Published online Feb 26, 2024. doi: 10.12998/wjcc.v12.i6.1163
Peer-review started: November 5, 2023
First decision: December 15, 2023
Revised: December 25, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 26, 2024
Processing time: 106 Days and 23.3 Hours
Rectal prolapse arises from benign etiology. When symptoms of internal intussusception mirror those of rectal prolapse, a misdiagnosis is possible, especially under limited clinical presentation. It is crucial to recognize and differentiate rectal prolapse from internal intussusception because the two diagnoses have different prognoses. Here, we describe a case of adult sigmoid intussusception presenting as rectal prolapse.
A 64-year-old woman with no known medical history visited a gastrointestinal outpatient department due to hard bloody stool defecation for 1 wk followed by constipation for 3 d. Colonoscopy revealed a huge polypoid ulcerated tumor at the sigmoid colon with lumen stenosis. The patient was admitted due to post-procedural dull abdominal pain. Due to failed colonoscopy reduction and stent insertion, the patient underwent sigmoid colon resection with primary end-to-end anastomosis, with the transverse colostomy pathological report showing adeno
Presentation and manifestation of sigmoid intussusception may resemble that of rectal prolapse, necessitating careful observation due to distinct prognostic implications.
Core Tip: This case underscores the potential for sigmoid intussusception to bear a resemblance to rectal prolapse. These two diagnoses have distinct etiologies and treatment. Adults and children have different etiological factors. Sigmoid intussusception related to malignancy leads to an unfavorable outcome, whereas rectal prolapse has a better prognosis. A comprehensive literature review was conducted to elucidate the advantages and disadvantages of preoperative reduction.
- Citation: Tsai TJ, Liu YS. Adult sigmoid intussusception resembling rectal prolapse: A case report. World J Clin Cases 2024; 12(6): 1163-1168
- URL: https://www.wjgnet.com/2307-8960/full/v12/i6/1163.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i6.1163
Rectal prolapse occurs more frequently in elderly females, and a large rectal mass may not undergo spontaneous reduction. Symptoms of internal intussusception may bear a resemblance to rectal prolapse. In acute clinical scenarios, a paucity of the medical history may result in misdiagnosis. The prognosis of the two is different; so, recognition and differentiation are of the utmost importance. In this article, we describe a case of adult sigmoid intussusception presenting as rectal prolapse.
Hard bloody stool defecation for 1 wk followed by constipation for 3 d.
A 64-year-old woman visited a gastrointestinal outpatient department due to hard bloody stool defecation for 1 wk followed by constipation for 3 d. A digital examination diagnosed the patient with a second-degree hemorrhoid. Laxative medication was prescribed to aid constipation. However, constipation persisted, and she visited the outpatient department again 2 d later. Abdominal X-ray, abdominal computed tomography, and colonoscopy were arranged on the same day. Sigmoid cancer was suspected. One day after the examinations, she visited the emergency department for dull lower abdominal pain, bloody mucus, and obstipation.
There was no remarkable history of past illness.
There was no personal or familial history of any specific disease.
The physical examination revealed tenderness in the lower quadrant of the abdomen. A digital rectal examination revealed rectal prolapse.
Laboratory tests revealed a normal white blood cell count of 4100/μL (normal range: 4000-91000/μL), normal neutrophil level of 58.1% (normal range: 39.4%-72.6%), and normal hemoglobin of 11.4 g/dL (12-15 g/dL).
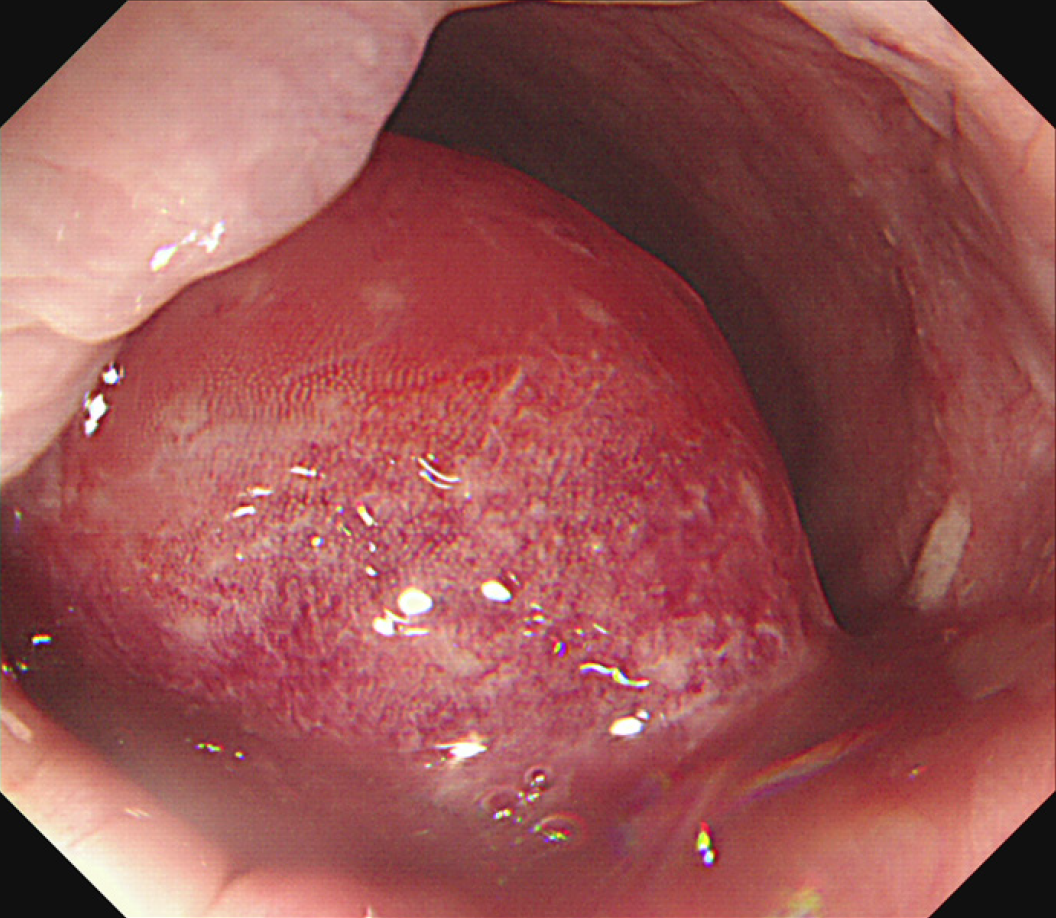
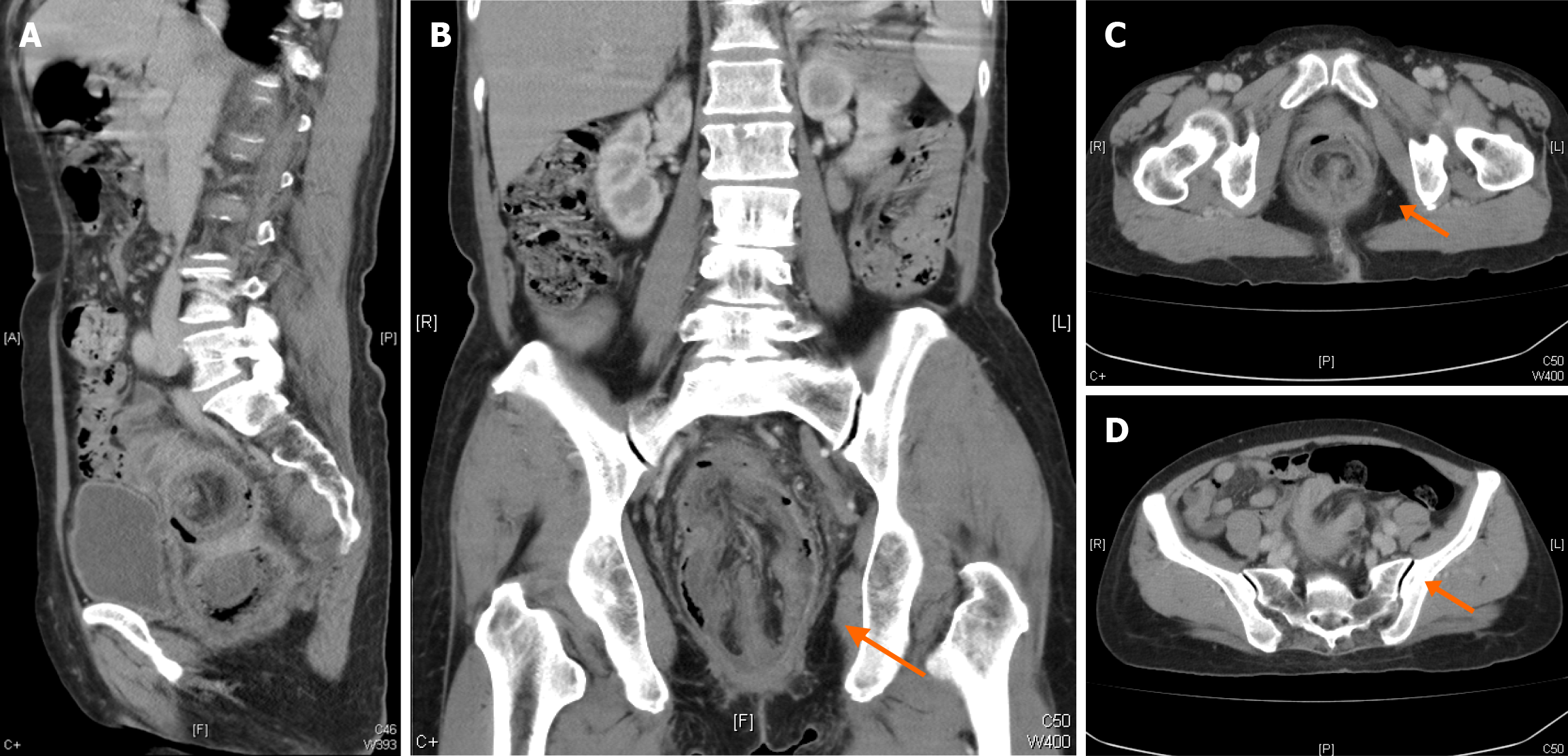
An abdominal X-ray showed fecal impaction in the colon. However, the colonoscope could not be advanced beyond about 15 cm from the anal verge. A huge polypoid ulcerated tumor with lumen stenosis was seen at the sigmoid colon, estimated to be 4 cm from the rectum (Figure 1). Abdominal computed tomography demonstrated sigmoid intussusception with inner irregular soft tissue (Figure 2).
Sigmoid intussusception resembling rectal prolapse.
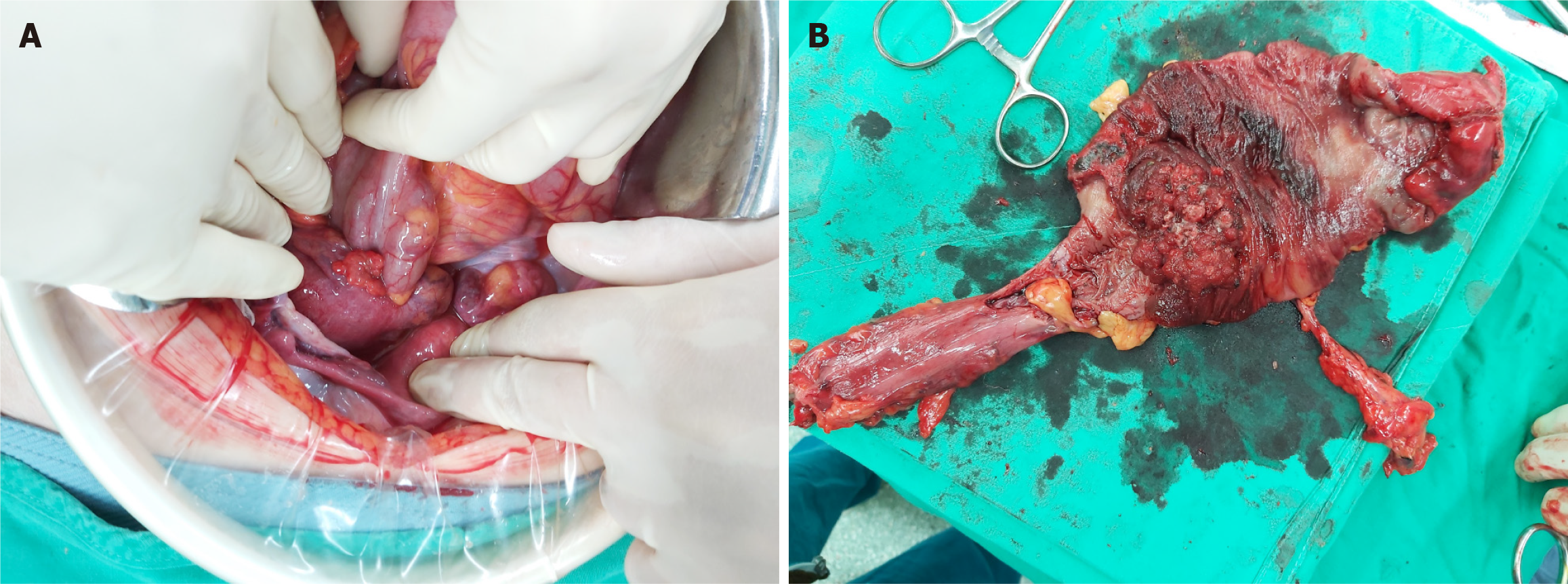
After discussion with the patient and her family, we established their expressed preference for nonsurgical treatment. Hence, we attempted colonoscopic reduction with stent insertion 2 d after admission. Colonoscopy treatment failed; so, a surgical approach was taken. Laparotomy for sigmoid colectomy with primary anastomosis was carried out. Intraoperative reduction of the prolapsed intussusception was not achieved by either the manual method or rectum dilator (Courtesy of Covidien, Inc., Norwalk, CT, United States) due to tense sigmoid intussusception with sigmoid cancer (Figure 3A). Distal resection under manual check via digital examination followed by primary end-to-end anastomosis with a transverse colostomy was performed (Figure 3B).
The patient recovered well post operation and was discharged on the 9th post-operative day. The pathology report confirmed a 5.1 cm adenocarcinoma, pT3NOMO, with KRAS Wild Type. The patient recovered and has returned to the outpatient clinic for close follow-up.
In comparison to its occurrence in children, adult intussusception is a rare condition. Pediatric intussusception is predominantly located in the small intestine, with 80%-90% of cases being idiopathic. By contrast, about half of adult intussusceptions occur in the large bowel, particularly in the right colon (70% of cases)[1]. Sigmoido-rectal intussusception is distinctly rare in the adult population.
Table 1[2-14] summarizes similar case reports that were published within the last 30 years. All cases involve sigmoid intussusception presenting as rectal prolapse. It is evident that sigmoido-rectal or sigmoido-anal intussusception are often misdiagnosed as rectal prolapse, especially when a detailed digital examination is not performed. Intussusception should be suspected after a tumor is observed. The classic triad of pediatric intussusception is paroxysmal abdominal pain, rectal bleeding, and abdominal palpable mass[15]. The symptoms of the classic triad are only observed in 9.8% of cases of adult intussusception. The clinical presentation of adult intussusception is nonspecific and chronic or subacute, presenting as intestinal obstruction (70.7%), abdominal pain (95.1%), bloody stool (26.8%), and a palpable abdominal mass (34.1%)[16,17].
| Ref. | Sex | Site of intussusception | Histopathology | Symptom | Reduction | Surgery |
| Younes et al[2], 1998 | F | Sigmoid | Lipoma | Rectal prolapse | Yes | Sigmoid colon resection, and rectopexy |
| Tony et al[3], 2007 | F | Colo-colonic | Lipoma | Rectal prolapse | No | External surgical resection |
| Chen et al[4], 2008 | M | Ileocolic | Lipoma | Abdominal pain, rectal prolapse | Yes | Subtotal colectomy |
| Ochiai et al[5], 2010 | F | Sigmoid | Adenocarcinoma | Abdominal pain, rectal prolapse | Yes | Intraoperative reduction and low anterior resection |
| Teyha et al[6], 2011 | M | Sigmoid | Idiopathic | Rectal prolapse | No | Sigmoid colon resection |
| Roy et at[7], 2011 | F | Sigmoid | Idiopathic | Rectal prolapse | Yes | Partial resection of the sigmoid colon |
| Elliott et al[8], 2014 | M | Sigmoid | Lipoma | Obstruction, rectal bleeding, rectal prolapse | Yes | Sigmoid colon resection |
| Mahmood et al[9], 2014 | M | Colo-colonic | Villous adenoma | Rectal prolapse, obstruction | Yes | Intraoperative reduction and sigmoid colon resection |
| Du et al[10], 2015 | F | Sigmoid-rectum | Tubulovillous adenoma | Obstruction, rectal bleeding, rectal prolapse | Yes | Total colectomy |
| West et al[11], 2019 | F | Sigmoid | Polyp | Rectal prolapse, hematochezia | No | Enterotomy and polypectomy |
| Mazumdar et al[12], 2021 | M | Sigmoid–rectum | Adenocarcinoma | Abdominal pain, rectal prolapse | No | Hartmann's procedure |
| West et al[13], 2022 | F | Sigmoid | Lipoma | Rectal bleeding, rectal prolapse | No | Hartmann's procedure |
| Penton et al[14], 2023 | M | Sigmoid | Adenocarcinoma | Rectal prolapse | Yes | Sigmoid colon resection |
Diagnosis is crucial, and a colonoscopy or sigmoidoscopy can provide insight into the potential underlying causes and obtain a specimen for histology. Computed tomography is considered superior because it can pinpoint the location and reveal the cause of the obstruction. In malignancy cases, computed tomography images provide more details of lymph nodes and metastasis status.
Treatment for adult colo-colonic or sigmoido-rectal intussusception is controversial. Sarr et al[18] investigated preoperative reduction due to malignant seeding risk. However, preoperative reduction can mean avoidance of emergent surgery or lesion survey and reduce the extent of intestinal resection and radical surgery for cancer. Though most cases of intussusception are related to lesions, few are idiopathic. In a recent study, preoperative endoscopy reduction was found to be more advantageous than emergent surgery because of the simultaneous diagnosis and treatment[17]. Moreover, endoscopy can provide a direct evaluation of the mucosal surface to determine the severity, such as ischemia or total obstruction or special intussusception. Laparoscopic reduction is feasible in idiopathic intussusception in adults. Radical resection is a priority for malignant cause. Rectal prolapse usually has a benign etiology, whereas sigmoido-rectal intussusception is mostly related to tumors.
Sigmoid intussusception in adults is mostly related to malignancy. Clinicians should be more cautious in differentiating between sigmoid intussusception and rectal prolapse based on limited presentation and medical history.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Surgery
Country/Territory of origin: Taiwan
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Jackson T, United States; Mehrvarz S, Iran S-Editor: Gong ZM L-Editor: Filipodia P-Editor: Zhao S
| 1. | Lambrou NA, Dunn WK, Robinson MH. Perineal resection of a sigmoid tumour presenting as colorectoanal intussusception: report of a case and review of the literature. Int J Colorectal Dis. 2006;21:286-287. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 2. | Younes ZH, Johnson DA, Dimick L. Sigmoido-anal intussusception presenting as rectal prolapse: role of endoscopic diagnosis. Gastrointest Endosc. 1998;47:561-563. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 7] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 3. | Tony J, Saji S, Sandesh K, Sunilkumar K, Ramachandran TM, Thomas V. External resection of a giant sigmoid lipoma causing colonic intussusception and prolapse through the anal canal. Trop Gastroenterol. 2007;28:127-128. [PubMed] |
| 4. | Chen R, Zhao H, Sang X, Mao Y, Lu X, Yang Y. Severe adult ileosigmoid intussusception prolapsing from the rectum: A case report. Cases J. 2008;1:198. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 9] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 5. | Ochiai H, Ohishi T, Seki S, Tokuyama J, Osumi K, Urakami H, Shimada A, Matsui A, Isobe Y, Murata Y, Endo T, Ishii Y, Hasegawa H, Matsumoto S, Kitagawa Y. Prolapse of Intussusception through the Anus as a Result of Sigmoid Colon Cancer. Case Rep Gastroenterol. 2010;4:346-350. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 10] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 6. | Teyha PS, Chandika A, Kotecha VR. Prolapsed sigmoid intussusception per anus in an elderly man: a case report. J Med Case Rep. 2011;5:389. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 5] [Article Influence: 0.4] [Reference Citation Analysis (1)] |
| 7. | Roy J, Gouda M, Reddy BS, Baker RP. Sigmoid intussusception presenting as rectal prolapse in an adult. Colorectal Dis. 2011;13:e385. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 8. | Elliott M, Martin J, Mullan F. Prolapsed giant sigmoid lipoma: a rare cause of adult ischaemic intussusception. BMJ Case Rep. 2014;2014. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 9. | Mahmood A, Ruan QZ, O'Hara R, Canna K. Adult intussusception presenting as rectal prolapse. BMJ Case Rep. 2014;2014:bcr2013203281. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 10. | Du JZ, Teo LT, Chiu MT. Adult rectosigmoid junction intussusception presenting with rectal prolapse. Singapore Med J. 2015;56:e78-e81. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 8] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 11. | West CT, Pilarski A, White D, Ricketts D. An intussuscepting colonic lipoma causing prolapse of the sigmoid colon in an adult. Br J Hosp Med (Lond). 2019;80:ii. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 12. | Mazumdar P, Kumar P, Katiyar G, Mulla M, Sardessai S. Sigmoid carcinoma with sigmoid-rectal intussusception presenting as rectal prolapse and large bowel obstruction in the ED. Egypt J Radiol Nucl Med. 2021;52:34. [RCA] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 13. | West J, Bellamy F, Smith B. Submucosal lipoma causing recto-sigmoid intussusception associated with an incidental gastrointestinal tumour. ANZ J Surg. 2022;92:1570-1572. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 14. | Penton AA, Jochum SB, Eberhardt JM. Unusual presentation of colon cancer as rectal prolapse in middle-aged male. Clin Case Rep. 2023;11:e6908. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 15. | Erkan N, Haciyanli M, Yildirim M, Sayhan H, Vardar E, Polat AF. Intussusception in adults: an unusual and challenging condition for surgeons. Int J Colorectal Dis. 2005;20:452-456. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 106] [Cited by in RCA: 115] [Article Influence: 5.8] [Reference Citation Analysis (0)] |
| 16. | Tarchouli M, Ait Ali A. Adult Intussusception: An Uncommon Condition and Challenging Management. Visc Med. 2021;37:120-127. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 11] [Cited by in RCA: 27] [Article Influence: 6.8] [Reference Citation Analysis (0)] |
| 17. | Wang N, Cui XY, Liu Y, Long J, Xu YH, Guo RX, Guo KJ. Adult intussusception: a retrospective review of 41 cases. World J Gastroenterol. 2009;15:3303-3308. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 142] [Cited by in RCA: 153] [Article Influence: 9.6] [Reference Citation Analysis (0)] |
| 18. | Sarr MG, Nagorney DM, McIlrath DC. Postoperative intussusception in the adult: a previously unrecognized entity? Arch Surg. 1981;116:144-148. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 30] [Article Influence: 0.7] [Reference Citation Analysis (0)] |