which tested positive for lymph node metastases.
The patient recovered smoothly and was discharged from the hospital seven days after surgery. Adjuvant chemotherapy was recommended and scheduled to be initiated in the oncology department three to four weeks after discharge.
Appendiceal intussusception was first discovered by McKidd in 1858, during an autopsy of a seven-year-old boy. The patient had experienced abdominal colic symptoms two months before death, and autopsy results revealed appendiceal intussusception caused by ascaris[1]. Collins et al[2] reviewed 71000 pathological specimens in 1963 and found only seven cases of appendiceal intussusception, with an incidence rate of only 0.01%. Although appendiceal intussusception can occur at any age, it is predominantly observed in adults, with the risk in women being twice that in men[3]. Reaching a definitive diagnosis of appendiceal intussusception was challenging in our patient. Initially, the patient was diagnosed with cecal cancer. However, we later discovered the coexistence of appendiceal and cecal intussusceptions, which altered our understanding of the case. Appendiceal cecal intussusception, caused by prolapse and rotation between the appendix and intestinal wall, can lead to intestinal obstruction. Symptoms such as abdominal pain, diarrhea, bloating, and vomiting may occur, making a misdiagnosis likely. Despite the rarity of appendiceal intussusception, physicians should be aware of the potential for this diagnosis and remain vigilant, carefully observing patients during the diagnostic process and subsequent treatment.
The etiology of appendiceal intussusception is complex and involves both anatomical and pathophysiological factors. Anatomical intussusception is characterized by an appendix located below the cecum or in the pelvic position, a thin mesoappendix, a healthy appendiceal wall, and autonomous peristalsis. Pathophysiological intussusception is caused by abnormalities in the appendiceal cavity, such as foreign bodies, fecaliths, worms, or lesions involving the appendiceal wall, including mucinous cysts, lymphoid hyperplasia, papillomas, polyps, adenocarcinoma, sarcoma, and endometriosis. There are also rare reports of cases in which the ligated remnant invaginates during appendectomy[4-9]. In our case, appendiceal intussusception was likely secondary to the ileocecal tumor acting as a lead point, which is in accordance with the potential of the ileocecal tumor to cause intussusception.
According to McSwain's classification[10], appendiceal intussusception can be divided into five anatomical variations. Langsam et al[11] further simplified the classification into four types: Type I begins at the tip of the appendix, with the tip of the appendix as the intussusception and its proximal part invaginating into the cecum; Type II begins at the base of the appendix, with the base of the appendix and the cecum as the intussusception; Type III forms intussusception at the proximal end of the appendix and invaginates into the distal part; and type IV is a complete inversion of the appendix, accompanied by terminal ileum intussusception. Our patient had type IV appendiceal intussusception with complete inversion of the appendix, accompanied by cecal cancer, but without cecal intussusception. This condition is rare in clinical practice, and appendiceal intussusception is often overlooked. Patients may present with the typical symptoms of acute appendicitis, or with chronic intermittent abdominal pain, changes in bowel habits, and acute or chronic blood loss[12]. However, the abdominal pain in our patient was likely caused by appendiceal intussusception and localized swelling and inflammation associated with the tumor at the base of the appendix.
Appendiceal intussusception may present as a pedunculated or hyperplastic polyp during colonoscopy. In the present case, colonoscopy revealed an atypical polyp. When encountering such situations, physicians must consider whether cross-sectional imaging is required to rule out malignancies. In such cases, cross-sectional imaging studies such as CT or magnetic resonance imaging may provide more information, aiding in the accurate identification and assessment of the possibility of appendiceal intussusception. Resecting the polyp without further examination may lead to complications, such as appendicitis or intestinal perforation, which can result in peritonitis[13]. The pre-operative imaging in our case demonstrated a space-occupying lesion in the ileocecal region, which, combined with the patient’s clinical presentation and laboratory findings, raised concerns for a malignant process. After a comprehensive assessment of the patient’s clinical data, a decision was made to proceed with surgical intervention, which led to the discovery and diagnosis of appendiceal intussusception concurrent with cecal adenocarcinoma.
In conclusion, appendiceal intussusception is a rare anatomical variant of the appendix, presenting symptoms similar to those of appendicitis, thus necessitating attention in the differential diagnostic process. The patient in the present case had adenocarcinoma of the cecum involving the appendix, with subsequent appendiceal intussusception. The cancer cells had affected the serosal and muscular layers of the invaginated appendix, which is an exceedingly unusual finding. Surgeons and radiologists must thoroughly understand the clinical manifestations and imaging characteristics of appendiceal intussusceptions. While the exact causal relationship between appendiceal intussusception and colorectal cancer in this case was initially unclear, after careful consideration of the clinical and surgical findings, we recognized that the ileocecal tumor likely contributed to the intussusception of the appendix. Future studies should focus on the potential link between appendiceal intussusception and the occurrence of colorectal cancer.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
| 1. | M'Kidd J. Case of Invagination of the Cœcum and Appendix. Edinb Med J. 1859;4:793-796. [PubMed] |
| 2. | Collins DC. 71,000 human appendix specimens. A final report, summarizing forty years' study. Am J Proctol. 1963;14:265-281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Chaar CI, Wexelman B, Zuckerman K, Longo W. Intussusception of the appendix: comprehensive review of the literature. Am J Surg. 2009;198:122-128. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 66] [Cited by in RCA: 69] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 4. | Blondiaux E, Savoye-Collet C, Foulatier O, Lemoine F, Dacher JN. Appendiceal intussusception caused by a mucocele of the appendix: imaging findings. Dig Liver Dis. 2007;39:1087. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 5. | Karabulut R, Sönmez K, Türkyilmaz Z, Yilmaz Y, Akyürek N, Başaklar AC, Kale N. Mucosa-associated lymphoid tissue lymphoma in the appendix, a lead point for intussusception. J Pediatr Surg. 2005;40:872-874. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 11] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 6. | Kawamura YJ, Toyama N, Kasamatsu T, Ota M, Konishi F. Intussusception of appendiceal adenoma mimicking invasive carcinoma. Endoscopy. 2002;34:749. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 10] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 7. | Mathew J, Aldean IM, Ghafar FA, Haboubi NY. Appendicular intussusception into a polyp. Tech Coloproctol. 2004;8:113-115. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Moradi P, Barakate M, Gill A, Farrow G. Intussusception of the veriform appendix due to endometriosis presenting as acute appendicitis. ANZ J Surg. 2007;77:758-760. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 20] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 9. | Takahashi M, Sawada T, Fukuda T, Furugori T, Kuwano H. Complete appendiceal intussusception induced by primary appendiceal adenocarcinoma in tubular adenoma: a case report. Jpn J Clin Oncol. 2003;33:413-415. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 25] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 10. | Mcswain B. Intussusception of the appendix: review of the literature and report of a case. South Med J. 1941;34:263-270. [RCA] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 57] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 11. | Langsam LB, Raj PK, Galang CF. Intussusception of the appendix. Dis Colon Rectum. 1984;27:387-392. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 44] [Cited by in RCA: 46] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 12. | Casteels M, Eggermont E, Kerremans R, Ponnette E. Intussusception of the vermiform appendix: a preoperative diagnosis in an adolescent girl. J Pediatr Gastroenterol Nutr. 1986;5:159-162. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 13. | Fazio RA, Wickremesinghe PC, Arsura EL, Rando J. Endoscopic removal of an intussuscepted appendix mimicking a polyp--an endoscopic hazard. Am J Gastroenterol. 1982;77:556-558. [PubMed] |