Published online Feb 26, 2024. doi: 10.12998/wjcc.v12.i6.1138
Peer-review started: October 7, 2023
First decision: December 8, 2023
Revised: January 6, 2024
Accepted: January 29, 2024
Article in press: January 29, 2024
Published online: February 26, 2024
Processing time: 135 Days and 17.8 Hours
Intestinal obstruction is a common occurrence in clinical practice. However, the occurrence of herpes zoster complicated by intestinal obstruction after abdominal surgery is exceedingly rare. In the diagnostic and treatment process, clinicians consider it crucial to identify the primary causes of its occurrence to ensure effective treatment and avoiding misdiagnosis.
Herein, we present the case of a 40-year-old female patient with intestinal ob
Pseudo-intestinal obstruction secondary to herpes zoster infection is difficult to distinguish from mechanical intestinal obstruction owing to various causes. In cases of inexplicable intestinal obstructions, considering the possibility of a viral infection is essential to minimize misdiagnosis and missed diagnoses.
Core Tip: Herpes zoster may induce a rare pseudo-obstruction of the small intestine in addition to pseudo-obstruction of the colon. We highlight an extremely rare case of a patient with small bowel pseudo-obstruction caused by herpes zoster after abdominal surgery. More unusual, this patient presented with intestinal symptoms after the onset of rash. In cases of inexplicable intestinal obstructions, considering the possibility of a viral infection is essential to minimize misdiagnosis and missed diagnosis.
- Citation: Dong ZY, Shi RX, Song XB, Du MY, Wang JJ. Postoperative abdominal herpes zoster complicated by intestinal obstruction: A case report. World J Clin Cases 2024; 12(6): 1138-1143
- URL: https://www.wjgnet.com/2307-8960/full/v12/i6/1138.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i6.1138
The occurrence of herpes zoster in the abdomen causing gastrointestinal symptoms is extremely rare. Herpes zoster complicated by pseudo-intestinal obstruction, primarily manifests as acute colonic obstruction (known as the Ogilvie syndrome). In addition to pseudo-obstruction of the colon, herpes zoster can induce a rare pseudo-obstruction of the small intestine[1-3]. Previous reports have suggested that herpes zoster induces acute pseudocolonic obstruction in patients who had undergone abdominal surgery, presenting bowel obstruction as the initial manifestation[4]. In most cases, pseudo-intestinal obstruction develops days to weeks before a rash appears[1]. In this case report, we highlight an extremely rare case of a patient with small bowel pseudo-obstruction, induced by herpes zoster after abdominal surgery. Remarkably, this patient presented with intestinal symptoms later than the onset of rash.
Skin rash on the right lower abdomen for 3 d and, abdominal pain with bloating for 1 d.
A 40-year-old female patient underwent a laparoscopic appendectomy at Baotou Central Hospital in April 2022. By day 2 after abdominal surgery, the patient transitioned to her regular diet and was successfully discharged from the hospital. On day 4, the patient developed clusters of erythematous rashes in the right lower abdomen, causing itching and pain at the site of the rash, along with intermittent radiating pain in the bilateral iliolumbar region. On the day 7, the patient experienced abdominal pain localized to the center of the abdomen, accompanied by nausea, vomiting, abdominal distension, and cessation of exhaust, with passage of only a small amount of stools. The abdominal pain later increased paroxysmally and persisted without relief, leading the patient to seek further treatment at Baotou Central Hospital.
The patient had been vaccinated against varicella in early childhood and experienced a varicella infection for the first time in 2017. The patient underwent laparoscopic appendectomy at Baotou Central Hospital in April 2022 and was in close contact with a patient who developed herpes zoster after abdominal surgery.
The patient denied any family history of malignant tumors.
After admission to the hospital, the patient's temperature was 37.1 ºC. Physical examination revealed clusters of red rashes in the right lower abdomen (Figure 1), tenderness in the middle and lower abdomen, and active bowel sounds.
Laboratory examination revealed an elevated white blood cell count (11.28 × 109 cells /L), neutrophil ratio (86.40%), and erythrocyte sedimentation rate (50 mm/h).
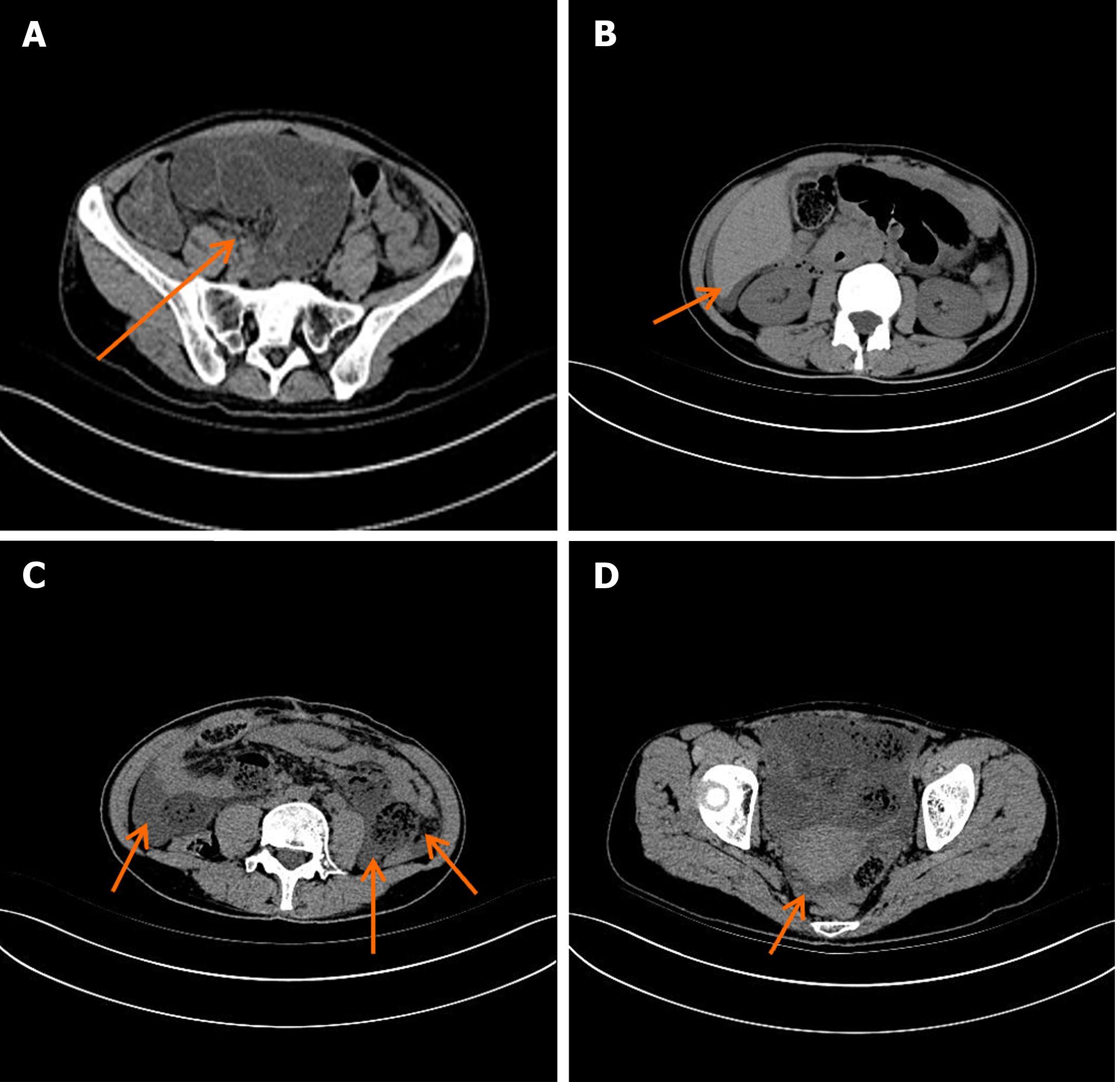
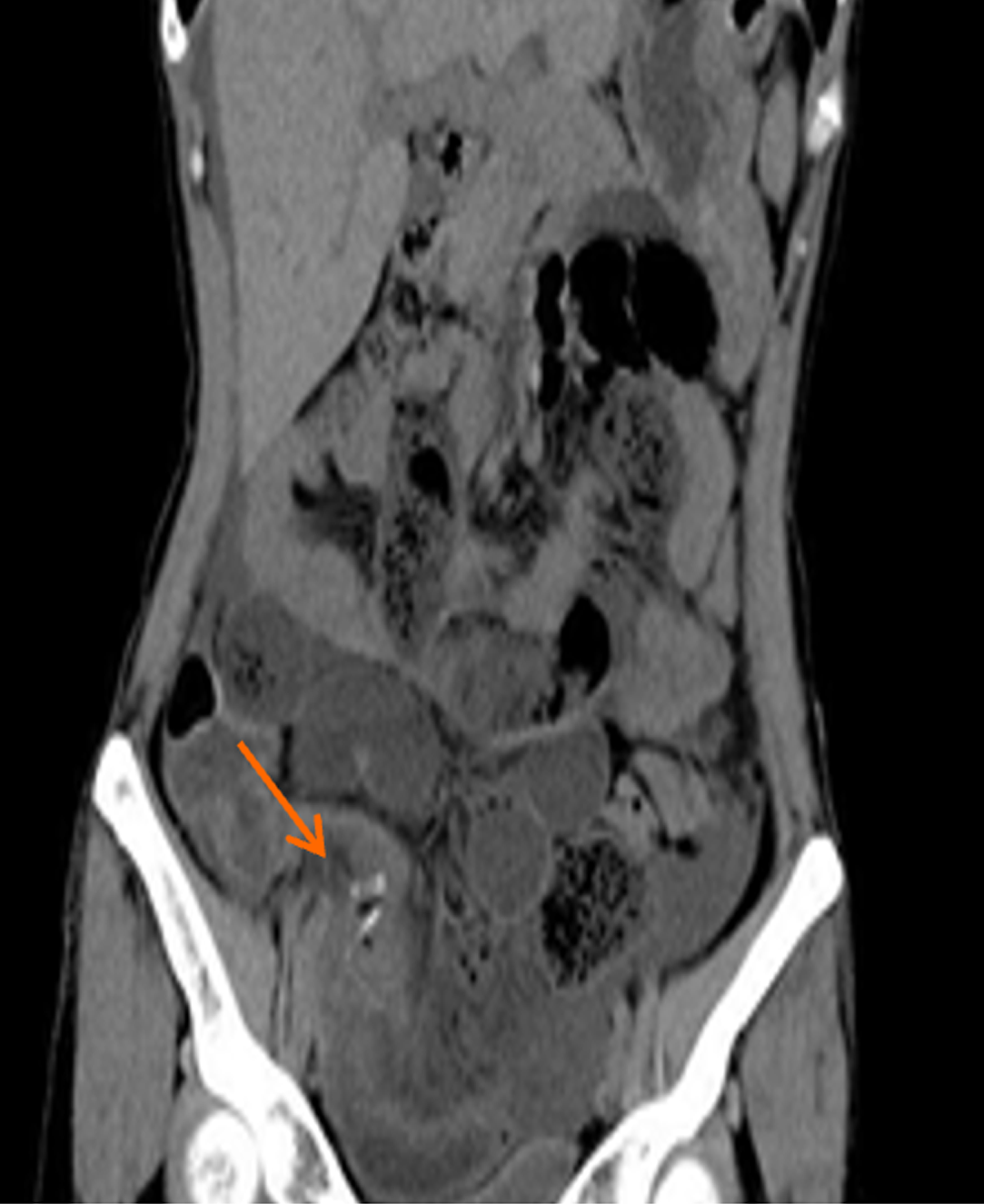
Abdominal ultrasonography revealed the presence of fluid inside the abdominal cavity. An upright abdominal plain radiograph indicated gas accumulation and scattered fluid levels in the abdominal intestine, suggesting intestinal obstruction (Figure 2). Whole-abdominal computed tomography confirmed considerable dilation and fluid accumulation in the abdominal and pelvic bowel, supporting the diagnosis (Figure 3A). Furthermore, it revealed fluid accumulation in the abdominal and pelvic cavities (Figures 3B-D). Additionally, at the coronal level, we could observe the position of the hem-lock clamp used during the patient's previous laparoscopic appendectomy (Figure 4).
Herpes zoster complicated by small bowel pseudo-obstruction was diagnosed.
The patient was treated with conservative management, including fasting on water, gastrointestinal decompression, enema and defecation, and fluid replenishment, along with antiviral therapy.
Over the next 5 d, the patient's abdominal pain and distension gradually subsided, with a concurrent reduction in the extent of the herpes zoster. At the follow-up visit after 15 d, the abdominal herpes zoster had completely disappeared and the patient recovered successfully. The patient remained symptom-free throughout the 1-year follow-up period.
Primary varicella zoster virus (VZV) infection results in varicella, which usually occurs in early childhood and causes a diffuse rash and viremia. The virus then establishes lifelong latency in the neurons of the dorsal-root, cranial-nerve, and enteric nervous system (ENS) ganglia[5]. Reactivation of VZV reactivates from latency is observed in approximately 30% of individuals, leading to a secondary cutaneous herpes zoster. Predisposing factors for VZV reactivation from latency include old age, stress, malnutrition, menstruation, and immunosuppression associated with malignancy, post-transplantation, and chemotherapy[6]. Herpes zoster is characterized by clustered blisters distributed along the peripheral nerves on one side of the body, accompanied by significant neuralgia[7]. Infection with herpes zoster virus causes a series of complications, including acute pain syndrome and postherpetic neuralgia. Peripheral motor neuropathy is an uncommon complication (2.5%–9.4%), affecting approximately 15% of the general population[8]. They can be somatic or visceral[9]. Depending on the level of the lesion, peripheral neuropathy may manifest as segmental motor paralysis of the upper and lower limb muscles, trunk, bladder, intestine, or diaphragm, whereas visceral neuropathy may involve the bladder and cause cystitis and/or urinary retention[1].
Cases of herpes zoster causing gastrointestinal symptoms in the abdomen are extremely rare, with colonic pseudo-obstruction considered the most common gastrointestinal complication[1]. In Ogilvie syndrome, the typical radiographic findings include marked dilatation of the cecum, ascending colon, and transverse colon[10]. Ogilvie syndrome, a special type of visceral herpes zoster, is a motor dysfunction caused by intestinal muscle neuropathy and is believed to occur when, owing to low immunity, VZV invades the visceral nerve fibers of the sympathetic and parasympathetic nerves, resulting in edema and inflammation of the motor nerve fibers[11]. Although it can occur at any age, it generally affects adults over 60 years of age. Common ganglion distribution is mainly concentrated at T10–T12 and L1-L4[12]. Small bowel pseudo-obstruction caused by herpes zoster is thought to share a similar mechanism with colonic pseudo-obstruction[2]. The herpes zoster virus stimulates sympathetic nerves, inhibits small intestinal peristalsis, and damages the myenteric plexus and muscularis propria[1,3].
VZV reaches the ENS through two potential mechanisms: transportation by peripheral T-lymphocytes and retrograde axonal transport from dorsal-root ganglion neurons infected through their epidermal projections[13]. Regardless of the triggering factors, VZV reactivation is likely to have the same effect on the ENS neurons[11]. Various theories on the pathogenesis of zoster-related gut obstruction are: (1) Parietal and visceral peritoneal inflammation; (2) extrinsic autonomic nervous system viral involvement; (3) direct VZV injury of both the enteric submucosal and myenteric plexus, as well as the muscularis propria; (4) possible hemorrhagic infarction of the abdominal sympathetic ganglia; (5) viral interruption of afferent C-fibers that cause intestinal hypomotility and subsequent pseudo-obstruction; and (6) viral injury of the thoracolumbar or sacral lateral columns resulting in disruption of parasympathetic nerves and subsequent intestinal hypomotility[1,2,11,12].
The best initial treatment for Ogilvie syndrome caused by herpes zoster is conservative management, which is successful in approximately 75% of patients. In cases where conservative treatment fails or the caecum is considerably dilated (> 12 cm), alternative treatments, including medical therapy, endoscopic decompression, or surgery, are considered[14]. For small bowel pseudo-obstruction, given the sympathetic innervation of the small bowel occurring through the T9 and T10 branches, epidural catheter insertion from the T9–T10 branches and local anesthetics administration can effectively block the sympathetic nerves, thereby shortening the treatment course and preventing severe complications requiring surgical intervention (i.e. intestinal necrosis and perforation)[2,15].
This reported case of pseudo small bowel obstruction due to herpes zoster after laparoscopic appendectomy is exceptionally rare. In particular, the onset of intestinal symptoms occurring later than the appearance of rash is an extremely rare pattern. However, current reports on pseudo-intestinal obstruction secondary to herpes zoster infection, both nationally and internationally, show that cutaneous herpes zoster occurs within a few days or weeks after intestinal involvement[6]. In this case, we considered that the patient had just undergone abdominal surgery and had close contact with herpes zoster virus-infected patients after the surgery, which had led to the reactivation of the VZV in the latent period. In our patient, herpes zoster was detected in the right lower abdomen. The virus is thought to invade the visceral nerve fibers and caused gastrointestinal dysfunction, resulting in intestinal obstruction due to the loss of intestinal motility. In addition, the patient in this case was a middle-aged woman, younger than the typical patient with pseudo-obstruction, who had an atypical location of the small bowel; therefore, several underlying causes for the intestinal obstruction is possible. Postoperative small bowel obstruction is a common complication of appendectomy. Women, in particular, have a higher risk of small bowel obstruction after appendectomy[16]. Additionally, occult etiologies causing small bowel obstruction, such as subclinical pelvic inflammatory pelvic disease, endometriosis, or inflammation of the adnexa, may also be misdiagnosed as adhesive small bowel obstruction.
In conclusion, herpes zoster complicated by pseudointestinal obstruction after abdominal surgery is rare. The clinical presentation of pseudo-intestinal obstruction secondary to herpes zoster infection is difficult to distinguish from that of mechanical intestinal obstruction due to other causes. For some inexplicable intestinal obstructions, considering the possibility of a viral infection is essential to minimize misdiagnosis and missed diagnoses.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Gastroenterology and hepatology
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C, C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Bortolotti M, Italy; Valek V, Czech Republic S-Editor: Zhang H L-Editor: Filipodia P-Editor: Cai YX
| 1. | Anaya-Prado R, Pérez-Navarro JV, Corona-Nakamura A, Anaya-Fernández MM, Anaya-Fernández R, Izaguirre-Pérez ME. Intestinal pseudo-obstruction caused by herpes zoster: Case report and pathophysiology. World J Clin Cases. 2018;6:132-138. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 14] [Cited by in RCA: 8] [Article Influence: 1.1] [Reference Citation Analysis (1)] |
| 2. | Lin YC, Cui XG, Wu LZ, Zhou DQ, Zhou Q. Resolution of herpes zoster-induced small bowel pseudo-obstruction by epidural nerve block: A case report. World J Clin Cases. 2022;10:9873-9878. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in CrossRef: 4] [Reference Citation Analysis (0)] |
| 3. | Pui JC, Furth EE, Minda J, Montone KT. Demonstration of varicella zoster virus infection in the muscularis propria and myenteric plexi of the colon in an HIV-positive patient with herpes zoster and small bowel pseudo-obstruction (Ogilvie's syndrome). Am J Gastroenterol. 2001;96:1627-1630. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 49] [Cited by in RCA: 48] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Ma C, Lv XP, Xia H and Song T. A case of acute colonic obstruction complicated by herpes zoster after abdominal surgery. Zhonghua Putong Waike Xue Wenxian (Electron Ed). 2015;9:232-233. [DOI] [Full Text] |
| 5. | Alpay K, Yandt M. Herpes zoster and Ogilvie's syndrome. Dermatology. 1994;189:312. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 6. | Edelman DA, Antaki F, Basson MD, Salwen WA, Gruber SA, Losanoff JE. Ogilvie syndrome and herpes zoster: case report and review of the literature. J Emerg Med. 2010;39:696-700. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 41] [Cited by in RCA: 35] [Article Influence: 2.3] [Reference Citation Analysis (1)] |
| 7. | Schmader K. Herpes Zoster. Ann Intern Med. 2018;169:ITC19-ITC31. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 38] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 8. | Thomas JE, Howard FM Jr. Segmental zoster paresis--a disease profile. Neurology. 1972;22:459-466. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 187] [Cited by in RCA: 156] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 9. | Maeda K, Furukawa K, Sanada M, Kawai H, Yasuda H. Constipation and segmental abdominal paresis followed by herpes zoster. Intern Med. 2007;46:1487-1488. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 10. | Haran C, Kyngdon RJ. Herpes zoster: a rare cause of Ogilvie syndrome. ANZ J Surg. 2021;91:E637-E639. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 11. | Carrascosa MF, Salcines-Caviedes JR, Román JG, Cano-Hoz M, Fernández-Ayala M, Casuso-Sáenz E, Abascal-Carrera I, Campo-Ruiz A, Martín MC, Díaz-Pérez A, González-Gutiérrez P, Aguado JM. Varicella-zoster virus (VZV) infection as a possible cause of Ogilvie's syndrome in an immunocompromised host. J Clin Microbiol. 2014;52:2718-2721. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 12] [Cited by in RCA: 13] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 12. | Masood I, Majid Z, Rind W, Zia A, Riaz H, Raza S. Herpes Zoster-Induced Ogilvie's Syndrome. Case Rep Surg. 2015;2015:563659. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 6] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Chen JJ, Gershon AA, Li Z, Cowles RA, Gershon MD. Varicella zoster virus (VZV) infects and establishes latency in enteric neurons. J Neurovirol. 2011;17:578-589. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 80] [Cited by in RCA: 79] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 14. | Ben Ameur H, Boujelbene S, Beyrouti MI. [Treatment of acute colonic pseudo-obstruction (Ogilvie's Syndrome). Systematic review]. Tunis Med. 2013;91:565-572. [PubMed] |
| 15. | Ponec RJ, Saunders MD, Kimmey MB. Neostigmine for the treatment of acute colonic pseudo-obstruction. N Engl J Med. 1999;341:137-141. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 422] [Cited by in RCA: 331] [Article Influence: 12.7] [Reference Citation Analysis (0)] |
| 16. | Tseng CJ, Sun DP, Lee IC, Weng SF, Chou CL. Factors Associated With Small Bowel Obstruction Following Appendectomy: A Population-Based Study. Medicine (Baltimore). 2016;95:e3541. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 9] [Article Influence: 1.0] [Reference Citation Analysis (0)] |