Published online Mar 16, 2024. doi: 10.12998/wjcc.v12.i8.1382
Peer-review started: November 29, 2023
First decision: January 15, 2024
Revised: January 24, 2024
Accepted: February 25, 2024
Article in press: February 25, 2024
Published online: March 16, 2024
Processing time: 103 Days and 17.3 Hours
Chronic heart failure (HF) is a clinical syndrome with high morbidity and mor
Core Tip: Cardiac rehabilitation (CR) is a medically supervised program designed to maintain or improve cardiovascular health of patients with heart failure (HF), recommended by guidelines. CR has been shown to be beneficial in HF, leading to improvements in central hemodynamic status and peripheral vascular, endothelial, and skeletal muscle function and, most significantly, in peak and submaximal exercise capacity, cardiorespiratory fitness, and quality of life. Main endpoints of a CR program include a wide spectrum of functional and psychological variables. Despite the strong recommendations in the guidelines, the attendance rates remain at low levels due to several barriers related to healthcare professionals, patients, and states.
- Citation: Kourek C, Briasoulis A, Magouliotis DE, Skoularigis J, Xanthopoulos A. Latest updates on structure and recommendations of cardiac rehabilitation programs in chronic heart failure. World J Clin Cases 2024; 12(8): 1382-1387
- URL: https://www.wjgnet.com/2307-8960/full/v12/i8/1382.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i8.1382
Chronic heart failure (HF) is a clinical syndrome with high morbidity and mortality worldwide and a tremendous socioeconomic burden[1,2]. Depending on the development and progression of the disease, advanced stages are associated with a reduced survival[3]. The prevalence of HF in Europe appears to be 12% of adults, increasing with age from 1% for those aged < 55 years to > 10% in those aged 70 years or more, while the incidence is approximately 5/1000 person-years[4,5]. Prognosis of patients with HF has improved significantly during the last decades, with HF with mildly reduced ejection fraction (HFmrEF) demonstrating better prognosis compared to HF with reduced ejection fraction (HFrEF). Mortality rate from hospitalized patients is shown to be lower in patients with HF with preserved ejection fraction (HFpEF) compared to patients with HFrEF (adjusted hazard ratio 0.68, 95%CI: 0.64-0.71)[6]. However, quality of life in HF patients remains poor[2].
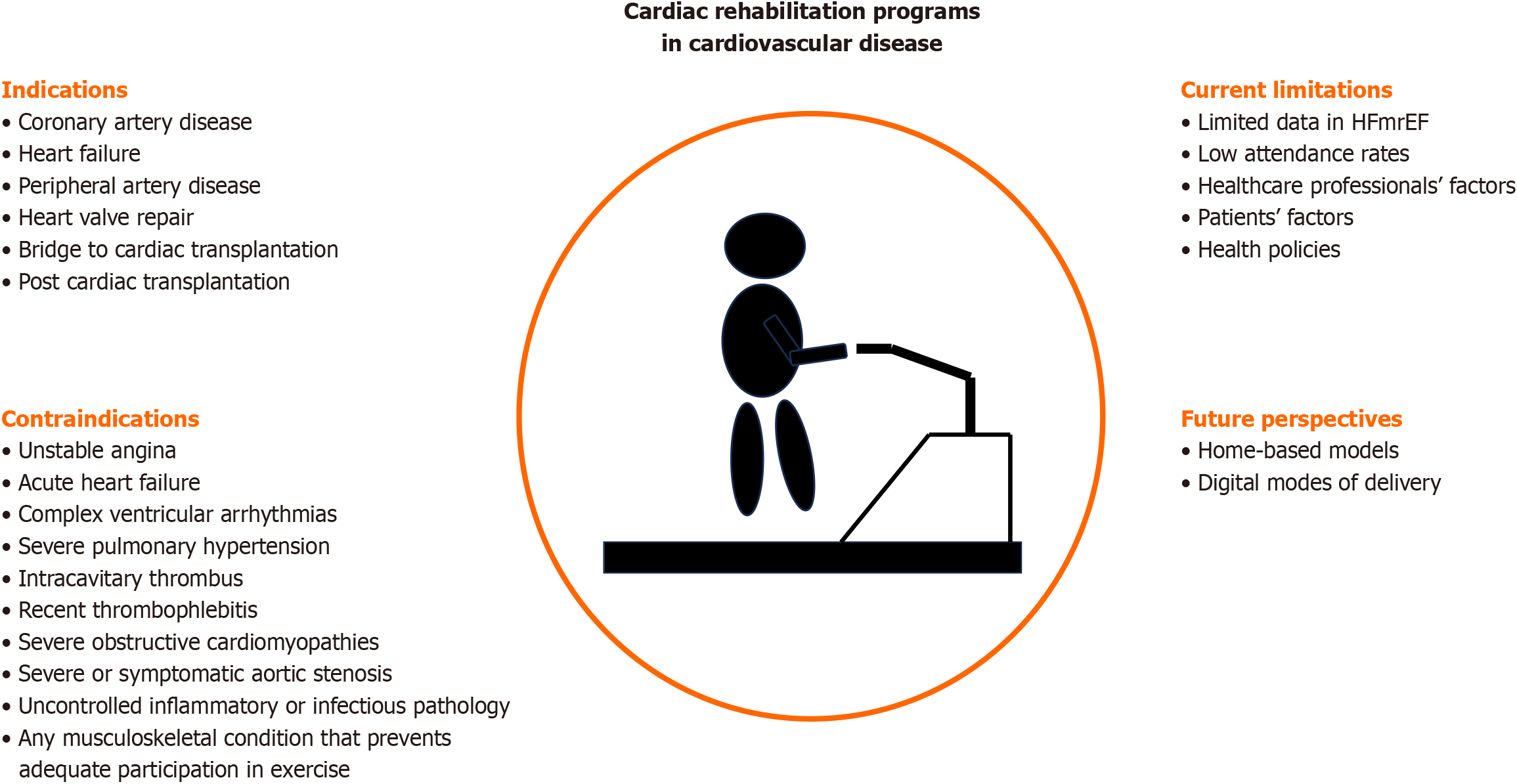
Cardiac rehabilitation (CR) is a medically supervised program designed to maintain or improve cardiovascular health of patients with cardiovascular disease (Figure 1). It is considered to be crucial in the secondary prevention in HF and is recommended by both American and European guidelines[1,2]. A CR program consists of a multispecialty group including physicians, nurses, physiotherapists, trainers, ergophysiologists, dietitians, and psychologists with the common purpose of improving functional capacity and quality of life of chronic HF patients. Variables such as the eligibility criteria of patients, the structure of the program, and the implemented exercise training protocols will be discussed in detail in the present editorial. Moreover, we are going to present all the updated knowledge and recommendations in CR programs.
Indications for CR include history of coronary artery disease, congestive HF, peripheral artery disease, heart valve repair, as a bridge to cardiac transplantation, and post cardiac transplantation[7]. Especially in cardiac transplantation, exercise training can mitigate the impact of the decreased strength and skeletal muscle abnormalities that develop prior to transplantation[8].
Most patients with HF, who are stable under medications, are capable of participating in CR programs. CR has been shown to be beneficial in all ejection fraction (EF) categories in HF. Specifically in HFrEF, exercise training leads to improvements in central hemodynamic status and peripheral vascular, endothelial, and skeletal muscle function, attenuation of sympathetic and neurohormonal activation, reduction in circulating levels of N-terminal pro–B type natriuretic peptide, and increases in vagal tone[9]. A recent systematic review and meta-analysis including 4481 patients showed that exercise-based CR is likely to improve exercise capacity and quality of life in HFrEF[10]. Similar beneficial results have been also demonstrated in HFpEF with several studies and meta-analyses showing significant improvements in peak and submaximal exercise capacity, cardiorespiratory fitness, and quality of life, as well as atrial reverse remodeling and improved left ventricular diastolic function[11]. In HFmrEF, data remains limited. A recent study showed that early CR significantly reduced cardiac death and re-hospitalization in these patients[12]. However, more studies regarding the potential benefits of CR are mandatory.
Patients with contraindications to exercise training are those with unstable angina, acute decompensated congestive HF, complex ventricular arrhythmias, severe pulmonary hypertension (right ventricular systolic pressure greater than 60 mmHg), intracavitary thrombus, recent thrombophlebitis with or without pulmonary embolism, severe obstructive cardiomyopathies, severe or symptomatic aortic stenosis, uncontrolled inflammatory or infectious pathology, or any musculoskeletal condition that prevents adequate participation in exercise[11,13]. Nevertheless, even these patients could benefit from specific exercise training modalities of low or intermediate intensity and/or individualized training protocols.
An individualized exercise prescription should be developed on the basis of a baseline evaluation in all patients, with incorporation of the goals of the patient and the treatment team[13]. The cardiopulmonary exercise testing (CPET) is the gold standard for the diagnostic evaluation of exercise intolerance, as well as for individualized prescription of structured physical training, along with the functional impairment reported by patients[14]. Some CR centers even include a repeat CPET after several weeks of training in order to guide the intensity progression[14].
CR is divided into three phases: I, II, and III, all of which aim to prevent further cardiovascular disease[14]. Phase I, consisting of early mobilization of the stable cardiac patient to the level of activity required to perform simple household tasks, is the clinical phase and is initiated while the patient is still in the hospital. Phase II is a supervised ambulatory outpatient program, usually with a duration of 3 to 6 months, which consists of outpatient monitored exercise while phase III (or post-CR) is a lifetime maintenance phase which consists of home- or gym-based exercise with the goal of continuing the risk factor modification and exercise program learned during phase II[14]. Another phase of CR is ‘’pre-habilitation’’, a pre-surgery phase usually before cardiac transplantation and coronary artery bypass grafting or under extracorporeal membrane oxygenation support[15]. However, this definition is not established in all countries, indicating a global variation regarding stages of CR.
CR is consisted by multiple components except for the patient, including the patient's family, different specialized physicians such as surgeons, cardiologists, physiatrists, and pneumonologists, specialized nurses, physical therapists, occupational therapists, pharmacists, psychologists, nutritionists, and other administrative officers[13]. CR programs do not consist of exercise training alone but a number of core components including baseline patient assessment, nutritional counseling, lifestyle modification, risk factor management for lipids, blood pressure, weight, diabetes, and smoking, psychosocial interventions, and physical activity counseling.
The main modality of exercise training is aerobic exercise which can be classified into different categories of intensity according to maximum oxygen consumption (VO2 max), maximum heart rate (max HR), heart rate reserve (HRR), and ratings of perceived exertion (RPE) scale of the initial CPET in each patient[16]. Specifically, low intensity exercise is defined as < 40% of VO2 max or < 55% of max HR or < 40% of HRR or 10-11 of the RPE scale while moderate intensity exercise as 40%-69% of VO2 max or 55%-74% of max HR or 40%-69% of HRR or 12-13 of the RPE scale. Moreover, high intensity exercise is defined as 70%-85% of VO2 max or 75%-90% of max HR or 70%-85% of HRR or 14-16 of the RPE scale, and very high intense exercise as > 85% of VO2 max or > 90% of max HR or > 85% of HRR or 17-19 of the RPE scale. Low and moderate intensity exercise includes aerobic training zone, high intensity includes both aerobic and lactate training zones, and very high intensity includes aerobic, lactate, and anaerobic training zones[16]. All the above parameters derive from the CPET measurements while the main tool of the RPE scale is the 20-point Borg scale.
Another major exercise training modality is muscle strength/resistance training. In resistance training, intensity is determined according to the 1 repetition maximum (1RM) test. Patients usually start from light initial loads at initiation of CR, with approximately 12-15 repetitions at 30% of 1RM and 40% of 1RM for the upper and lower body, respectively[16]. The recovery phase should be at least twice the time of the contraction phase. In the meantime, the intensity should be increased up to 70% of 1RM and 80% of 1RM for the upper and lower body, respectively, during the CR program[16].
It should be made clear that the progression of the intensity of aerobic and resistance training in CR should be made only when it is medically safe and patients are able to execute the exercises with proper technique and do not present orthopedic symptoms, cardiac arrhythmias, or episodes of syncope or dizziness[17].
Other exercise training modalities include inspiratory muscle training, neuromuscular electrical stimulation, as well as water and breathing exercises.
The main endpoints of a CR program include a wide spectrum of functional and psychological variables[17]: (1) Exercise capacity measured by peak VO2, 6-min walking test distance, power output, or exercise duration is an important parameter for the assessment of CR. Improvements in one of these indices is related to improvement in cardiorespiratory fitness of an HF patient; (2) Cardiac function measured by peak cardiac output, stroke volume, HR, or left ventricular EF is another important criterion of the effectiveness of a CR program; (3) Microcirculation assessed by peripheral conduit artery function through endothelial-dependent vasodilation, skeletal muscle function, and endothelial function is the cornerstone for potential benefit in the clinical impact in HF patients; (4) Sympathetic nervous system activity as measured by muscle sympathetic nervous system activity at both rest and during exercise; (5) Health status and quality of life assessed by the Kansas City Cardiomyopathy Questionnaire and the Minnesota Living with Heart Failure Questionnaire has a direct impact in the daily life of HF patients; and (6) Clinical outcomes including all-cause and HF-specific hospitalization and mortality are probably the most significant outcomes for most randomized controlled trials and determine future guidelines in HF.
All these outcomes are objective and measurable in the effectiveness of a CR program. However, their importance in patients with HF is controversial. They are useful when there is also a clinical relevance such as improvement in their symptoms and daily activities, increase of their exercise tolerance, and improved quality of life. In other words, surrogate markers should be interpreted with caution and, perhaps, we should be focusing on what is important to patients. Probably, mortality and all-cause admission to hospital seem to be more important than many of these variables. Unfortunately, data from the largest trials have been disappointing so far. For instance, the Rehabilitation after Myocardial Infarction Trial that compared 1813 patients after myocardial infraction referred to comprehensive CR programs or discharged to ‘’usual care’’, found no important effect on mortality, cardiac or psychological morbidity, risk factors, or health-related quality of life or activity[18].
As far as safety is concerned, most studies have found no evidence suggesting that exercise training causes harm in terms of an increased risk of all-cause death in patients with chronic stable HF. It is reported that one case of heart attack occurs per 300000 exercise hours and the mortality rate is also quite low (0 to 1 case per 300000 exercise hours)[16]. Non-fatal events such as arrhythmias, syncope, musculoskeletal injuries, and dyspnea are more common, especially in high-risk patients.
Due to the lack of data in all types of HF, more randomized controlled trials are required. Specifically, there is a general lack of high-quality research in CR compared with pharma trials and lack of strong mortality outcomes in both HFpEF and HFrEF. Many CR trials include small samples and the most significant data derive from meta-analysis of small trails, which is at high risk of bias.
Despite strong guideline recommendations for CR, attendance rates remain at low levels in cardiovascular disease patients: < 20% in Europe and the United States over the last 2 decades[19]. Healthcare professional factors including lack of endorsement of CR by clinicians due to the lack of awareness on the evidence of its effectiveness, patient factors including physical, psychosocial, and economic aspects that influence their participation in CR, and state factors including reduced or bad-organized availability of CR programs, health policies, and small number of campaigns on rehabilitation limit HF patients from participating in such rehabilitation programs[19].
Alternatives to center-based programs include home-based models and digital modes of delivery, such as cardiac tele-rehabilitation through the use of mobile or internet-based communication and social media platforms that allow patients to access CR virtually[20]. The major advantages of home-based CR programs are the expanded access, individually tailored programs, convenient scheduling, minimal transportation barriers, privacy, and integration with regular home routine while the main disadvantages compared to the traditional CR programs are less intensive exercise training, less social support, less face-to-face monitoring and communication, and safety concerns for patients at higher risk[20]. Cardiac tele-rehabilitation, however, is not feasible for every patient, as lower levels of digital literacy and access to the Internet in certain groups such as ethnic minorities, the elderly, and the socioeconomically deprived could limit their participation[20].
CR is a significant tool in the therapeutic approach of HF, recommended by the most recent guidelines. Careful evaluation of HF patients, appropriate exercise prescription, and individualized goals for each patient are some aspects of a successful CR program. However, there are still significant gaps in the literature, especially regarding specific HF subgroups and future perspectives of CR. As a result, more randomized controlled trials are required in order to create individualized exercise training protocols.
Provenance and peer review: Invited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Cardiac and cardiovascular systems
Country/Territory of origin: Greece
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Leslie SJ, United Kingdom S-Editor: Zhang H L-Editor: Wang TQ P-Editor: Zhao YQ
| 1. | Heidenreich PA, Bozkurt B, Aguilar D, Allen LA, Byun JJ, Colvin MM, Deswal A, Drazner MH, Dunlay SM, Evers LR, Fang JC, Fedson SE, Fonarow GC, Hayek SS, Hernandez AF, Khazanie P, Kittleson MM, Lee CS, Link MS, Milano CA, Nnacheta LC, Sandhu AT, Stevenson LW, Vardeny O, Vest AR, Yancy CW. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: Executive Summary: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. 2022;145:e876-e894. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 231] [Article Influence: 77.0] [Reference Citation Analysis (1)] |
| 2. | McDonagh TA, Metra M, Adamo M, Gardner RS, Baumbach A, Böhm M, Burri H, Butler J, Čelutkienė J, Chioncel O, Cleland JGF, Crespo-Leiro MG, Farmakis D, Gilard M, Heymans S, Hoes AW, Jaarsma T, Jankowska EA, Lainscak M, Lam CSP, Lyon AR, McMurray JJV, Mebazaa A, Mindham R, Muneretto C, Francesco Piepoli M, Price S, Rosano GMC, Ruschitzka F, Skibelund AK; ESC Scientific Document Group. 2023 Focused Update of the 2021 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure. Eur Heart J. 2023;44:3627-3639. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 37] [Cited by in RCA: 923] [Article Influence: 461.5] [Reference Citation Analysis (0)] |
| 3. | Garascia A, Palazzini M, Tedeschi A, Sacco A, Oliva F, Gentile P. Advanced heart failure: from definitions to therapeutic options. Eur Heart J Suppl. 2023;25:C283-C291. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 4] [Cited by in RCA: 4] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Roger VL. Epidemiology of Heart Failure: A Contemporary Perspective. Circ Res. 2021;128:1421-1434. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 58] [Cited by in RCA: 507] [Article Influence: 126.8] [Reference Citation Analysis (0)] |
| 5. | Tsao CW, Aday AW, Almarzooq ZI, Anderson CAM, Arora P, Avery CL, Baker-Smith CM, Beaton AZ, Boehme AK, Buxton AE, Commodore-Mensah Y, Elkind MSV, Evenson KR, Eze-Nliam C, Fugar S, Generoso G, Heard DG, Hiremath S, Ho JE, Kalani R, Kazi DS, Ko D, Levine DA, Liu J, Ma J, Magnani JW, Michos ED, Mussolino ME, Navaneethan SD, Parikh NI, Poudel R, Rezk-Hanna M, Roth GA, Shah NS, St-Onge MP, Thacker EL, Virani SS, Voeks JH, Wang NY, Wong ND, Wong SS, Yaffe K, Martin SS; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart Disease and Stroke Statistics-2023 Update: A Report From the American Heart Association. Circulation. 2023;147:e93-e621. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1045] [Cited by in RCA: 2479] [Article Influence: 1239.5] [Reference Citation Analysis (0)] |
| 6. | Meta-analysis Global Group in Chronic Heart Failure (MAGGIC). The survival of patients with heart failure with preserved or reduced left ventricular ejection fraction: an individual patient data meta-analysis. Eur Heart J. 2012;33:1750-1757. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 508] [Cited by in RCA: 548] [Article Influence: 39.1] [Reference Citation Analysis (0)] |
| 7. | Wheat HL, Fedson S, Bozkurt B, Josephson RA. Cardiac rehabilitation in heart failure: Indications for exercise training based on heart failure phenotype. Prog Cardiovasc Dis. 2022;70:16-21. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 8. | Kourek C, Karatzanos E, Nanas S, Karabinis A, Dimopoulos S. Exercise training in heart transplantation. World J Transplant. 2021;11:466-479. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 28] [Cited by in RCA: 23] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 9. | Kourek C, Briasoulis A, Karatzanos E, Zouganeli V, Psarra K, Pratikaki M, Alevra-Prokopiou A, Skoularigis J, Xanthopoulos A, Nanas S, Dimopoulos S. The Effects of a Cardiac Rehabilitation Program on Endothelial Progenitor Cells and Inflammatory Profile in Patients with Chronic Heart Failure of Different Severity. J Clin Med. 2023;12. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 1] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Bjarnason-Wehrens B, Nebel R, Jensen K, Hackbusch M, Grilli M, Gielen S, Schwaab B, Rauch B; German Society of Cardiovascular Prevention and Rehabilitation (DGPR). Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): A systematic review and meta-analysis. Eur J Prev Cardiol. 2020;27:929-952. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 55] [Cited by in RCA: 91] [Article Influence: 15.2] [Reference Citation Analysis (0)] |
| 11. | Sachdev V, Sharma K, Keteyian SJ, Alcain CF, Desvigne-Nickens P, Fleg JL, Florea VG, Franklin BA, Guglin M, Halle M, Leifer ES, Panjrath G, Tinsley EA, Wong RP, Kitzman DW; American Heart Association Heart Failure and Transplantation Committee of the Council on Clinical Cardiology; Council on Arteriosclerosis, Thrombosis and Vascular Biology; and American College of Cardiology. Supervised Exercise Training for Chronic Heart Failure With Preserved Ejection Fraction: A Scientific Statement From the American Heart Association and American College of Cardiology. Circulation. 2023;147:e699-e715. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 65] [Cited by in RCA: 63] [Article Influence: 31.5] [Reference Citation Analysis (0)] |
| 12. | Adachi T, Iritani N, Kamiya K, Iwatsu K, Kamisaka K, Iida Y, Yamada S; FLAGSHIP collaborators. Prognostic Effects of Cardiac Rehabilitation in Patients With Heart Failure (from a Multicenter Prospective Cohort Study). Am J Cardiol. 2022;164:79-85. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 4] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 13. | Bozkurt B, Fonarow GC, Goldberg LR, Guglin M, Josephson RA, Forman DE, Lin G, Lindenfeld J, O'Connor C, Panjrath G, Piña IL, Shah T, Sinha SS, Wolfel E; ACC’s Heart Failure and Transplant Section and Leadership Council. Cardiac Rehabilitation for Patients With Heart Failure: JACC Expert Panel. J Am Coll Cardiol. 2021;77:1454-1469. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 164] [Article Influence: 41.0] [Reference Citation Analysis (0)] |
| 14. | Hansen D, Abreu A, Ambrosetti M, Cornelissen V, Gevaert A, Kemps H, Laukkanen JA, Pedretti R, Simonenko M, Wilhelm M, Davos CH, Doehner W, Iliou MC, Kränkel N, Völler H, Piepoli M. Exercise intensity assessment and prescription in cardiovascular rehabilitation and beyond: why and how: a position statement from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur J Prev Cardiol. 2022;29:230-245. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 88] [Cited by in RCA: 161] [Article Influence: 53.7] [Reference Citation Analysis (1)] |
| 15. | Kourek C, Nanas S, Kotanidou A, Raidou V, Dimopoulou M, Adamopoulos S, Karabinis A, Dimopoulos S. Modalities of Exercise Training in Patients with Extracorporeal Membrane Oxygenation Support. J Cardiovasc Dev Dis. 2022;9. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 4.7] [Reference Citation Analysis (0)] |
| 16. | Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, Collet JP, Corrado D, Drezner JA, Halle M, Hansen D, Heidbuchel H, Myers J, Niebauer J, Papadakis M, Piepoli MF, Prescott E, Roos-Hesselink JW, Graham Stuart A, Taylor RS, Thompson PD, Tiberi M, Vanhees L, Wilhelm M; ESC Scientific Document Group. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42:17-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 358] [Cited by in RCA: 1008] [Article Influence: 252.0] [Reference Citation Analysis (1)] |
| 17. | Keteyian SJ, Michaels A. Heart Failure in Cardiac Rehabilitation: A review and practical considerations. J Cardiopulm Rehabil Prev. 2022;42:296-303. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 10] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 18. | West RR, Jones DA, Henderson AH. Rehabilitation after myocardial infarction trial (RAMIT): multi-centre randomised controlled trial of comprehensive cardiac rehabilitation in patients following acute myocardial infarction. Heart. 2012;98:637-644. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 155] [Cited by in RCA: 171] [Article Influence: 12.2] [Reference Citation Analysis (0)] |
| 19. | Taylor RS, Dalal HM, Zwisler AD. Cardiac rehabilitation for heart failure: 'Cinderella' or evidence-based pillar of care? Eur Heart J. 2023;44:1511-1518. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 66] [Article Influence: 33.0] [Reference Citation Analysis (0)] |
| 20. | Dalal HM, Doherty P, McDonagh ST, Paul K, Taylor RS. Virtual and in-person cardiac rehabilitation. BMJ. 2021;373:n1270. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 47] [Cited by in RCA: 57] [Article Influence: 14.3] [Reference Citation Analysis (0)] |