Published online Feb 26, 2024. doi: 10.12998/wjcc.v12.i6.1150
Peer-review started: October 15, 2023
First decision: December 15, 2023
Revised: December 26, 2023
Accepted: January 22, 2024
Article in press: January 22, 2024
Published online: February 26, 2024
Processing time: 127 Days and 22.5 Hours
Giant congenital biliary dilation (CBD) is a rare condition observed in clinical practice. Infants born with this condition often experience a poor overall health status, and the disease progresses rapidly, leading to severe biliary obstruction, infections, pressure exerted by the enlarged CBD on abdominal organs, distur
Herein, we present the details of an 11-d-old male newborn who was diagnosed with giant CBD. The patient was admitted to the neonatal surgery department of our hospital due to a history of common bile duct cyst that was detected more than 3 mo ago, and also because the patient had been experiencing yellowish skin for the past 9 d. The abnormal echo in the fetal abdomen was first noticed by the patient’s mother during a routine ultrasound examination at a local hospital, when the patient was at 24 wk + 6 d of pregnancy. This finding raised concerns about the possibility of congenital biliary dilatation (22 mm × 21 mm). Subsequent ultrasound examinations at different hospitals consistently confirmed the presence of a congenital biliary dilatation. No specific treatment was administered for biliary dilatation during this period. A computed tomography scan conducted during the hospitalization revealed a large cystic mass in the right upper quadrant and pelvis, measuring approximately 9.2 cm × 7.4 cm × 11.3 cm. Based on the scan, it was classified as a type I biliary dilatation.
The analysis reveals that prenatal imaging techniques, such as ultrasound and magnetic resonance imaging, play a crucial role in the early diagnosis, fetal prognosis, and treatment plan for giant CBD. Laparoscopic surgery for giant CBD presents certain challenges, including difficulties in separating the cyst wall, anastomosis, and hemostasis, as well as severe biliary system infection and ulceration. Consequently, there is a high likelihood of converting to laparotomy. The choice between surgical methods like hepaticojejunostomy (HJ) or hepaticoduodenostomy has not been standardized yet. However, we have achieved favorable outcomes using HJ. Preoperative management of inflammation, biliary drainage, liver function protection, and supportive treatment are particularly vital in improving children’s prognosis. After discharge, it is essential to conduct timely reexamination and close follow-up to identify potential complications.
Core Tip: Clinically, giant congenital biliary dilation (CBD) is a rare condition compared to ordinary CBD. There are numerous research articles discussing surgical treatment options for common CBD. The choice of specific surgical method should be based on the individual circumstances of the hospital, the child, and the family members. In our case report, we present the experience of treating a very young child (11 d old) with a significantly dilated biliary tract. The overall condition of the child before the operation was critical. During laparoscopic biliary reconstruction, we encountered a thin and ulcerated cyst wall, making separation and bleeding control challenging. Therefore, we opted for an open laparotomy and performed a Roux-en-Y anastomosis between the common hepatic duct and jejunum. Taking into consideration the analysis of similar cases indexed in PubMed, we suggest that open surgery is more advantageous than laparoscopic treatment for children with giant CBD who are in critical condition and have severe biliary tract distortion.
- Citation: Quan DW, Li PG, Xu XH, Liu SQ. Giant bile duct dilatation in newborn: A case report. World J Clin Cases 2024; 12(6): 1150-1156
- URL: https://www.wjgnet.com/2307-8960/full/v12/i6/1150.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i6.1150
Congenital biliary dilation (CBD) is a common developmental malformation of the biliary system in newborns. It predominantly occurs in childhood, with a higher incidence in females and Asians compared to males and Caucasians[1,2]. Advancements in prenatal diagnostic technologies, such as B-ultrasound and magnetic resonance imaging (MRI), have enabled the diagnosis of CBD in some children during the fetal period[3-6]. CBD is associated with numerous serious complications, necessitating early surgical intervention following a clear diagnosis[7]. In this report, we present a case of a newborn with giant CBD, characterized by a young age, a large cyst, and significant anatomical variations in abdominal organs. The surgical treatment of this case posed significant challenges. We provide a summary of the diagnosis and treatment experience with this baby and conduct a review of relevant literature.
An 11-d-old Chinese male infant with a weight of 2.84 kg was admitted to the neonatal surgery department of our hospital due to obvious abdominal distension, vomiting and jaundice for 9 d.
Abnormal abdominal echo was found for the first time during the routine ultrasound examination of the mother at the local hospital during pregnancy (24 wk + 6 d), suggesting that the possibility of congenital biliary dilatation (22 mm × 21 mm) is high, and it is recommended to refer to a higher-level hospital. During the period, ultrasound examinations in different hospitals revealed congenital dilation of the biliary tract, and no special treatment was performed. Cesarean section was performed at 37 wk + 5 d of pregnancy, with a birth weight of 3.05 kg. Nine days ago, the child’s skin and sclera were found to be yellow-stained and he vomited yellow-white stomach contents 7 to 8 times a day which was accompanied by crying, no fever, and the defecation of yellow stool. Parents were referred to our hospital for further treatment.
No other medical conditions have been identified in the past.
The patient denied any family history of similar diseases and had no other special medical history.
On physical examination, the vital signs were as follows: Body temperature, 36.5 °C; blood pressure, 85/50 mmHg; heart rate, 108 beats per min; respiratory rate, 28 breaths per min. Furthermore, the skin and sclera exhibited jaundice throughout the body, accompanied by a palpable soft mass in the right upper quadrant.
The abnormal laboratory test indicators observed after admission suggest that the child’s overall condition is poor: Liver function: Total bilirubin: 300.0 μmol/L, direct bilirubin: 174.90 μmol/L, total protein: 62.3 g/L, aspartate aminotransferase: 77 U/L, serum alkaline phosphatase: 163 U/L, glutamyl transpeptidase: 473 U/L; electrolyte: Carbon dioxide (CO2): 30.5 mmol/L, K+: 6.08 mmol/L, Na+: 110.2 mmol/L, Cl-: 59.7 mmol/L, Ca2+: 2.32 mmol/L; renal function: Urea: 16.69 mmol/L, Cr: 67 μmol/L, uric acid: 408 μmol/L, CO2: 20.7 mmol/L; blood routine: White blood cells 26.70 × 109, neutrophils (NEUT): 15.58 × 109, percentage of NEUT: 58.3%; high-sensitivity C-reactive protein: 8.06 mg/L; blood ammonia: 90.00 μmol/L; routine urine and stool analysis showed no abnormalities.
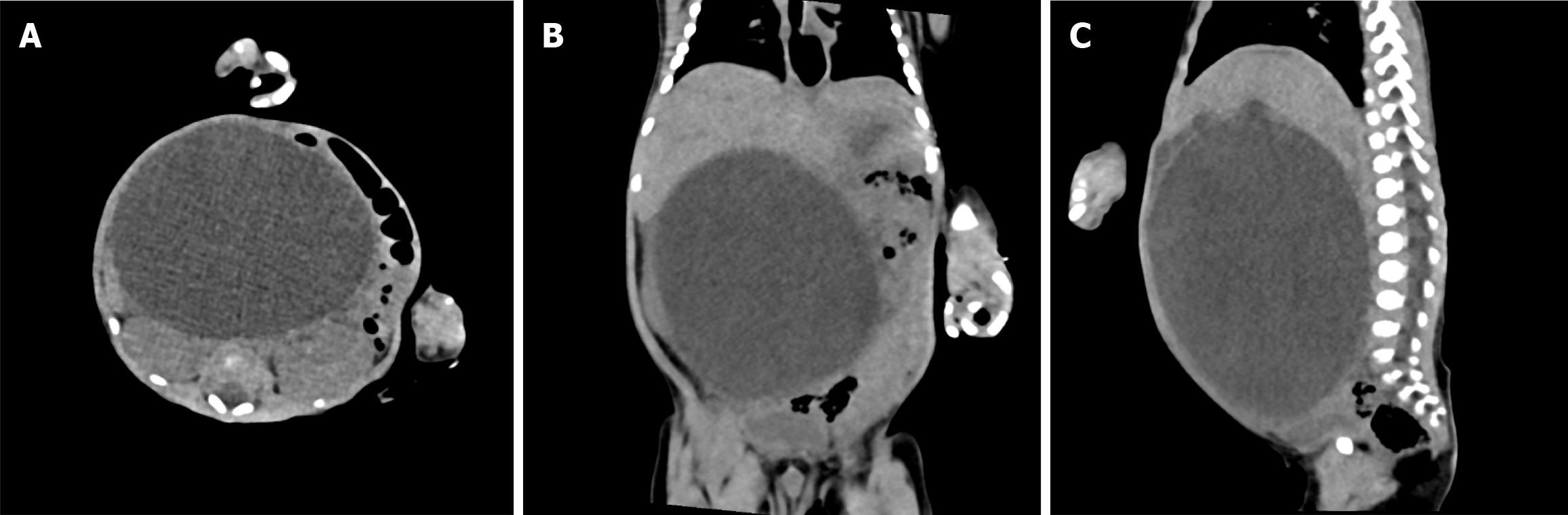
Abdominal computed tomography (CT) examination conducted after admission revealed a large cystic mass located in the right upper quadrant and pelvis (Figure 1). The mass was identified as a type I biliary dilatation, with dimensions measuring approximately 9.2 cm × 7.4 cm × 11.3 cm. Prior to the surgery, contrast agent was injected through the choledochal cyst drainage tube and an X-ray was taken, which confirmed the presence of a significant cystic dilatation in the common bile duct, with visualization of a portion of the common hepatic duct (Figure 2).
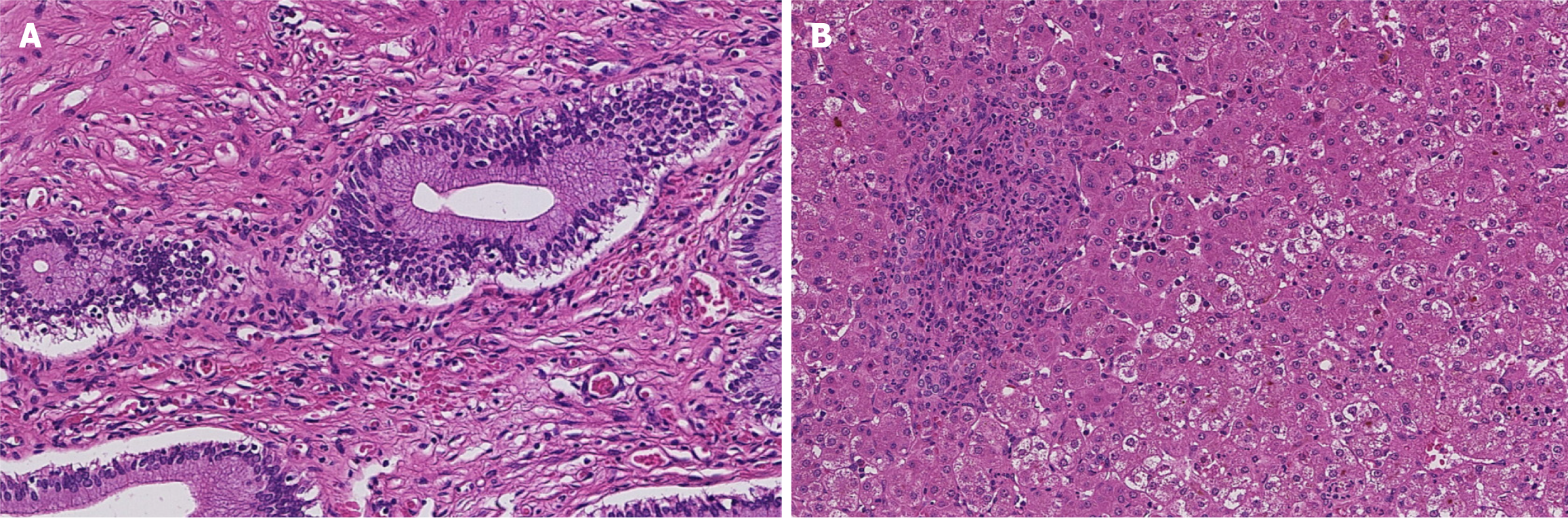
Combined with the child’s medical history, clinical manifestations, imaging and pathological examination results (Figure 3), the final diagnosis was CBD.
Considering the child’s initial poor general condition upon admission, immediate surgical treatment was not possible. Therefore, the child was initially provided with symptomatic and supportive treatment, including anti-infection measures, biliary drainage, electrolyte supplementation, coagulation factor supplementation, and albumin infusion. This treatment was continued for a duration of 15 d, and surgical treatment was subsequently performed once the child’s basic condition had stabilized.
Surgical procedure: In the initial laparoscopic exploration, it was observed that the common bile duct was dilated and cystic, exhibiting severe edema and congestion in the cyst wall. Subsequently, the cyst was incised and decompressed, revealing multiple green ulcers tightly adhering to the cyst wall, which posed challenges in their separation. Notably, when attempting to separate the middle part of the posterior wall of the cyst, significant bleeding occurred, making the separation process difficult. As a result, the decision was made to convert the operation to open surgery.
We used Roux-en-Y anastomosis technique, the common bile duct and jejunum were connected. The jejunum was then cut off, with a 20 cm gap from the ligament of Treitz. The distal port was closed, while ensuring that there was no tension on the mesentery. The hepatic branch was lifted through the colon and joined end-to-side with the common bile duct. The anastomotic stoma had a width of 1.5 cm. The proximal port of the jejunum was anastomosed end-to-side with the biliary branch, 15 cm away from the anastomosis stoma of the common bile duct.
Following the placement of an abdominal drainage tube and confirming the absence of active bleeding and leakage, a small tissue sample was taken from the edge of the liver for biopsy. Electrocoagulation was performed to stop any bleeding, the abdominal cavity was closed, and the wound was bandaged. The operation was successfully completed.
The patient recovered well after surgery, and there were no recent complications such as wound infection, incisional hernia, massive bleeding, biliary fistula, pancreatic fistula, intestinal fistula, peritonitis, etc. After 6 mo of follow-up, no long-term complications such as adhesive intestinal obstruction, anastomotic stricture, cholangitis, pancreatitis, biliary stones, or reflux esophagitis were found.
The causes and mechanisms of CBD-related pathogenesis have not yet been fully elucidated. The prevailing view suggests that an abnormal pancreaticobiliary junction leads to reflux of pancreatic juice, resulting in damage to the bile duct, destruction of the bile duct intima, and fibrosis. These factors contribute to fetal biliary dilatation. Some scholars also propose that congenital biliary dysplasia caused by certain genetic factors is an important cause of CBD[8]. CBD is predominantly observed in infants and young children and may manifest as abdominal distension, jaundice, high fever, vomiting, pale stools, and impaired liver function. According to the Todani classification, CBD can be divided into types I to V, with type I being the most common clinically. At present, the surgical treatment methods with the largest number of reports in domestic and foreign literature are mainly laparoscopic hepaticojejunostomy and hepaticoduodenostomy. A few qualified centers have been able to complete the corresponding surgery with the assistance of robots. For some special cases, whether using laparoscopy or robot-assisted surgery, it is necessary to convert to laparotomy for treatment.
Prenatal imaging technologies such as ultrasound and MRI play an important role in the early diagnosis of fetal congenital malformations, fetal prognosis and treatment options. With the continuous development and application of ultrasound technology in routine prenatal examinations of pregnant women, the detection rate of CBD has gradually increased. The first suspicion of common bile duct dilatation in this child was discovered during a routine physical examination by his mother. When performing prenatal ultrasound examination, it is necessary to make a reasonable judgment based on the characteristics of ultrasound imaging, and pay attention to the differentiation from other congenital diseases of the fetal abdomen, such as liver cysts, biliary atresia, ovarian cysts, etc.
The prenatal imaging characteristics of CBD under ultrasound are mainly oval in shape, with a cystic ductal-like structure. They have a thin cyst wall and clear cyst fluid. The size of the cyst ranges from 1.4 to 3.0 cm and gradually increases with gestational age. There is no presence of blood, but there is an abundant blood flow around the cyst. Biliary atresia and CBD can be distinguished based on the presence of echo, the size of the echo, and whether the size of the echo increases over time. Small, anechoic cysts indicate biliary atresia, while if the cyst enlarges as the pregnancy progresses, it suggests dilation of the bile ducts[3-5]. According to Wu et al[6] the MRI imaging characteristics of CBD during the fetal period include the cyst being located above the lower edge of the liver and connected with the intrahepatic bile duct. The researchers also evaluated the daily growth rate of choledochal cysts from the fetal to preoperative time and observed that the length, width, and size of the cyst may increase over time. They argue that prenatal MRI has a higher diagnostic accuracy for CBD compared to ultrasound because MRI is superior in depicting the cyst’s location and its relationship with the biliary tract[6].
After being diagnosed with CBD, it is recommended to perform surgery promptly in order to mitigate the negative impacts of the abnormal biliary tract in children. In the process of researching domestic and foreign literature on the diagnosis and treatment of CBD, it was found that the majority of articles are retrospective studies that investigate the effectiveness of conventional volume CBD reconstruction using various surgical techniques. These studies also examine the short-term and long-term complications associated with this approach. However, there is a limited number of case reports that specifically concentrate on neonatal giant CBD.
Yurttutan et al[9] reported a case study involving a child with a giant CBD, which bears some resemblance to the present case. The child in question was just 4 mo and 15 d of age, and the cyst height was measured to be over 16 cm, making it the largest volume recorded thus far. Prior to the surgery, ultrasound and CT scans were conducted as imaging examinations. The surgical approach employed was an abdominal common hepatic duct-jejunostomy Roux-en-Y anastomosis. The patient was discharged from the hospital 10 d after the operation. However, the article did not provide information regarding the incidence of postoperative complications or the mid- and long-term follow-up results in children[9]. The special features of our case reported in this article are as follows: (1) The child underwent surgery at the age of 28 d, which is younger than any other child with CBD reported so far; (2) In newborns who are only 11 d old, there is a huge bile duct with a height of 11 cm; and (3) The disease progressed rapidly within a short period after birth, causing significant compression of the intestines, spleen, and kidneys in the abdominal cavity. The child has the characteristics of young age, large cyst volume, acute onset, and critical condition. Based on the actual situation of the child, the reasons for conversion to laparotomy in this case were analyzed as follows: (1) The child had severe bile duct infection in the early stage, and the highest value of high-sensitivity C-reactive protein exceeded the normal range by more than 100 times, resulting in serious adhesion between the enlarged cystic wall and surrounding tissues which is not easy to separate under laparoscopy; (2) The cyst wall ulcer is seriously damaged, the cyst wall is thin, and it is difficult to anastomose under laparoscopy; (3) During the separation process under laparoscopy, bleeding cannot be effectively controlled; (4) The coagulation function is caused by hepatic insufficiency in children; (5) The volume of the cyst is giant (> 11 cm) occupying most of the abdominal cavity of the child; and (6) The child is young and the space in the abdominal cavity is limited, making the laparoscopic operation difficult. We consider that larger cysts in children may result in more significant distortion of the biliary system, thinner cyst walls, and increased compression of surrounding tissues and organs. Additionally, severe cholangitis can lead to adhesions, further complicating the laparoscopic biliary recon
The key to successful surgical reconstruction of the biliary system in children with giant CBD lies in providing comprehensive supportive treatment for the children prior to surgery. It is particularly crucial to address inflammation, correct internal environment disorders, improve coagulation function, and ensure proper nutrition. The selection of the specific reconstruction method should be based on the patient’s individual conditions and the expertise of different medical centers.
The disease progresses rapidly in children with giant CBD shortly after birth, and their overall condition is critical. Therefore, timely surgical treatment is necessary to improve the situation. Based on this case and the literature retrieved from PubMed, we recommend laparotomy as a treatment option due to its reliable efficacy and it being a relatively simple operation. Imaging examinations during the fetal period are also crucial for diagnosing and identifying CBD, enabling timely assessment and formulation of treatment plans.
Thanks to Professor Liu for his guidance and support in writing this article.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Varma V, India S-Editor: Wang JJ L-Editor: Filipodia P-Editor: Zhao S
| 1. | Urushihara N, Fukumoto K, Yamoto M, Miyake H, Takahashi T, Nomura A, Sekioka A, Yamada Y, Nakaya K. Characteristics, management, and outcomes of congenital biliary dilatation in neonates and early infants: a 20-year, single-institution study. J Hepatobiliary Pancreat Sci. 2018;25:544-549. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 19] [Article Influence: 2.7] [Reference Citation Analysis (0)] |
| 2. | Aly MYF, Mori Y, Miyasaka Y, Ohtsuka T, Sadakari Y, Nakata K, Oda Y, Shimizu S, Nakamura M. Laparoscopic surgery for congenital biliary dilatation: a single-institution experience. Surg Today. 2018;48:44-50. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 10] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 3. | Shin HJ, Yoon H, Han SJ, Ihn K, Koh H, Kwon JY, Lee MJ. Key imaging features for differentiating cystic biliary atresia from choledochal cyst: prenatal ultrasonography and postnatal ultrasonography and MRI. Ultrasonography. 2021;40:301-311. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 4. | Koukoura O, Kelesidou V, Delianidou M, Athanasiadis A, Dagklis T. Prenatal sonographic diagnosis of biliary tract malformations. J Clin Ultrasound. 2019;47:292-297. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 10] [Cited by in RCA: 14] [Article Influence: 2.3] [Reference Citation Analysis (0)] |
| 5. | Weng R, Hu W, Cai S, Guo X, Luo Q. Prenatal diagnosis and prognosis assessment of congenital choledochal cyst in 21 cases. J Obstet Gynaecol. 2016;36:324-327. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 13] [Cited by in RCA: 13] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 6. | Wu H, Tian J, Li H, Liu H, Liu Y, Lu L, Chen X, Zhang X, Xu W. Accuracy of Magnetic Resonance Imaging in Prenatal Diagnosis of Choledochal Cysts: A Single-Center Retrospective Analysis. Int J Clin Pract. 2022;2022:3268797. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 7. | Ai C, Wu Y, Xie X, Wang Q, Xiang B. Roux-en-Y hepaticojejunostomy or hepaticoduodenostomy for biliary reconstruction after resection of congenital biliary dilatation: a systematic review and meta-analysis. Surg Today. 2023;53:1-11. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (1)] |
| 8. | Liem NT, Agrawal V, Aison DS. Laparoscopic management of choledochal cyst in children: Lessons learnt from low-middle income countries. J Minim Access Surg. 2021;17:279-286. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 9. | Yurttutan N, Karakus SC, Koku N, Demirci M, Ucak R. A giant choledochal cyst in infancy: a case report. Korean J Pediatr. 2016;59:239-241. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 6] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 10. | Guzman JPS, III LLR, Suntay MLR, Bernaldez RG. Comparison between hepaticojejunostomy and hepaticoduodenostomy after excision of choledochal cyst in children: a cohort study. World J Pediatric Surg. 2019;2:e000029. [RCA] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |