Published online Mar 6, 2024. doi: 10.12998/wjcc.v12.i7.1356
Peer-review started: December 10, 2023
First decision: December 18, 2023
Revised: December 27, 2023
Accepted: February 2, 2024
Article in press: February 2, 2024
Published online: March 6, 2024
Processing time: 81 Days and 16.6 Hours
While most complications of cervical surgery are reversible, some, such as symptomatic postoperative spinal epidural hematoma (SEH), which generally occurs within 24 h, are associated with increased morbidity and mortality. Delayed neurological dysfunction is diagnosed in cases when symptoms present > 3 d postoperatively. Owing to its rarity, the risk factors for delayed neurological dysfunction are unclear. Consequently, this condition can result in irreversible neurological deficits and serious consequences. In this paper, we present a case of postoperative SEH that developed three days after hematoma evacuation.
A 68-year-old man with an American Spinal Injury Association (ASIA) grade C injury was admitted to our hospital with neck pain and tetraplegia following a fall. The C3-C7 posterior laminectomy and the lateral mass screw fixation surgery were performed on the tenth day. Postoperatively, the patient showed no changes in muscle strength or ASIA grade. The patient experienced neck pain and subcutaneous swelling on the third day postoperatively, his muscle strength decreased, and his ASIA score was grade A. Magnetic resonance imaging showed hypointense signals on T1 weighted image (T1WI) and T2WI located behind the epidural space, with spinal cord compression. Emergency surgical intervention for the hematoma was performed 12 h after onset. Although hypoproteinemia and pleural effusion did not improve in the perioperative period, the patient recovered to ASIA grade C on day 30 after surgery, and was transferred to a functional rehabilitation exercise unit.
This case shows that amelioration of low blood albumin and pleural effusion is an important aspect of the perioperative management of cervical surgery. Surgery to relieve the pressure on the spinal cord should be performed as soon as possible to decrease neurological disabilities.
Core Tip: Symptomatic postoperative spinal epidural hematoma (PSEH) is a rare but fatal complication of spinal surgery. Here, we present the case of a patient who underwent cervical laminectomy for cervical spinal cord injury with tetraplegia complicated by PSEH. Hypoproteinemia and pleural effusion can aggravate spinal cord edema and worsen the neurological symptoms. Emergency hematoma evacuation is an effective method to relieve the pressure on the spinal cord. A literature review of similar cases was performed.
- Citation: Yan RZ, Chen C, Lin CR, Wei YH, Guo ZJ, Li YK, Zhang Q, Shen HY, Sun HL. Delayed neurological dysfunction following posterior laminectomy with lateral mass screw fixation: A case report and review of literature. World J Clin Cases 2024; 12(7): 1356-1364
- URL: https://www.wjgnet.com/2307-8960/full/v12/i7/1356.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i7.1356
Posterior cervical decompressive laminectomy and lateral mass screw-rod arthrodesis are safe and effective with good long-term efficacy, and have been widely used to manage a variety of cervical spine disorders, including cervical spinal cord injury and multi-segmental cervical spinal canal stenosis[1-4]. Common complications include spinal cord injury, C5 nerve palsy, loss of motion, loss of lordosis, and other complications related to the fixation instruments[4]. Most complications are mild or reversible, and do not require reoperation. Among the complications of this procedure, the incidence of postoperative spinal epidural hematoma (SEH) is extremely low, ranging from only 0.05%-3%[1]. Symptomatic postoperative SEH manifests as surgical site pain, breathing difficulties, and progressive paralysis, and undetected postoperative SEH can lead to severe neurological deficits and even death. Therefore, prompt surgical decompression is usually recommended to prevent irreversible disability[5].
Most postoperative SEH cases are diagnosed within a few days, generally within 24 h after surgery, as initial wound healing is not yet complete[5]. However, postoperative SEH is rarely diagnosed more than three days after surgery; a situation termed delayed postoperative SEH[5,6]. Due to its rarity, little attention has been paid to delayed postoperative SEH following posterior cervical decompressive laminectomy, and literature on the topic is scarce. This lack of knowle
In the present study, we report a case of delayed SEH that developed three days after cervical C3-C7 laminectomy. The patient was promptly diagnosed and underwent urgent evacuation of the hematoma. Fortunately, serious consequences were avoided because of the prompt treatment.
The patient was a 68-year-old man admitted to our institute with a chief complaint of neck pain and tetraplegia following a fall.
Half an hour before presenting to the Emergency Department, the patient fell down and hit his head and neck on a stone while pushing his bicycle on the roadside. He experienced neck pain and could not move his limbs without head, chest, or abdominal pain.
The patient had no history of hypertension, diabetes mellitus, trauma, or tumors. The patient was vegetarian, and his body mass index was 21.91 kg/m2.
The patient had no relevant family medical history.
Upon physical examination, the patient’s temperature was 36.2 °C, his blood pressure was 100/65 mmHg, his respiratory rate was 20 breaths per minute, his heart rate was 70 beats per minutes, and he was fully conscious. The patient’s conscious sensory function and partial motor function were preserved. Sensory function was also preserved in the anal and perineal areas. The muscle strength in the extremities was as follows: Left upper limb, grade 3; right upper limb, grade 2; internal muscles of the hand, grade 0; left lower limb, grade 3; and right lower limb, grade 2. The injury was graded as a grade C injury according to the American Spinal Injury Association scoring system.
The patient’s preoperative coagulation function and platelet count were normal, while other laboratory findings were as follows: Plasma albumin, 34.3 g/L; hemoglobin, 107 g/L; and uric acid, 157.00 μmol/L.
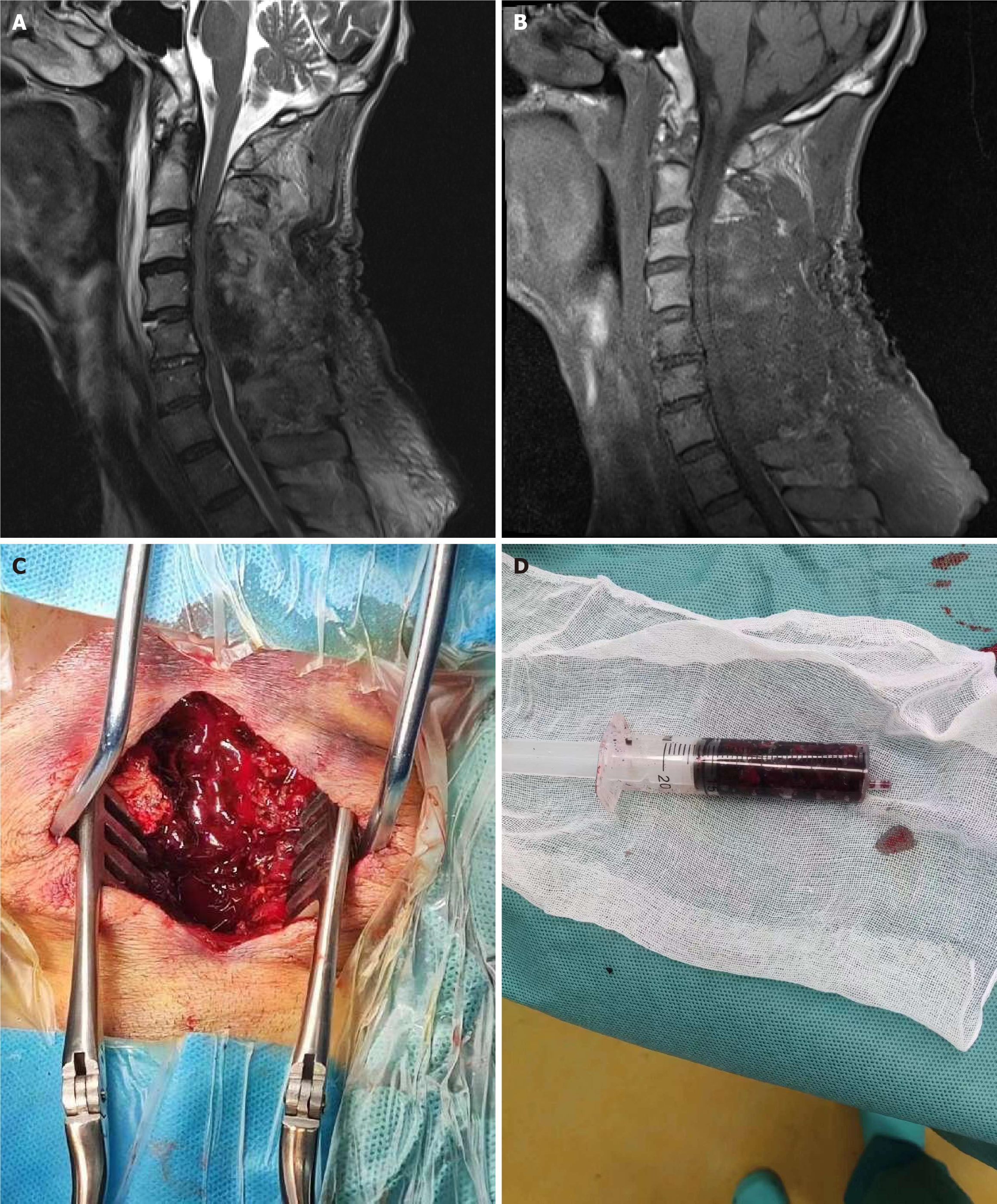
Anteroposterior and lateral X-ray images showed a C4, C5 spinous process fracture. Cervical computed tomography revealed a C4 laminar fracture, and magnetic resonance imaging (MRI) revealed spinal stenosis of C3-C7 with spinal cord edema, a compressed spinal cord, and traumatic disc rupture and protrusion of C5/6 and C6/7 (Figure 1).
The clinical diagnosis was cervical spinal cord injury with tetraplegia (grade C), C4 laminar fracture, and C4, C5 spinous process fracture.
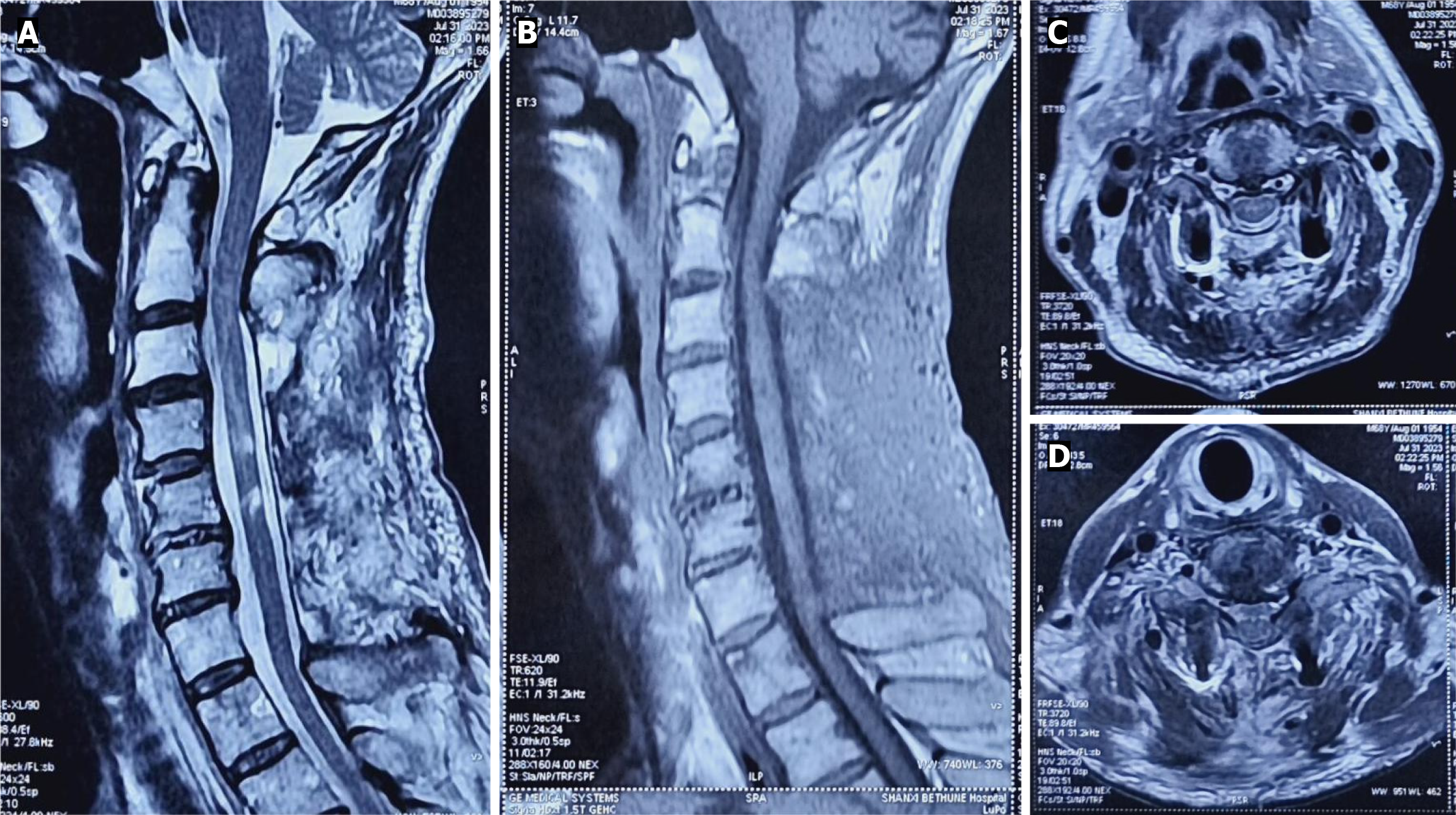
Ten days after hospitalization, the patient underwent a total laminectomy and lateral mass screw and rod fixation (C3-C7). The surgery was uneventful, with no excessive bleeding. Two negative pressure drains were placed in each wound. The blood pressure was 105/65 mmHg postoperatively, and the symptoms and physical examination results immediately after surgery were the same as those preoperatively. The two drains were removed three days after surgery as the output gradually decreased. On the same day, approximately 55 h after surgery, the patient experienced neck pain that was relieved in the lateral position. Subsequently, the patient suddenly lost muscle strength in the limb (grade 0). He further presented with subcutaneous swelling of the extremities, severe scrotal edema, and eyelid swelling. Emergency cervical MRI [T1- and T2-weighted imaging (WI)] revealed hypointense signals located behind the epidural space with a compressed spinal cord. Blood tests revealed a plasma albumin level of 24.2 g/L, and B-ultrasonography revealed pleural and pericardial effusion.
Emergency surgery was performed approximately 8 h following symptom onset, and a hematoma was identified between the epidural space and the posterior muscles (Figure 2). No active hemorrhages were observed. After complete evacuation of the hematoma, two drainage tubes were placed as close as possible to the dura mater. Negative vacuum pressure was applied for 10 min after wound closure. The two drainage tubes were removed on days 7 and days 8 postoperatively. The patient’s lower limb muscle strength recovered to grade 1 on the second day after hematoma evacuation and to grade 2 on the fourteenth day. Finally, the patient was transferred to the functional rehabilitation department.
On day 30, muscle strength of the left upper and lower limbs and motor weakness recovered to grade 3+, right upper and lower limbs to grade 2+, and internal muscles of the hand to grade 1. The epidural hematoma completely disappeared on MRI, and the central spinal cord revealed high signal intensity on T2WI (Figure 3).
Bleeding of the epidural venous plexus is a common cause of delayed SEH. However, the associated risk factors are complex, with preoperative risk factors including age > 60 years[7,8], RH-positive blood, hypertension[9], preoperative nonsteroidal anti-inflammatory drugs usage[8], coagulation dysfunction, and vascular anomalies[10]. Furthermore, vertebral hemangioma, multilevel surgery, surgical bleeding > 1000 mL, epidural procedures, and scar tissue have been identified as intraoperative risk factors. In another study, the last numerical value of international normalized ratio > 2.0 within 48 h, the postoperative hemoglobin value < 10 g/dL, the time for ventilator dependence > 48 h, early heparin treatment, and tension-related events such as sneezing, coughing, constipation, and sudden vigorous events were all considered as postoperative risk factors[11]. Other sources of hematoma include bone bleeding, a prepared fusion bed, instrument-irritating vascularized ligamentum flavum[12], and muscle bleeding. Additionally, some studies have reported that the deep cervical artery could be a source of delayed SEH[13,14]. Spinal manipulation therapy can also cause SEH[15]. However, so far, approximately a third of SEH cases have no clear etiology; and are thus classified as spontaneous SEH[16,17]. We reviewed all previously reported cases of SEH, and the characteristics of these cases are summarized in the Table 1.
| Ref. | Country | Sex/age (yr) | Diagnosis | Surgery | Main symptoms | Onset time | Location of bleed | Risk factor | Treatment | Outcome |
| Chung et al[8], 2020 | Malaysia | Female/76 | T11/12, stenosis, CSM | Decompression, fusion | Paraparesis | 4 d | T11/T12 | Unknown | Surgery | Recovery |
| Male/53 | Laminectomy and LMF C4-C6 | Tetraplegia | 4 d | C4-C6 | Unknown | Surgery | Recovery | |||
| Tomii et al[5], 2018 | Japan | Male/56 | CSM | C4-C6 UODL | Tetraplegia | 7 d | C4-C6 | Hypertension | Surgery | Recovery |
| Xu et al[9], 2022 | China | Male/86 | CDH | C3-C5 ACDF | Tetraplegia | 5 d | Behind disc | Unknown | Surgery | Die |
| Haghnegahdar et al[12], 2016 | Iran | Male/ 29 | Cervical locked facet. Subluxation | Poster fixation and fusion | Arm pain numbness | 11 yr | C3-C4 ligamentum flavum | Instrument irritation | Surgery | Recovery |
| Na and Khoo[16], 2023 | Singapore | Male/28 | Spontaneous SEH | / | Neck pain. Numbness | 2 d | C5-6 extradural | Unknown | Non surgery | Recovery |
| Koga et al[14], 2019 | Japan | Male/67 | CSM | CPL | Neck pain | 26 h | C3-6 epidural | Deep artery | Surgery | Recovery |
| Liu et al[15], 2021 | China | Female/30 | / | SMP | Neck pain | 3 d | C6-C7 | Unknown | Surgery | Recovery |
| Male/55 | / | SMP | Back pain | 1 d | T1-T3 | Unknown | Surgery | Recovery | ||
| Male/28 | / | SMP | Numbness | 4 h | T1-T2 | Unknown | Surgery | Recovery | ||
| Choi et al[13], 2013 | Korea | Male/65 | CSM | CPL | Shoulder arm pain | 30 months | C5-C7 Epi | Oozed bleeding | Surgery | Recovery |
| Khan et al[27], 2007 | United States | Male/55 | CSM | CPL | Spasms | 9 d | C3-7 Epi | Unknown | Surgery | Recovery |
| Female/58 | CSM | CPL | Spasms | 2 d | T1-2 Epi | Unknown | Surgery | Recovery | ||
| Female/66 | CSM | CPL | Spasms | 2 d | C4-5 Epi | Unknown | Surgery | Recovery | ||
| Alahmadi et al[20], 2022 | Magnolia | Female/67 | SSEDH | / | Neck pain and stiffness | 2 h | C3-7 Epi | Platelets dysfunction | Surgery | Recovery |
| Kim and Kuh[21], 2012 | Korea | Male/36 | CDH | ACDF | Headache hypertension | 30 months | C2-T5 Epi | Hypertension | Surgery | Recovery |
| Morse et al[18], 2007 | United States | Male/67 | DLS | PLIF | Left chest pain | 13 h | C4-S1 Epi | Anticoagulation therapy | Surgery | Recovery |
| Lee et al[11], 2010 | Korea | Male/60 | CDH | ACDF | Neck pain | 4 h | C1-T4 Epi | Coagulopathy | Surgery | Recovery |
| Fiani et al[17], 2021 | United States | Male/52 | SSEH | / | Upper back pain | / | C4-C7 Epi | Coagulopathy. Hypertension. Coagulopathy | Surgery | Recovery |
| Female/72 | SSEH | / | Neck pain | / | C3-T2 Epi | Surgery | Recovery | |||
| Carlhan-Ledermann et al[10], 2020 | Switzerland | Female/7 | SSEH | / | Neck pain | / | C2-T1 Epi | Vascular malformationVWF decrease | Surgery | Recovery |
| Male/4.5 | SSEH | / | Neck pain | / | C3-C5 Epi | No | Recovery | |||
| Jaweed et al[32], 2020 | United States | Male/42 | SSEH | / | Neck pain. Paraparesis | / | C3-C4 Epi | Unknown | Surgery | Recovery |
Coagulation disorders due to anticoagulant use have been indicated as a potential factor related to re-bleeding after surgery[16,18,19]. A study concluded that postoperative hematoma formation was related to anticoagulant therapy[20]. However, the relationship between anticoagulant use, as measured by activated partial thromboplastin time and re-bleeding after surgery, remains controversial. Hypertension is a known risk factor for the development of postoperative SEH[21]. However, a study reported that only patients with high postoperative systolic blood pressure had a 1.1-fold higher risk of developing hematomas compared to normal patients[22]. Patients usually present with high blood pressure after surgery due to wound pain. High postoperative blood pressure could lead to high whole blood viscosity that stimulates blood clots and plugs the drainage tube. As such, postoperative blood pressure should be monitored and hypertension should be controlled immediately.
The mechanisms underlying epidural hematomas are not yet completely understood. However, the venous vessel pressure theory may explain the impetus for postoperative SEH. One study previously reported that the epidural venous plexus is directly exposed to intrathoracic pressure, which balances the pressure/volume ratio in relation to the intracranial and intrathoracic pressure and volume change[23]. Increased thoracic pressure elevates the intraspinal venous system within the epidural space. High pressure in the epidural venous plexus would predispose a weakened epidural vein to rupture[24]. The patient in the present case presented with limb swelling and pleural effusion after the first operation due to hypoproteinemia. Prior studies have shown that an accumulation of pleural fluid causes gradual increases in thoracic pressure[25], while another study showed that this condition reduces venous return and accelerates massive blood flow reversal from the large caval system into the smaller epidural veins[25,26]. Considering these anatomical prerequisites in association with pleural effusion induced by hypoproteinemia, an increased venous pressure could lead to bleeding and hematoma formation, which extend along the posterior epidural space and compress the cervical spinal cord. In our case, neck pain and limb discomfort developed at night, without any predisposing factors such as coughing, straining, sneezing, or hypertension. This nocturnal development suggests that a relationship may exist between chest pressure and hemodynamic changes that may have caused the epidural hematoma.
The present case is unusual due to the presence of a slowly progressive hematoma that accumulated over several days, with mild neck pain and weakness as the primary complaints. Sometimes, the cause of pain or new neurological symptoms recognized immediately after initial surgery are uncertain, due to the retention of blood in the spinal surgery site[27]. In the present case, we found that the postoperative hematoma comprised a clot without blood. We presumed that the hematoma began to develop within a short period on the third postoperative day. MRI is considered as the gold standard diagnostic modality for hematoma[28], as it can demonstrate the specific features of hemorrhage, including an isointense signal on T1WI, a high signal on T2WI within 24 h, and increased signal intensity on both T1WI and T2WI after 24 h. Low-intensity signal images can also be observed in the hyperacute phase of the hematoma. In the present case, a MRI was performed immediately and showed isointense low signal intensity on T1WI and heterogeneous intensity on T2WI, with marked indentation on the dural sac, indicating a hematoma at the surgical site. Additionally, MRI is helpful for measuring the extent, volume, and location of hematoma. Merter and Shibayama[29] previously developed a new classification system for SEH using MRI based on the measurement of the dural sac area and used this system to determine the correlation between the symptoms of postoperative SEH and the compression of the dural sac area. This study indicated that the classification of postoperative SEH based on MRI could predict the clinical status; in other words, a narrower preoperative epidural area would indicate a better clinical outcome in patients with postoperative SEH.
Patients’ neurological recovery is related to their preoperative symptoms and the time interval to surgery[30,31]. Prominent symptoms lasting for several hours in cervical postoperative SEH are generally caused by the narrow spinal canal and the low tolerance of cervical neurological structures to the space-occupying effect of a forming hematoma. Therefore, differentiation from ischemic stroke and prompt surgery to clear the hematoma are key to ensure optimal outcomes in postoperative SEH patients[32]. In one related study, Bediwy et al[33] concluded that decompression surgery within 8 h could result in good neurological outcomes in patients with SEH. Similarly, Bakker et al[34] reported that the preoperative duration of paralysis was the only independent predictor of poor outcome; therefore, it is crucial to determine the neurological deficits and to shorten the interval time to evacuation surgery in patients following posterior cervical spine surgery.
Although delayed postoperative SEH following cervical spinal surgery is rare, clinicians should keep this diagnosis in mind to ensure prompt diagnosis and treatment. Meticulous correction of perioperative hypoproteinemia following cervical spine surgery is important to prevent delayed postoperative SEH.
The authors would like to thank professor Li Chun-De for his technical assistance.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Mahmoud MZ, Saudi Arabia S-Editor: Wang JJ L-Editor: A P-Editor: Zhao S
| 1. | Wang T, Tian XM, Liu SK, Wang H, Zhang YZ, Ding WY. Prevalence of complications after surgery in treatment for cervical compressive myelopathy: A meta-analysis for last decade. Medicine (Baltimore). 2017;96:e6421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 42] [Cited by in RCA: 53] [Article Influence: 6.6] [Reference Citation Analysis (0)] |
| 2. | Al Barbarawi MM, Allouh MZ. Cervical lateral mass screw-rod fixation: Surgical experience with 2500 consecutive screws, an analytical review, and long-term outcomes. Br J Neurosurg. 2015;29:699-704. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 14] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 3. | Chen G, Liu X, Zhao E, Chen N, Wei F, Liu S. Comparative Five-Year Surgical Outcomes of Open-Door versus French-Door Laminoplasty in Multilevel Cervical Spondylotic Myelopathy. Biomed Res Int. 2020;2020:8853733. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.6] [Reference Citation Analysis (1)] |
| 4. | Al Barbarawi MM, Allouh MZ, Qudsieh SM, Barbarawi A. Cervical decompressive laminectomy and lateral mass screw-rod arthrodesis: surgical experience and analytical review of 4120 consecutive screws. Br J Neurosurg. 2021;35:480-485. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (1)] |
| 5. | Tomii M, Mizuno J, Kazama K, Matsushima T, Watanabe K. Delayed Postoperative Spinal Epidural Hematoma after Cervical Laminoplasty. NMC Case Rep J. 2018;5:35-38. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 0.9] [Reference Citation Analysis (2)] |
| 6. | Aono H, Ohwada T, Hosono N, Tobimatsu H, Ariga K, Fuji T, Iwasaki M. Incidence of postoperative symptomatic epidural hematoma in spinal decompression surgery. J Neurosurg Spine. 2011;15:202-205. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 100] [Cited by in RCA: 121] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 7. | Awad JN, Kebaish KM, Donigan J, Cohen DB, Kostuik JP. Analysis of the risk factors for the development of post-operative spinal epidural haematoma. J Bone Joint Surg Br. 2005;87:1248-1252. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 158] [Cited by in RCA: 172] [Article Influence: 8.6] [Reference Citation Analysis (1)] |
| 8. | Chung WH, Tan RL, Chiu CK, Kwan MK, Chan C. Delayed Post-operative Spinal Epidural Haematoma after Posterior Spinal Surgery: Report of Two Cases. Malays Orthop J. 2020;14:170-173. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 9. | Xu W, Guo J, Zhu J, Zhao X, Yasaman I, Chen J, Wang J, Fan S, Fang X. Delayed postoperative spinal epidural hematoma after anterior cervical discectomy and fusion: A case report. Front Surg. 2022;9:1005462. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (1)] |
| 10. | Carlhan-Ledermann A, Laubscher B, Steinlin M, Ulrich CT, Verma RK, Rizzi M, Maduri R, Grunt S. Spinal epidural hematoma without significant trauma in children: two case reports and review of the literature. BMC Pediatr. 2020;20:77. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (1)] |
| 11. | Lee DY, Lee SH. Cervicothoracic spinal epidural hematoma after anterior cervical spinal surgery. J Korean Neurosurg Soc. 2010;48:541-543. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 9] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 12. | Haghnegahdar A, Sedighi M, Rahmanian A, Baghban F. Cervical Ligamentum Flavum Hematoma: A Case Report. Global Spine J. 2016;6:e30-e34. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 13. | Choi JH, Kim JS, Lee SH. Cervical spinal epidural hematoma following cervical posterior laminoforaminotomy. J Korean Neurosurg Soc. 2013;53:125-128. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 7] [Cited by in RCA: 11] [Article Influence: 0.9] [Reference Citation Analysis (0)] |
| 14. | Koga M, Hattori G, Maeda M, Nakamura Y, Miyagi T, Okura A, Morioka M, Uchikado H. Deep Cervical Artery as a Source of Bleeding in Postoperative Spinal Epidural Hematoma: A Case Report. NMC Case Rep J. 2019;6:87-90. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 15. | Liu H, Zhang T, Qu T, Yang CW, Li SK. Spinal epidural hematoma after spinal manipulation therapy: Report of three cases and a literature review. World J Clin Cases. 2021;9:6501-6509. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 2] [Cited by in RCA: 5] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 16. | Na XBM, Khoo SMK. Stroke-like manifestation of a spontaneous spinal epidural hematoma with spontaneous resolution: a case report. Int J Emerg Med. 2023;16:10. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 17. | Fiani B, Jarrah R, Fiani NJ, Runnels J. Spontaneous cervical epidural hematoma: Insight into this occurrence with case examples. Surg Neurol Int. 2021;12:79. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 7] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 18. | Morse K, Weight M, Molinari R. Extensive postoperative epidural hematoma after full anticoagulation: case report and review of the literature. J Spinal Cord Med. 2007;30:282-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 23] [Cited by in RCA: 24] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Yi S, Yoon DH, Kim KN, Kim SH, Shin HC. Postoperative spinal epidural hematoma: risk factor and clinical outcome. Yonsei Med J. 2006;47:326-332. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 118] [Cited by in RCA: 127] [Article Influence: 6.7] [Reference Citation Analysis (0)] |
| 20. | Alahmadi MJ, Almolky KS, Rezai DM. Spontaneous Spinal Epidural Hematoma Associated With Short-Term Dual Antiplatelet Therapy: A Case Report. Cureus. 2022;14:e29415. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 21. | Kim JS, Kuh SU. Immediate Revision Surgery due to Post-Anterior Cervical Discectomy and Fusion (ACDF) Spinal Epidural Hematoma. Korean J Spine. 2012;9:111-113. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 22. | Wang L, Wang H, Sun Z, Chen Z, Sun C, Li W. Incidence and Risk Factors for Symptomatic Spinal Epidural Hematoma Following Posterior Thoracic Spinal Surgery in a Single Institute. Global Spine J. 2022;12:1175-1183. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 11] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 23. | Martin BA, Reymond P, Novy J, Balédent O, Stergiopulos N. A coupled hydrodynamic model of the cardiovascular and cerebrospinal fluid system. Am J Physiol Heart Circ Physiol. 2012;302:H1492-H1509. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 40] [Cited by in RCA: 42] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 24. | Abbott NJ, Pizzo ME, Preston JE, Janigro D, Thorne RG. The role of brain barriers in fluid movement in the CNS: is there a 'glymphatic' system? Acta Neuropathol. 2018;135:387-407. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 309] [Cited by in RCA: 390] [Article Influence: 55.7] [Reference Citation Analysis (0)] |
| 25. | Chen H, Chen K, Xu JQ, Zhang YR, Yu RG, Zhou JX. Intracranial pressure responsiveness to positive end-expiratory pressure is influenced by chest wall elastance: a physiological study in patients with aneurysmal subarachnoid hemorrhage. BMC Neurol. 2018;18:124. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 18] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 26. | Koutsoukou A, Katsiari M, Orfanos SE, Kotanidou A, Daganou M, Kyriakopoulou M, Koulouris NG, Rovina N. Respiratory mechanics in brain injury: A review. World J Crit Care Med. 2016;5:65-73. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 26] [Cited by in RCA: 35] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 27. | Khan MH, Lee JY, Donaldson WF, Kang JD. Epidural Hematoma Presenting with Severe Neck Pain without Neurological Deficit - A Late Complication of Posterior Cervical Spine Surgery: Presentation of Three Unusual Cases. Asian Spine J. 2007;1:57-60. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 2] [Cited by in RCA: 3] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 28. | Sarubbo S, Garofano F, Maida G, Fainardi E, Granieri E, Cavallo MA. Spontaneous and idiopathic chronic spinal epidural hematoma: two case reports and review of the literature. Eur Spine J. 2009;18:1055-1061. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 23] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 29. | Merter A, Shibayama M. A new classification for spinal epidural hematoma following microendoscopic decompressive laminotomy: A prospective clinical and magnetic resonance imaging study of 245 patients. Acta Orthop Traumatol Turc. 2020;54:596-603. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 2] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 30. | Graziani N, Bouillot P, Figarella-Branger D, Dufour H, Peragut JC, Grisoli F. Cavernous angiomas and arteriovenous malformations of the spinal epidural space: report of 11 cases. Neurosurgery. 1994;35:856-63; discussion 863. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 3] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 31. | Lunardi P, Mastronardi L, Lo Bianco F, Schettini G, Puzzilli F. Chronic spontaneous spinal epidural hematoma simulating a lumbar stenosis. Eur Spine J. 1995;4:64-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 16] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 32. | Jaweed M, Ganesan D, Yasin MA, Liew BS, Bin Rosman AK. Acute Spontaneous Cervical Spinal Epidural Haematoma a Very Rare Presentation Mimicking of Carotid Dissection during Sleep. Asian J Neurosurg. 2020;15:455-457. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 33. | Bediwy AS, Al-Biltagi M, Saeed NK, Bediwy HA, Elbeltagi R. Pleural effusion in critically ill patients and intensive care setting. World J Clin Cases. 2023;11:989-999. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Cited by in RCA: 6] [Article Influence: 3.0] [Reference Citation Analysis (5)] |
| 34. | Bakker NA, Veeger NJ, Vergeer RA, Groen RJ. Prognosis after spinal cord and cauda compression in spontaneous spinal epidural hematomas. Neurology. 2015;84:1894-1903. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 48] [Cited by in RCA: 64] [Article Influence: 6.4] [Reference Citation Analysis (0)] |