Published online Mar 16, 2024. doi: 10.12998/wjcc.v12.i8.1430
Peer-review started: October 2, 2023
First decision: December 15, 2023
Revised: December 29, 2023
Accepted: February 18, 2024
Article in press: February 18, 2024
Published online: March 16, 2024
Processing time: 161 Days and 19.2 Hours
Peripherally inserted central catheters (PICCs) are an essential infusion route for oncology patients receiving intravenous treatments, but lower extremity veni
On 24 August 2022, a 58-year-old male was admitted to our department due to an intermittent cough persisting for over a month, which worsened 10 d prior. Imaging and laboratory investigations suggested the patient with pulmonary malignancy and SVCS. Chemotherapy was not an absolute contraindication in this patient. Lower extremity venipuncture is the preferred technique because administering upper extremity venous transfusion to patients with SVCS can exacerbate oedema in the head, neck, and upper extremities. The patient and his family were informed about the procedure, and informed consent was obtained. After successful puncture and prompt treatment, the patient was discharged, experiencing some relief from symptoms.
Inferior vena cava catheterisation is rare and important for cancer patients with SVCS, particularly in complex situations involving ectopic placement.
Core Tip: The conventional peripherally inserted central catheter catheterization selected deep venous vessels in the upper limb. Patients with superior vena cava syndrome (SVCS), lower extremity venipuncture is the preferred technique because administering upper extremity venous transfusion to patients with SVCS can exacerbate oedema in the head, neck, and upper extremities. The greater angle of the left lower extremity vein through the common iliac vein into the inferior vena cava and the conundrum that the left side of the femoral vein does not easily enter the inferior vena cava when passing through the common iliac vein, a right lower extremity catheterisation was performed in this case report.
- Citation: Zhu XJ, Zhao L, Peng N, Luo JM, Liu SX. Lower extremity peripherally inserted central catheter placement ectopic to the ascending lumbar vein: A case report. World J Clin Cases 2024; 12(8): 1430-1436
- URL: https://www.wjgnet.com/2307-8960/full/v12/i8/1430.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i8.1430
Due to their safety, reliability, and applicability, peripherally inserted central catheters (PICCs) play a crucial role in delivering chemotherapy and other intravenous treatments to oncology patients. PICCs have effectively prevented issues like repeated punctures, venous injury from chemotherapy drugs, and tissue necrosis caused by drug extravasation. In oncology, the prevalence of superior vena cava syndrome (SVCS) is notable. SVCS occurs due to partial or complete blockage of blood flow back to the right atrium via the superior vena cava. Patients with SVCS present with acute or subacute dyspnoea and oedema of the face and neck. Lower extremity venipuncture is the preferred technique because administering upper extremity venous transfusion to patients with SVCS can exacerbate oedema in the head, neck, and upper extremities. Peripherally inserted central catheterisation in the lower extremity is safe and feasible, providing a viable path for establishing safe venous transfusion in patients with SVCS while reducing the discomfort associated with repeated venous punctures. However, despite its benefits, peripherally inserted central catheterisation is associated with several complications such as catheter dislocation, rupture, leakage, occlusion, infections, phlebitis, and venous thrombosis. Herein, the case of a patient with a lower extremity PICC ectopic to the ascending lumbar vein is reported.
An intermittent cough persisting for over a month, which worsened 10 d prior.
In mid-July 2022, the patient developed intermittent cough, dry cough, but without diagnosis and treatment. In mid-August, the patient felt that his cough symptoms worsened, and was treated in a local hospital for chest computed tomography (CT) indicating lung occupying. Chest enhanced CT was further performed in The First Affiliated Hospital of Chongqing Medical University. Enhanced chest CT revealed a soft tissue mass in the right upper mediastinum and right hilus pulmonis suggesting a malignant neoplastic lesion, highly suggestive of mediastinal-type lung cancer involving the superior vena cava and the innominate vein, along with internal cancer thrombosis and multiple collateral circulations in the right neck and back root. Further, bronchofibrescopic biopsies were performed.
The patient was previously healthy, with no history of chronic disease, infectious diseases, and also suffered no accidental trauma. He also has a history of smoking for about 30 years and drinking alcohol for more than 20 years.
Father died of natural causes, mother died of "lung cancer" and siblings are in good health.
Temperature: 36.0 °C, pulse frequency: 76 times/min, respiratory rate: 20 times/min, blood pressure: 96/70 mmHg, clear mind, mental stability, walked into the ward, skin and mucous membranes of the whole body normal, no edema, no subcutaneous bleeding.
Except for the abnormalities of the relevant tumor markers, blood routine examination, urine routine examination, stool routine examination without special tips.
Enhanced chest CT revealed a soft tissue mass in the right upper mediastinum and the right hilus pulmonis, suggesting a malignant neoplastic lesion, highly suggestive of mediastinal-type lung cancer involving the superior vena cava and the innominate vein. Internal cancer-related thrombosis and multiple collateral circulations in the right neck and back root were also observed. Further, bronchofibrescopic biopsies confirmed the diagnoses of small cell lung cancer (cT4N3Mx) in the right hilus pulmonis, secondary malignancy in the lymph nodes, and SVCS.
The following diagnoses were established: (1) Small cell lung cancer (cT4N3Mx) in the right hilus pulmonis; (2) Secondary malignancy in the lymph nodes; and (3) SVCS.
Chemotherapy was not an absolute contraindication in this patient. Therefore, the initial treatment involved a chemo
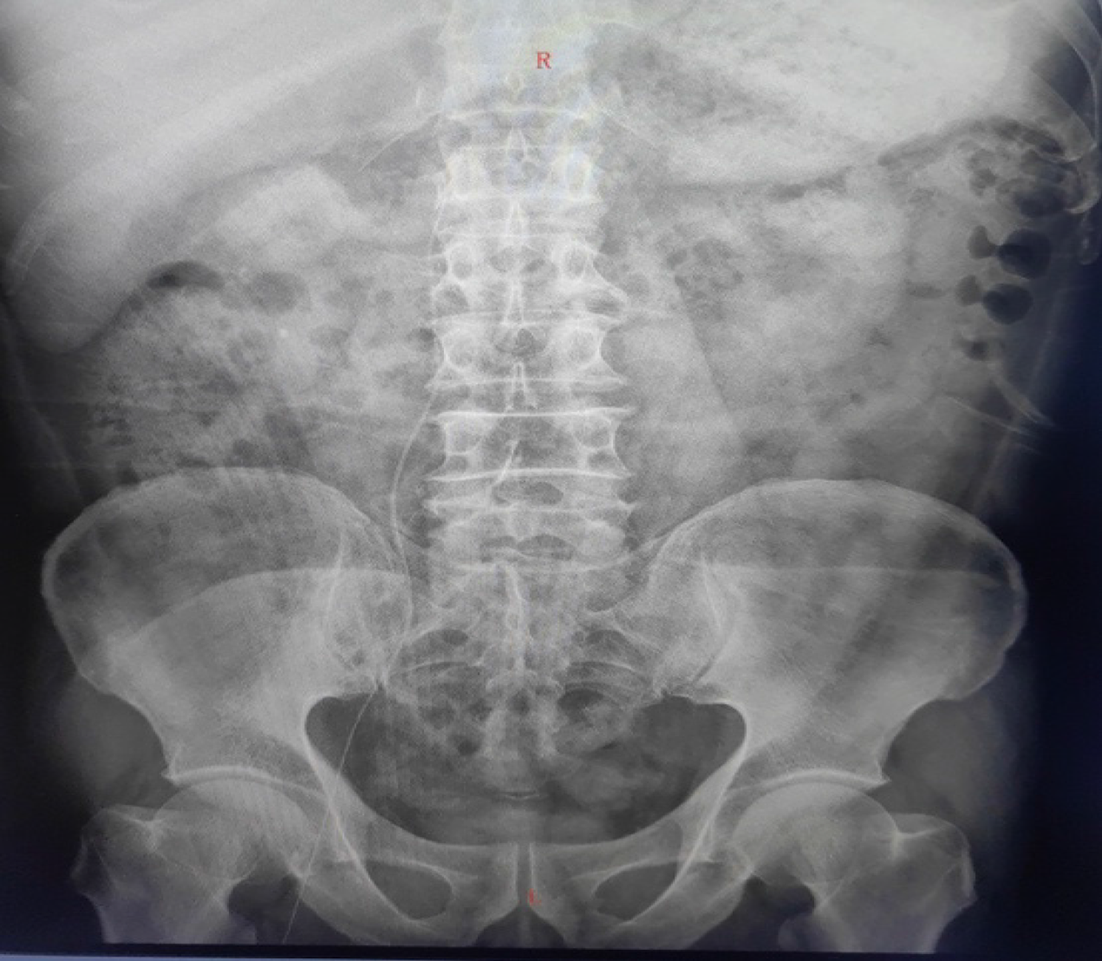
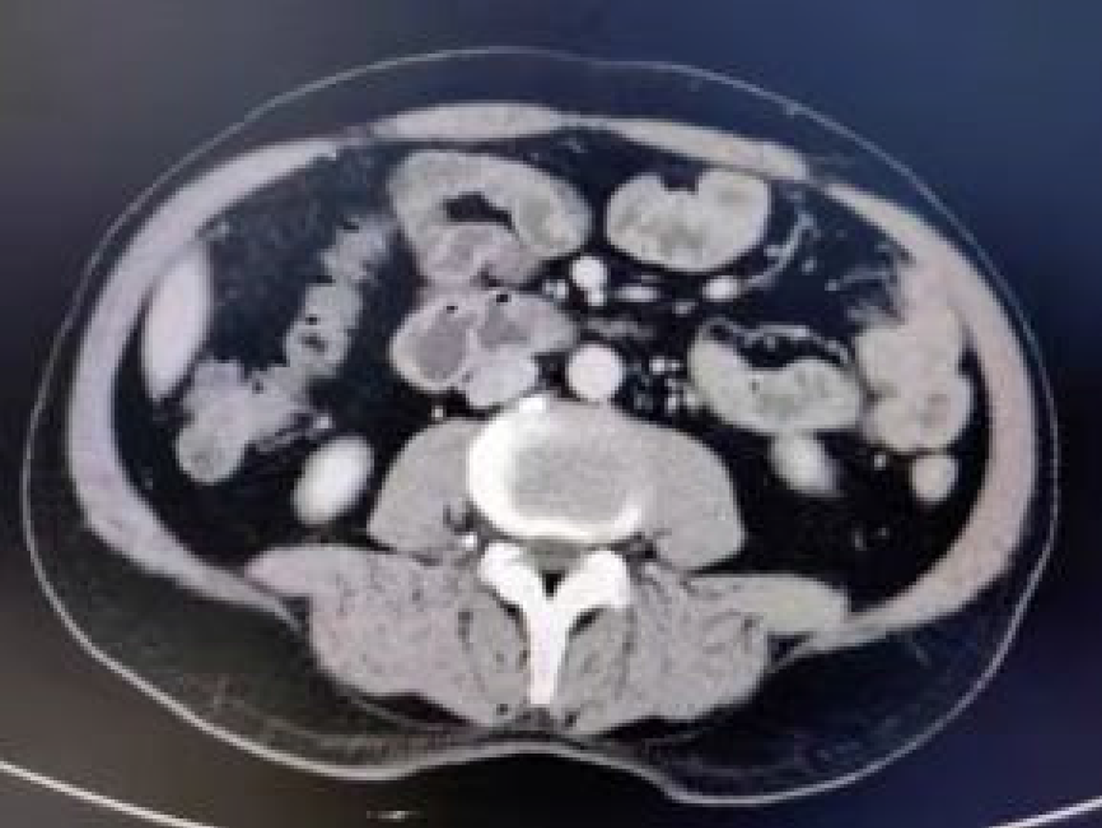
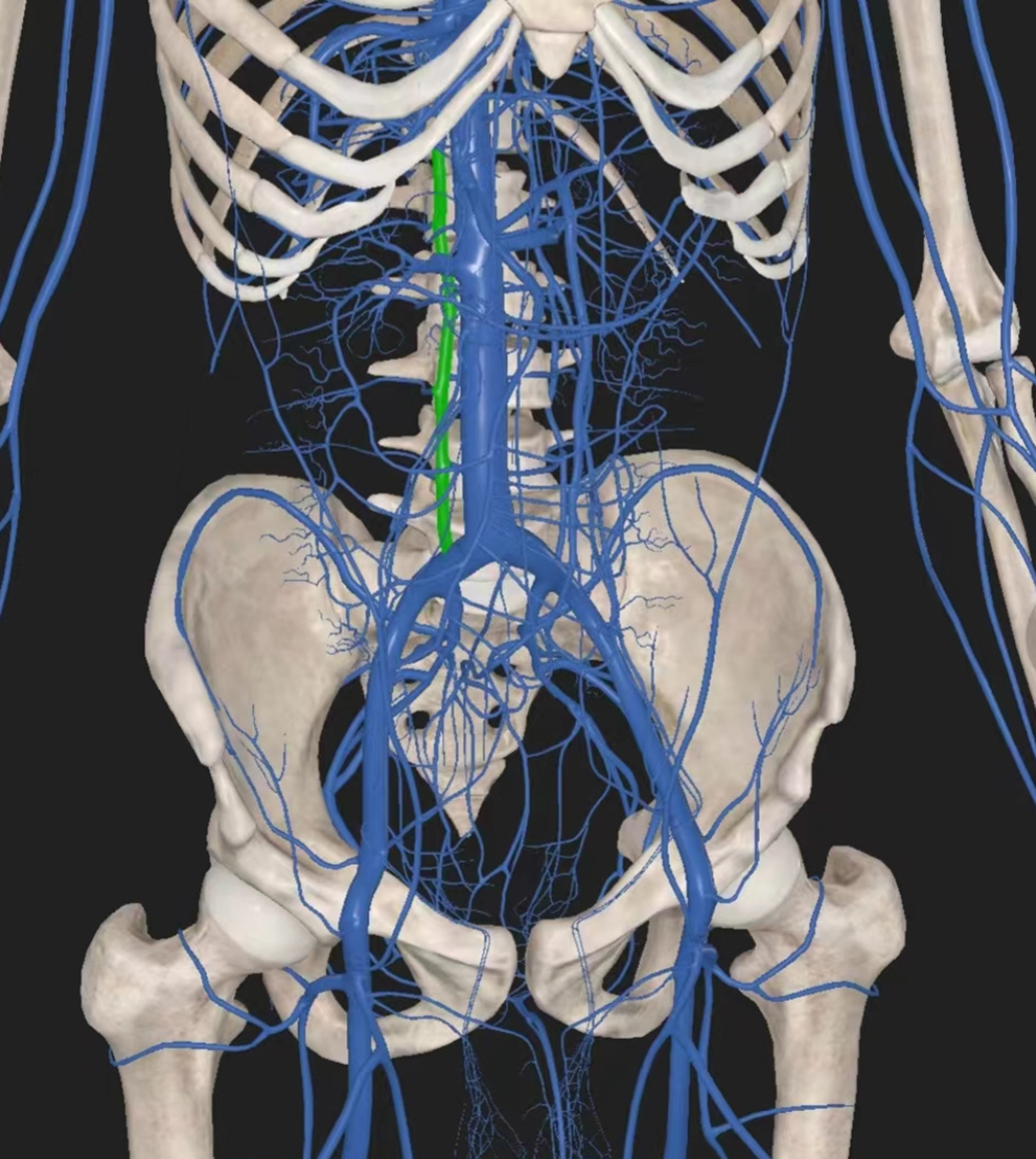
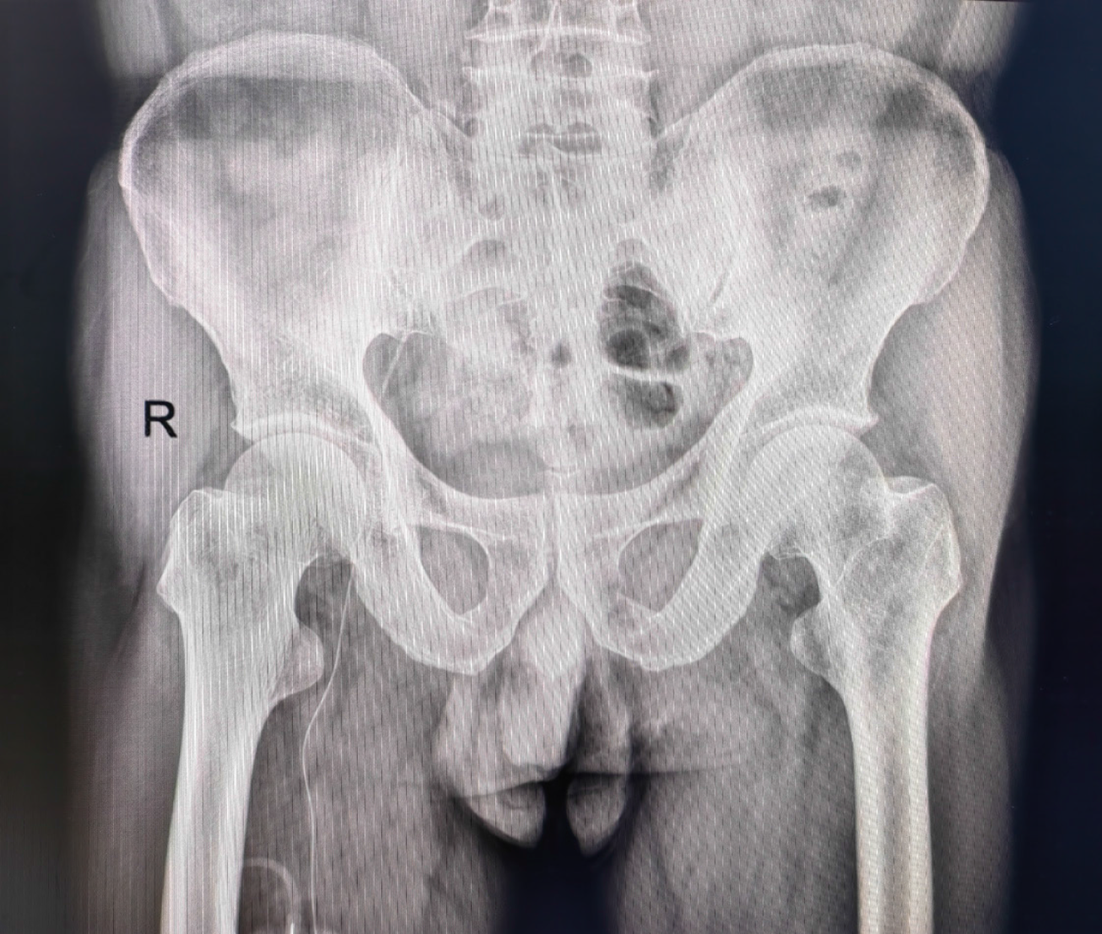
After successful puncture, abdominal radiography confirmed the catheter’s placement at lumbar 1 (Figure 1). Prompt treatment, the patient was discharged, experiencing some relief from symptoms. The patient was re-examined on 18 September 2022. Blood coagulation was observed within the catheter and extension tube, indicating a blockage due to haemagglutination (Figure 2). Despite negative pressure thrombolysis using urokinase during pumpback, no blood was observed; however, the transfusion flow remained unobstructed. A second test of conventional chest and abdominal radiography were performed to confirm the catheter’s placement, which indicated that the catheter tip was situated at lumbar 4, with 3 cm of it remaining exposed (Figure 3). This caused the catheter to bend within the vessel. Attempts to alleviate the obstruction by connecting saline to the syringe and quickly injecting it from the catheter cavity were made, followed by a re-examination through chest and abdomen flat slice imaging. Despite these efforts, the catheter tip was still located at lumbar 4. Although the catheter was retained due to successful administration of the second-cycle treatment, a CT re-examination at the end of the third-cycle treatment displayed the absence of the catheter within the superior vena cava (Figure 4). This was suggestive of a potential ectopic position. Subsequent analysis of vascular anatomy and CT images by the radiologist confirmed the catheter’s ectopic placement within the ascending lumbar vein (Figure 5). Reporting this to the hospital's venous specialist team prompted catheter removal, with successful blood retraction and transfusion upon catheter retraction to 28 cm. Finally, the catheter was safely secured after being cut and repositioned into the external iliac vein (Figure 6).
It is crucial for the nursing team to thoroughly evaluate the vessel before surgery to prevent potential intravascular complications[1].
In clinical practice, the right lower extremity vein is preferred for lower extremity catheterisation[2,3]. The complexity arises from the greater angle of the left lower extremity vein and passage through the common iliac vein into the inferior vena cava on the left side, making it challenging to place a catheter in the left lower extremity vein.
Several factors, such as blockage of the catheter’s open end, blood regurgitation due to various factors including cough-induced pressure[4], improper sealing of the catheter after transfusion, blood clot formation within the catheter, vascular injury, blood flow stagnation, a hypercoagulable state of the patient, and intraluminal occlusion due to fibrin or clot formation[5]. Considering these factors is crucial in clinical practice.
The lumbar veins are the ventral branches of the inferior vena cava. The dilated ascending lumbar vein is easily accessed using a guidewire. However, due to its alignment with the inferior vena cava along the longitudinal axis, distinguishing it in resulting radiographs becomes challenging. Moreover, the infrequency of such cases adds to the difficulty in identification. After encountering a series of late complications, a conclusion was reached through multidisciplinary discussions and CT.
Relevant studies suggest that an inaccurate position of the catheter tip poses a risk for unplanned extubation[6]. Herein, the lower extremity PICC tip did not fully reach the inferior vena cava[7]. Therefore, it is essential to consider the nature of the drug before administering it. Additionally, to prevent associated complications, a thorough assessment of catheter function and drug properties by the sedation nurse specialist, clinician, and pharmacist is essential before administration.
Incorrect catheter tip placement increases the risk of vascular perforation, infection, and ectopia, increasing the probability of arrhythmia, thrombosis, and potentially fatal outcomes[8]. This report highlights an unusual instance of a lower extremity PICC positioned ectopically in the ascending lumbar vein. Our study provides a basis for subsequent clinical care. It emphasises the need to holistically assess the patient’s overall condition by considering various factors in the context of the primary issue. Accurately identifying the vascular anatomy and precise determination of the catheter tip’s location are crucial for effective treatment and medication administration, particularly in patients with cancer. Early identification can lower complication rates, prolong catheter retention time, and improve patient satisfaction and quality of life. The collaborative efforts of a multidisciplinary team are crucial role in successful peripherally inserted central catheterisation and relevant care. However, inferior vena cava catheterisation is rare, particularly in complex situations involving ectopic placement. Therefore, multidisciplinary team collaboration, standardisation, and evaluation for special patient punctures have gained the interest of researchers.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Nursing
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Ueda H, Japan S-Editor: Zhang H L-Editor: A P-Editor: Zheng XM
| 1. | Raptis DA, Neal K, Bhalla S. Imaging Approach to Misplaced Central Venous Catheters. Radiol Clin North Am. 2020;58:105-117. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Gorski LA, Hadaway L, Hagle ME, Broadhurst D, Clare S, Kleidon T, Meyer BM, Nickel B, Rowley S, Sharpe E, Alexander M. Infusion Therapy Standards of Practice, 8th Edition. J Infus Nurs. 2021;44:S1-S224. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 229] [Cited by in RCA: 566] [Article Influence: 141.5] [Reference Citation Analysis (0)] |
| 3. | Wang YH, Su CS, Chang KH, Went CJ, Lee WL, Lai CH. Percutaneous intervention to correct central venous port catheter malposition. Perfusion. 2018;33:404-406. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 4. | Guimarães AF, Souza AA, Bouzada MC, Meira ZM. Accuracy of chest radiography for positioning of the umbilical venous catheter. J Pediatr (Rio J). 2017;93:172-178. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 22] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 5. | Hawthorn A, Bulmer AC, Mosawy S, Keogh S. Implications for maintaining vascular access device patency and performance: Application of science to practice. J Vasc Access. 2019;20:461-470. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Gorski LA. Complication of infusion therapy. In: Gorski LA. Phillips´s Manual of I.V. Therapeutics: Evidence-Based Practice for infusion Therapy. 7th ed. Philadelphia: F.A. Davis Company, 2018. |
| 7. | Kisa P, Ting J, Callejas A, Osiovich H, Butterworth SA. Major thrombotic complications with lower limb PICCs in surgical neonates. J Pediatr Surg. 2015;50:786-789. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 8. | Sertic AJ, Connolly BL, Temple MJ, Parra DA, Amaral JG, Lee KS. Perforations associated with peripherally inserted central catheters in a neonatal population. Pediatr Radiol. 2018;48:109-119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 26] [Cited by in RCA: 33] [Article Influence: 4.7] [Reference Citation Analysis (0)] |