Published online Feb 26, 2024. doi: 10.12998/wjcc.v12.i6.1157
Peer-review started: November 3, 2023
First decision: January 5, 2024
Revised: January 11, 2024
Accepted: February 3, 2024
Article in press: February 3, 2024
Published online: February 26, 2024
Processing time: 108 Days and 20.6 Hours
There are very few cases of cardiac occluder detachment, and it is rare to com
The patient underwent left atrial appendage occlusion surgery in our hospital due to atrial fibrillation. After the surgery, the occluder fell off and became free in the left ventricle, which is very dangerous. We innovatively used ultrasound guidan
The size selection of the occluder is slightly conservative, and the shape of the left atrial appendage opening is irregular.
Core Tip: A case of successfully removing the detached left atrial appendage occluder using a catcher under the combined guidance of transthoracic ultrasound and digital subtraction angiography.
- Citation: Yu K, Mei YH. Left atrial appendage occluder detachment treated with transthoracic ultrasound combined with digital subtraction angiography guided catcher: A case report. World J Clin Cases 2024; 12(6): 1157-1162
- URL: https://www.wjgnet.com/2307-8960/full/v12/i6/1157.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i6.1157
Left atrial appendage occluder detachment is one of the most serious complications of left atrial appendage occlusion, but the incidence is low, and most treatment measures are removal after thoracotomy. In this case, we innovatively used ultrasound combined with digital subtraction angiography (DSA) guided percutaneous intervention surgery to successfully remove the detached occluder.
An 80-year-old man was admitted on September 1, 2023, two days after a sudden syncope.
The patient suddenly fainted and fell to the ground while standing up from the chair 9 days ago, with a facial landing and bleeding from a torn lip, accompanied by temporary loss of consciousness. After self relief, there was no obvious discomfort, no limb convulsions, no urinary and fecal incontinence, no foaming at the mouth, no headache or nausea and vomiting, and no palpitations or chest tightness before onset. Come to the emergency department of our hospital for treatment. The emergency blood pressure was measured at 98/56 mmHg, and the head computed tomography (CT) showed no bleeding and the electrocardiogram showed atrial fibrillation. Go home after being hospitalized in the neurology department for treatment. Now, in order to further treat heart disease, the patient has been readmitted to the cardiovascular department and diagnosed with coronary heart disease and atrial fibrillation.
Has a history of atrial fibrillation and medication is unknown. Have a history of gastric bleeding. Have a history of appendectomy.
Long term alcohol consumption, approximately 100 mL/d. Deny any history of infectious diseases such as hepatitis and tuberculosis, no history of trauma, no history of food or drug allergies, and no family history of hereditary diseases.
T 36.4 ℃, P 72 bpm, R 18 bpm, BP 145/72 mmHg. Clear consciousness, cooperative physical examination, clear respiratory sounds in both lungs, no dry or wet rales heard, heart rate 76 beats per minute, arrhythmia, atrial fibrillation rhythm. The abdomen is flat and soft, without tenderness or rebound pain, the liver and spleen are not large. There is no edema in both lower limbs. The muscle strength and tension of the limbs are normal, and the pathological signs are negative. Bilateral tendon reflexes exist symmetrically, without obvious sensory impairment, with a soft neck without resistance, and negative Kniger and Brucella signs on both sides.
Cardiac troponin I < 0.03 ng/mL; NT-proBNP: 4391.7 pg/mL.
After admission, a dynamic electrocardiogram showed: (1) Atrial fibrillation; (2) two hundred and thirty-seven premature ventricular contractions; and (3) four hundred and seventy-one long R-R intervals > 2.0 s, with a maximum of 3273 ms during the entire process.
Transthoracic echocardiography suggested: (1) Enlargement of the ascending aorta; (2) left atrial enlargement and right ventricular enlargement; (3) mild mitral regurgitation and moderate tricuspid regurgitation; and (4) arrhythmias.
(1) Cardiogenic syncope; and (2) persistent atrial fibrillation.
Considering that the patient had a history of gastrointestinal bleeding and a high risk of stroke and bleeding, left atrial appendage closure surgery was planned after the team was able to communicate with the patient and his family members.
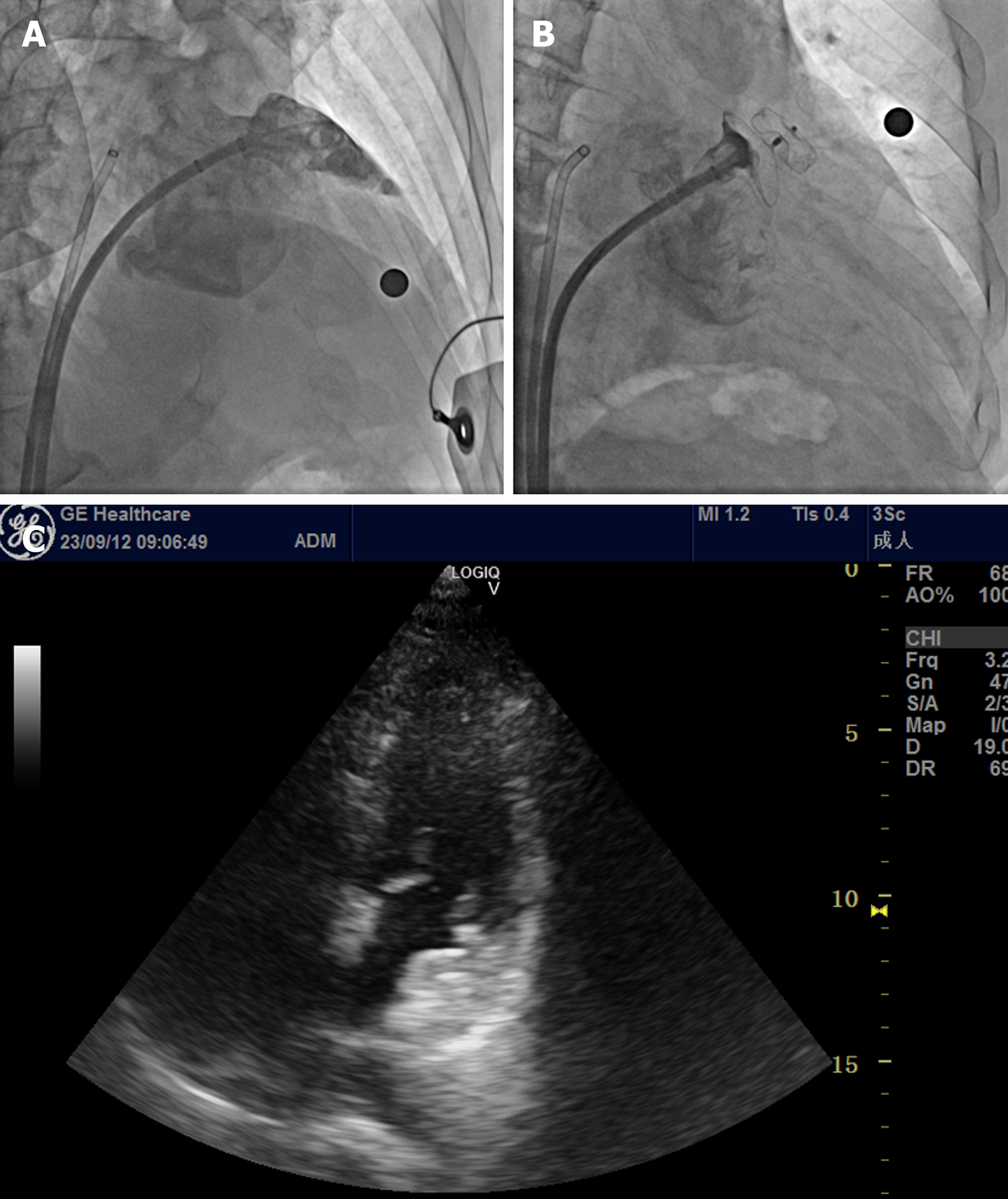
At 08:00 am on September 12, 2023, the surgery was performed under the guidance of DSA and transthoracic echocardiography. After a successful atrial septal puncture, the pigtail catheter was sent along the outer sheath to the left atrial appendage for an imaging examination (Figure 1A). The inner diameter and opening diameter of the left atrial appendage were measured, and LACbes 22 mm were configured in vitro according to the size of the patient's left atrial appendage × 32 mm of the occluded left atrial appendage. Under radiographic guidance, the occlusion was adjusted to the left atrial appendage, and with the assistance of RAOSO+CAU20 imaging, the occlusion umbrella was released. Radiography revealed that the occlusion umbrella was stable at the left atrial appendage opening, and the imaging showed that the left atrial appendage had been isolated from the left atrial blood flow (Figure 1B). A traction test was performed for another minute. RAOS0+CAU20 confirmed that the occlusion umbrella was firmly fixed, and there was no obvious leakage of contrast agent around the umbrella. The occlusion was, accordingly, considered satisfactory. Cardiac ultrasound examination showed that the occlusion umbrella was stably fixed at the opening of the left atrial appendage, and no blood flow signal was observed from the left atrial appendage or left atrium around the umbrella (Figure 1C), indicating successful occlusion of the left atrial appendage. Under radiographic guidance, the separation and delivery system, and the sealing umbrella were separated. Postoperatively, the patient's vital signs were stable, and the puncture point was ligated with sheath removal and pressure. The patient returned to the ward safely.
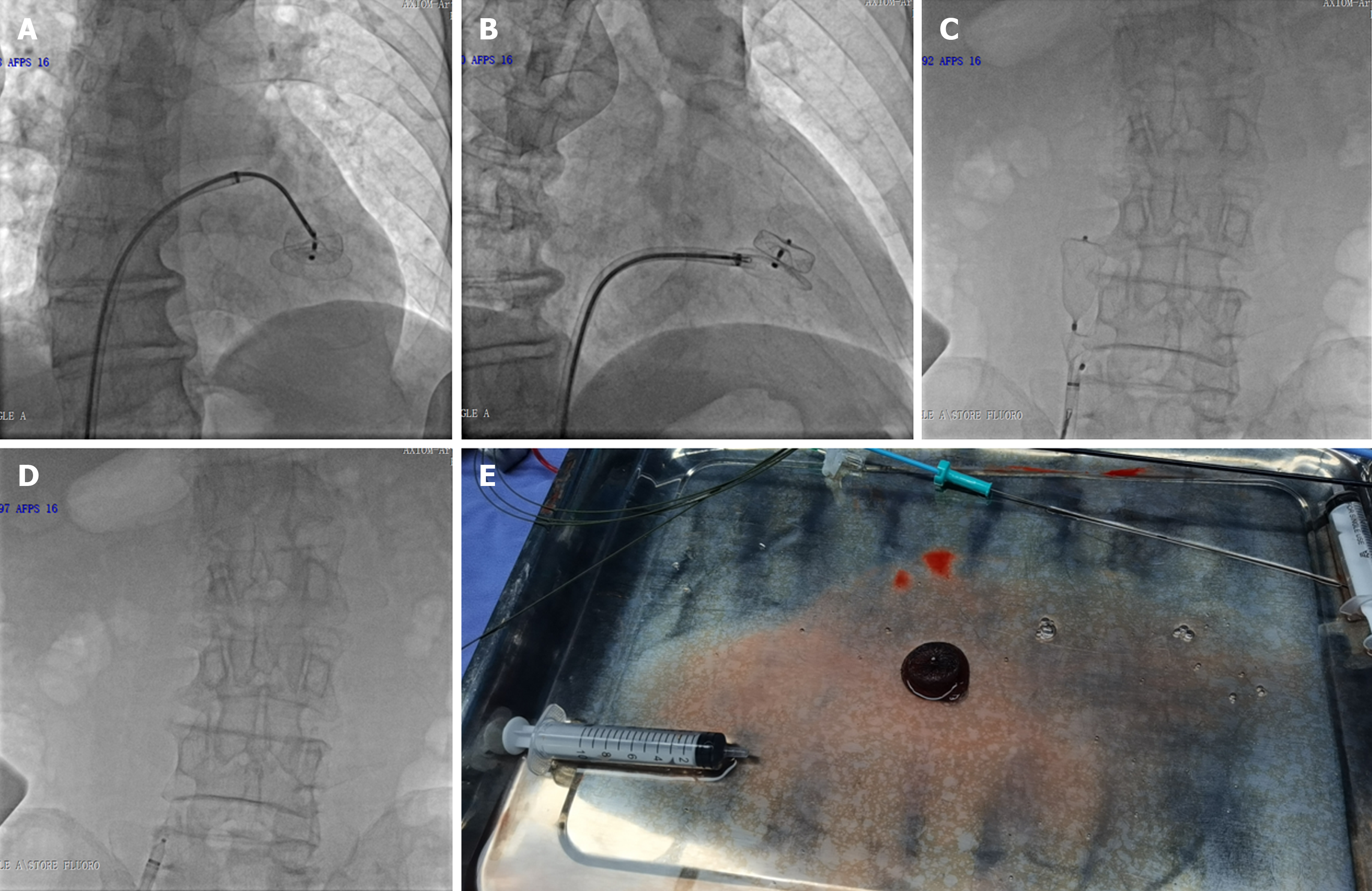
At 9:37 am on September 13, 2023, the patient visited the ultrasound imaging department for a follow-up cardiac ultrasound examination, which showed that the occluder had fallen off and was free in the left ventricle (Figure 2). CT confirmed this finding. After consultation with the superior hospital staff, the left atrial appendage occluder was removed and a left atrial appendage occlusion was performed at 18:35 on the same day. After a successful atrial septal puncture, a Medtronic 4FC12 adjustable sheath was inserted, followed by a 7F AL1 guide tube to the left ventricle along the adjustable bent sheath. The occluder grasping device was inserted along the guide tube, and the occluder was grasped under ultrasound guidance and X-ray fluoroscopy (Figure 3A). After successfully capturing the occluder, ice saline was injected along the adjustable curved sheath to soften the occluder (Figure 3B), and it was grabbed successfully by the sheath (Figure 3C and D). The occluder was successfully removed (Figure 3E), and the patient's vital signs were stable without any special discomfort reported. In this way, an in vitro configuration LACbes 26 mm × 32 mm left atrial appendage occlusion was performed. Under radiographic guidance, the occlusion umbrella was adjusted to the left atrial appendage, and with the assistance of RAOS0+CAU20 imaging, the occlusion was released. Radiography revealed that the occlusion was stable at the left atrial appendage opening, and the imaging showed that the left atrial appendage was isolated from the left atrial blood flow. A traction test was performed for another minute. RAOS0+CAU20 confirmed that the occlusion was fixed and there was no obvious leakage of contrast agent around the umbrella, indicating the satisfactory completion of the surgery.
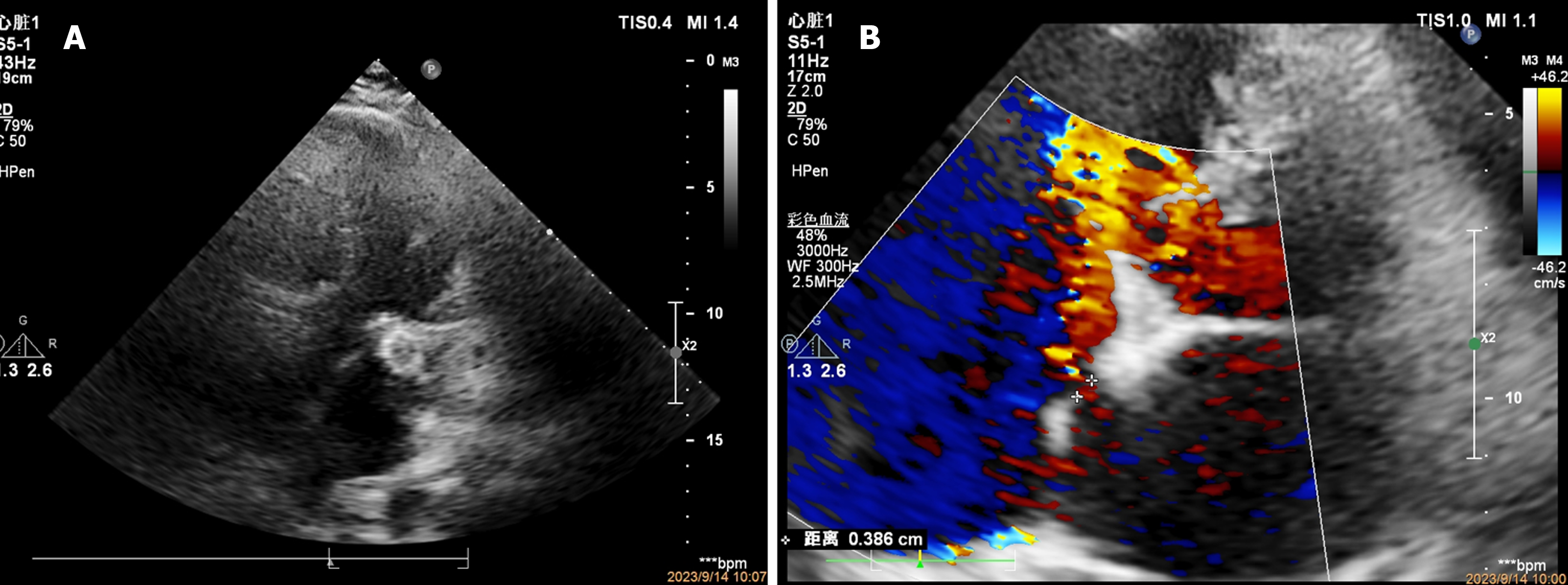
After a cardiac ultrasound examination conducted immediately postoperatively, it was evident that the closure umbrella was stably fixed at the left atrial appendage opening. No blood flow signal was observed from the left atrial appendage or left atrium around the umbrella. There was a small amount of mitral regurgitation, a small amount of septal blood flow was observed in the middle of the atrial septum, and no fluid accumulation was obvious in the pericardial cavity, indicating successful closure of the left atrial appendage. Under radiographic guidance, the conveying system and sealing umbrella had been separated. Postoperatively, the patient's vital signs were stable, and the puncture point of the pressure package was removed. The patient returned to the ward safely.
The next morning, a follow-up cardiac ultrasound was performed, and the closure umbrella was stably fixed at the left atrial appendage opening (Figure 4A). Mild mitral regurgitation was observed, and a shunt signal with a width of approximately 4mm was observed at the atrial septal puncture site (Figure 4B).
The left atrial appendage is the most prone site for atrial thrombus formation during atrial fibrillation, and stroke is among the most common complications of atrial fibrillation[1]. This patient with atrial fibrillation had a history of gastric bleeding and was unwilling to receive long-term oral anticoagulant therapy. After a multidisciplinary consultation, and after hearing the opinions of the patient and his family, left atrial appendage closure surgery was performed. An unpredictable occluder detachment occurred postoperatively.
The detachment of occluders is among the most serious complications of left atrial appendage closure surgery, but the incidence is low. Not many cases have been reported at home and abroad[2], and most remedial measures are thoracotomy and removal. In this case, ultrasound combined with DSA-guided percutaneous intervention was used to successfully remove the detached occluder[3].
The method used is as follows: under ultrasound guidance, the occluder was clamped and fixed in the left ventricle using toothed forceps in the occluder, and ice saline was injected into the sheath to fully soften the occluder. After fully softening the occluder, it was pulled into the sheath as much as possible, and withdrawn through the mitral valve, left atrium, atrial septum, right atrium, and inferior vena cava.
The surgical approach is summarized as follows: (1) Fully softening the occluder with ice saline is the key step of the entire surgery; (2) transthoracic ultrasound combined with DSA guidance is an important means of quickly capturing the occlude; (3) during the process of grasping and capturing the occluder, toothed forceps should be selected, but physical damage to structures such as the valves, tendons, or myocardium, must be avoided; (4) it is necessary to immediately evaluate the mechanical damage to structures such as the mitral valve and atrial septum using ultrasound after removing the original sealing device; and (5) finally, the detachment of the occluder may be caused by the irregular shape of the left atrial appendage opening and the slightly conservative size selection of the occluder.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Radiology, nuclear medicine and medical imaging
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Boffano P, Italy S-Editor: Liu JH L-Editor: A P-Editor: Cai YX
| 1. | Chinese Society of Cardiology of Chinese Medical Association; Editorial Board of Chinese Journal of Cardiology. [2019 Chinese Society of Cardiology (CSC) expert consensus statement on left atrial appendage closure in the prevention of stroke in patients with atrial fibrillation]. Zhonghua Xin Xue Guan Bing Za Zhi. 2019;47:937-955. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 2] [Reference Citation Analysis (0)] |
| 2. | Fastner C, Lehmann R, Behnes M, Sartorius B, Borggrefe M, Akin I. Veno-venous double lasso pull-and-push technique for transseptal retrieval of an embolized Watchman occluder. Cardiovasc Revasc Med. 2016;17:206-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 3. | Meng W, Zheng Y, Ren Z, Yang H, Li S, Zhao D, Chen W, Zhu M, Liu W, Zhang Y, Xu Y. A case of left atrial appendage occluder detachment treated with double sheath tube combined with double foreign body forceps. Zhonghua Xin Xue Guan Bing Za Zhi. 2022;50:817-818. [RCA] [DOI] [Full Text] [Reference Citation Analysis (0)] |