Published online Feb 16, 2024. doi: 10.12998/wjcc.v12.i5.903
Peer-review started: October 26, 2023
First decision: November 8, 2023
Revised: December 5, 2023
Accepted: January 19, 2024
Article in press: January 19, 2024
Published online: February 16, 2024
Processing time: 97 Days and 3.7 Hours
Vestibular dysfunction (VH) is a common concomitant symptom of late peri
To explore the effect of health education based on the IMB model on the degree of vertigo, disability, anxiety and depression in patients with unilateral vestibular hypofunction.
The clinical data of 80 patients with unilateral vestibular hypofunction from January 2019 to December 2021 were selected as the retrospective research objects, and they were divided into the control group and the observation group with 40 cases in each group according to different nursing methods. Among them, the control group was given routine nursing health education and guidance, and the observation group was given health education and guidance based on the IMB model. The changes in self-efficacy, anxiety and depression, and quality of life of patients with unilateral VH were compared between the two groups.
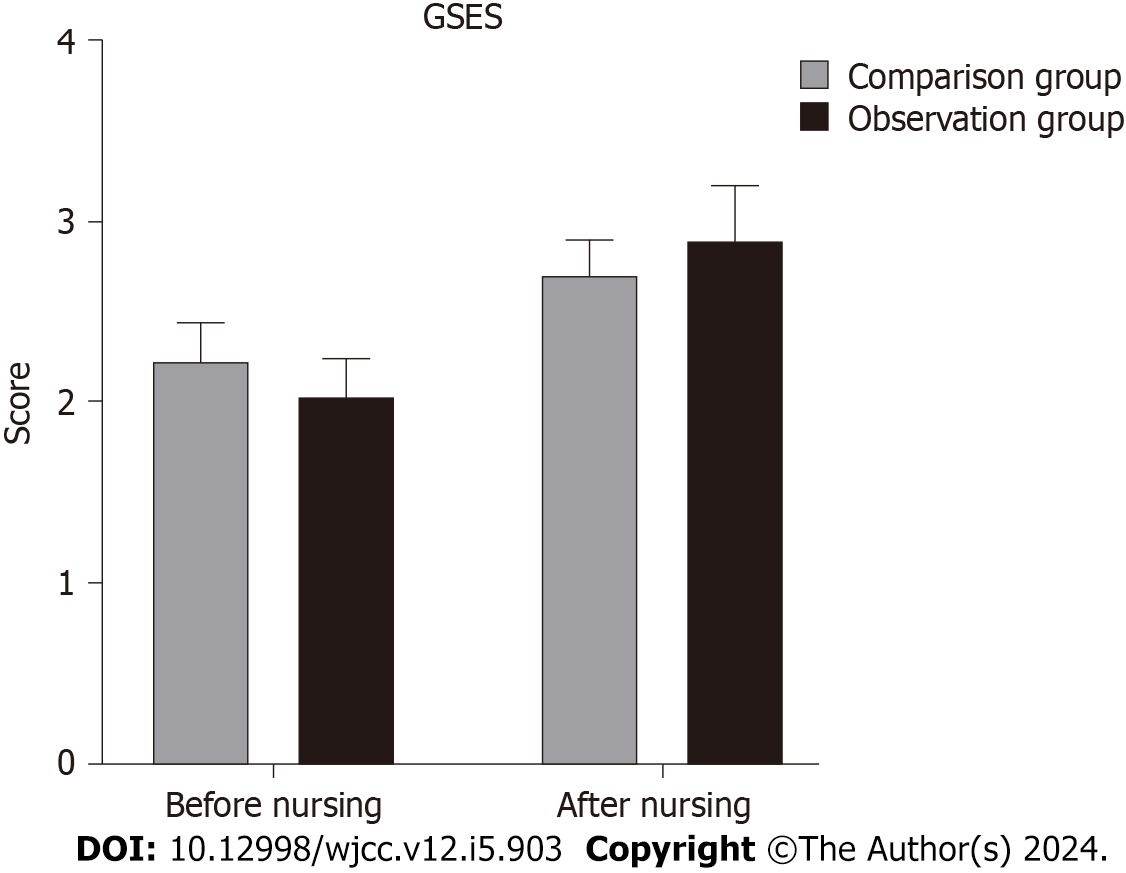
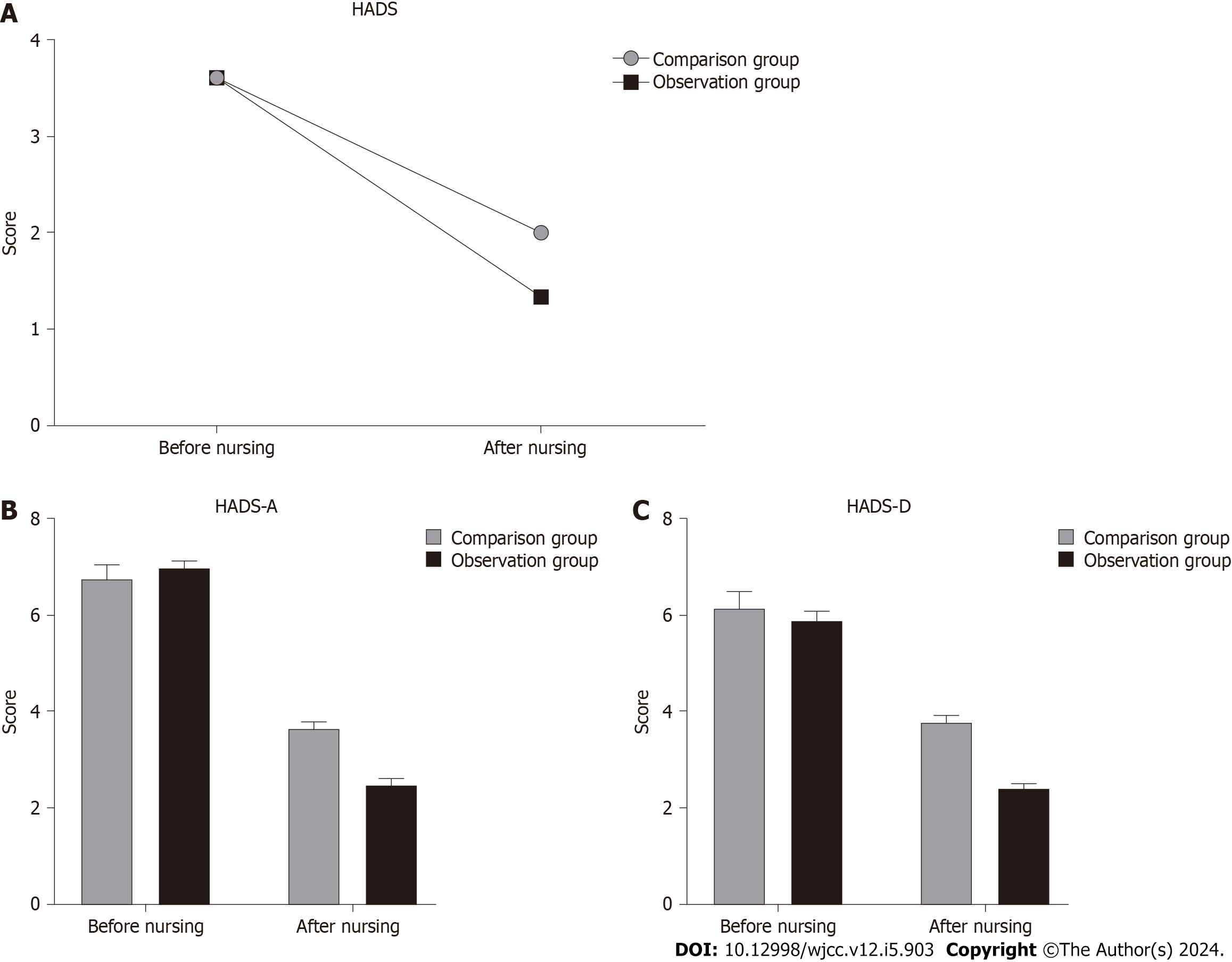
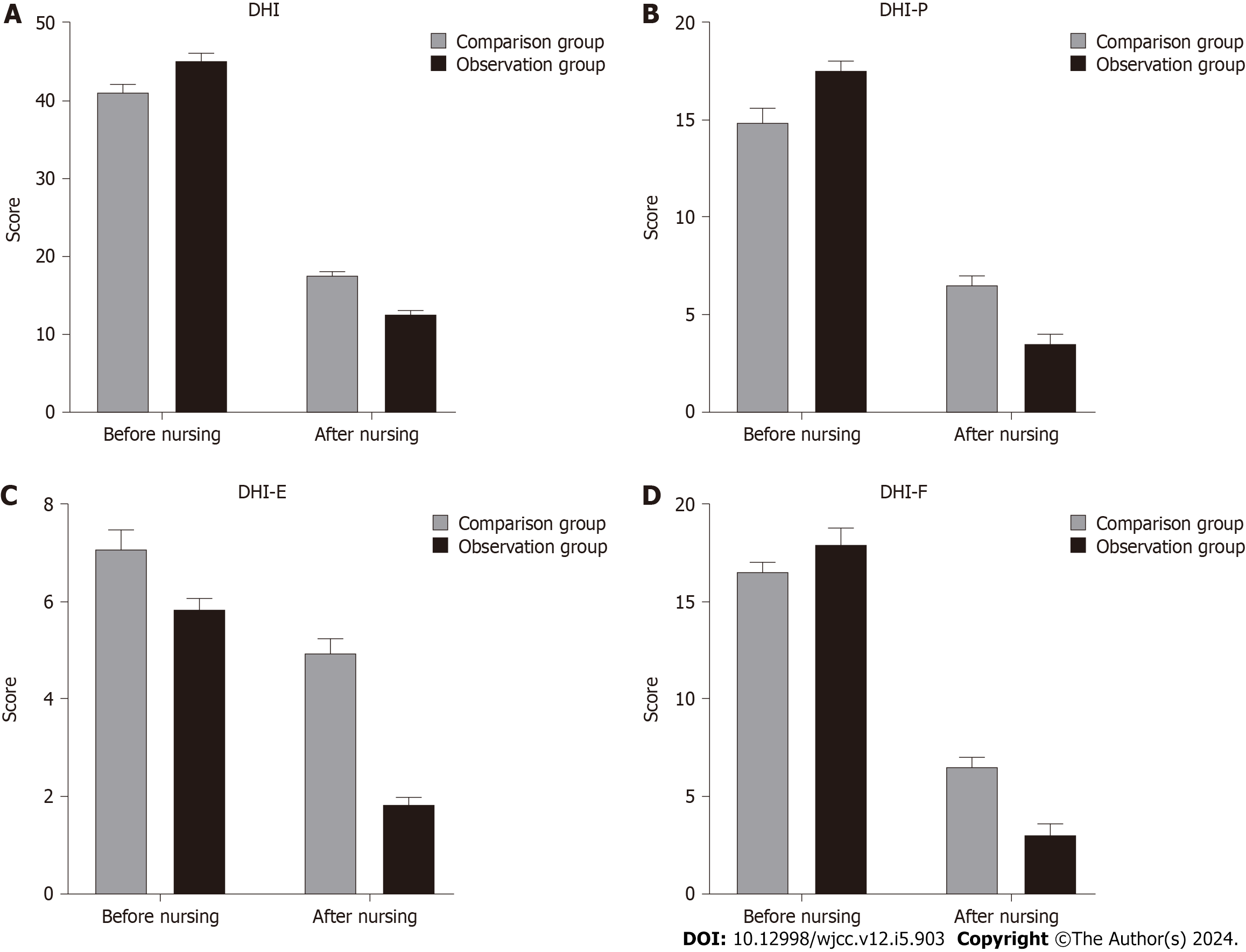
There was no significant difference in General Self-Efficacy Scale (GSES) scale scores between the two groups of patients before nursing (P > 0.05), which was comparable; after nursing, the GSES scale scores of the two groups were higher than those before nursing. The nursing group was higher than the control group, and the difference was statistically significant (P < 0.05). There was no significant difference in the scores of Hospital Anxiety and Depression Scale (HADS) and anxiety and depression subscales between the two groups before nursing (P > 0.05). After nursing, the HADS score, anxiety, and depression subscale scores of the two groups of patients were lower than those before nursing, and the nursing group was lower than the control group, and the difference was statistically significant (P < 0.05). After nursing, the Dizziness Handicap Inventory (DHI) scale and DHI-P, DHI-E and DHI-F scores in the two groups were decreased, and the scores in the nursing group were lower than those in the control group, and the difference was statistically significant (P < 0.05).
Health education based on the IMB model can effectively improve patients' quality of life, increase self-efficacy of patients with unilateral vestibular hypofunction, enhance patients' confidence, enable patients to resume normal work and life as soon as possible, reduce patients' anxiety and depression, and effectively improve patients' psychological status.
Core Tip: Vestibular dysfunction (VH) is a common concomitant symptom in the late stage of various external vestibular diseases, and the etiology is unknown in about 50% of cases. In this paper, 80 patients with unilateral VH were selected as retrospective research objects. We found that health education based on information-motivation-behavioral skills model can effectively improve the quality of life of patients, improve the self-efficacy of patients with unilateral VH, enhance their self-confidence, enable them to return to normal work and life as soon as possible, and reduce their anxiety and depression. Effectively improve the psychological state of patients.
- Citation: Shi Q, Wu RJ, Liu J. Effect of health education based on information-motivation-behavioral skills model on patients with unilateral vestibular dysfunction. World J Clin Cases 2024; 12(5): 903-912
- URL: https://www.wjgnet.com/2307-8960/full/v12/i5/903.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i5.903
Vestibular dysfunction (VH) is a common concomitant symptom in the late stages of a variety of peripheral vestibular lesions, and although the cause of VH may be traumatic, toxic, infectious, genetic, or neurodegenerative, the etiology is unknown in approximately 50% of cases[1,2]. Postural instability, blurred vision during head movements, dizziness, and imbalance can occur in the decompensated phase after vestibular function injury[3]. In recent years, the incidence of vestibular vertigo has been increasing with the increase of various adverse factors and the aging of the population[4]. Vertigo and dizziness due to vestibular hypofunction can also cause a series of psychological problems, such as depression and anxiety, if not taken care of in a timely manner. Unilateral VH (UVH) is observed and measured by video nystagmography, and vestibular function is assessed using the slow-phase velocity of the vestibular oculomotor reflex with a hemiplegic value greater than or equal to 25% on one side[5]. The information-motivation-behavioral skills (IMB) model can be used both as a model to predict health behaviors and as a framework of care for patients in terms of information, motivation, and behavioral skills to induce behavioral change[6]. Information is an important component in the IMB model, but it is not sufficient by itself to change behavior; information and motivation lead to changes in individual attitudes, but individuals need behavioral skills to put their behaviors into practice[7]. The IMB model posits that information and motivation activate behavioral skills that lead to behavior change and maintenance of change; information and motivation may also have a direct impact on health behaviors, especially when accomplishing specific Behavior does not require complex or new behavioral skills when the IMB model has the advantage of incorporating self-efficacy theory, drawing on rational behavior theory's understanding of motivation, and integrating various factors that influence behavior, which has higher feasibility[8].
Currently, no studies have been seen using the IMB model of health education for the care of patients with VH. Although research on vestibular rehabilitation started earlier in China, there is still a gap between the research on vestibular rehabilitation and foreign countries, and the development of vestibular rehabilitation exercises and the implementation of individualized vestibular rehabilitation are not ideal[9]. Nowadays, with economic development people's requirements for quality of life are increasing, and the benefits that patients can obtain from vestibular rehabilitation should not be ignored. Our study attempts to use the IMB model of health education as a guide, aiming to improve patients' self-efficacy, reduce symptoms, improve their quality of life, return them to normal life sooner and use their professional knowledge to avoid health misconceptions in their daily life.
The clinical data of 80 patients with unilateral VH from January 2019 to December 2021 were selected as the subjects of a retrospective study and divided into a comparison group and an observation group of 40 cases each according to the mode of care. UVH diagnosis[6]: Vestibular oculomotor reflexes were observed and measured by video nystagmography, and vestibular function was assessed using the slow-phase velocity of the vestibular oculomotor reflex with a value of light paralysis of the semicircular canal on one side The value of hemiplegia on one side was greater than or equal to 25%. The data collected in our study were used only for clinical research and data analysis, not for other purposes, and no other personnel had the right to use the study data without the consent of the study subjects, which helped the patients to improve their dizziness symptoms and did not cause any physical or mental harm to them.
Inclusion criteria: (1) Vestibular function examination (hot and cold test) with results reported as unilateral VH, age ≥ 18 years, with elementary school or above education; (2) patients with self-care ability, able to understand and cooperate with our study, detailed and complete clinical information of patients and their families; and (3) patients in non-acute vertigo period, able to cooperate with hot and cold test examination.
Exclusion criteria: (1) Those with cognitive impairment or mental illness, unable to communicate normally, with otolithic balance test (+); (2) those with other types of vertigo, such as acute vertigo, central vertigo, traumatic vertigo, with serious cardiovascular system diseases, respiratory system diseases or major diseases in other parts of the body and serious systemic diseases; and (3) those with a history of malignant tumors, unable to rehabilitation training, such as cervical spondylosis, bone and joint disease, visual impairment, hemiplegia, pregnancy, etc., and the use of vestibular inhibitory drugs such as flunarizine hydrochloride, vertigo stop, diazepam, etc. within 48 h.
Patients fill out questionnaires and scales in detail at the first visit. Nurses introduce patients to knowledge related to vestibular function, high-risk factors, medication guidance, etc., and carefully answer patients' questions about disease treatment and rehabilitation. Psychological care: anxiety and depression can interact with vertigo and dizziness symptoms, so you should divert your attention appropriately and keep a relaxed state of mind. Treatment in case of vertigo attack: When vertigo occurs, lie down close to the bed or sit on the ground to avoid falling. Inform patients that vestibular rehabilitation exercises can help relieve the symptoms of dizziness and vertigo, and instruct them on general vestibular rehabilitation exercises: (1) Patients take a lying or sitting position to practice repeatedly according to the situation (the speed is first slow and then fast: Look up and down with both eyes; look left and right with both eyes; stare at fingers with both eyes and move from 1 meter to 0.3 meter in front of you; tilt your head forward and then backward; turn your head left and right (the latter two practice with eyes open first and then with eyes closed); (2) patients take a sitting position: shrugging shoulders around; upper body leaning forward and picking up objects from the floor; (3) patients were in the standing position for the first two steps, and then practiced separately: Sitting to standing with eyes open and closed; passing the ball from left to right hand; turning and standing from the seat; and (4) activities: Patients practiced walking across the room with eyes open and closed, respectively; walking back and forth up ramps and steps; any movement that required bending and stretching. Repeat each movement 20 times, 2-3 times a day. The method and precautions. At the biweekly review, the questions raised by the patients were answered and the patients were instructed to review on time.
Information care: Patients were given the "Knowledge manual related to vestibular hypofunction" to explain the knowledge about vestibular hypofunction, high-risk factors, clinical manifestations, etc., and to inform patients of the importance of vestibular rehabilitation exercises for symptom relief, etc., so as to eliminate patients' potential anxiety due to lack of disease knowledge; when the care was repeated, the patients' mastery of the previous care was first assessed, and the weak points were supplemented. Commonly used drugs for vestibular hypofunction mainly include drugs to improve microcirculation, symptomatic supportive therapy, glucocorticoids, etc.; inform patients of the name, dosage, usage, and adverse effects of commonly used drugs. Inform patients of the risks of the disease to their own safety, make a good assessment of the safety of their home environment, ensure adequate rest and sleep, and avoid overexertion. Normal daily activities can be performed, avoid strenuous exercise, and to reduce the risk of falls, elderly patients need to be accompanied by family members when going out. Patients are invited to add WeChat or contact phone numbers to answer questions related to rehabilitation treatment, send weekly information about diseases related to vestibular hypofunction, rehabilitation exercise videos, etc., and instruct patients to review on time.
Behavioral care: Provide patients with a good environment for medical care, receive only one patient at a time, fully protect patients' privacy, actively communicate with patients, understand the impact of the disease on their work and life, listen to patients' concerns during the disease treatment process, encourage patients to express their inner thoughts and health needs, and answer patients' questions one by one. We also use this as a basis to assess the patient's perception of the disease so that we can give appropriate guidance to the patient's specific situation in educational nursing care and provide strong support to the patient. Patients were introduced to cases of successful treatment of dizziness and vertigo to enhance their confidence, encouraged to state the reasons that led to their lack of confidence in treatment and affected their health behaviors, enhanced their determination to actively cooperate with treatment through comfort, encouragement and praise, and set goals for rehabilitation exercises together with patients to motivate them to join rehabilitation exercises on their own initiative. Ask patients about the difficulties they encounter in the rehabilitation process and answer them during the biweekly review. Understand the support status of the patient's family and friends; provide guidance to the patient's family along with health guidance, instruct the family on ways to help the patient improve his anxiety and depression, and encourage and supervise the patient's daily rehabilitation exercises at home.
Vestibular rehabilitation exercises instruction: Patients raise their arms, put their fingers in front of their eyes and keep them still, look at their fingers levelly and turn their heads from side to side. The patient raises the arm, places the finger in front of the eyes and keeps it still, looks at the finger with the eyes level, then closes the eyes while trying to fix the eyes on the position where the finger rests, then turns the head from side to side, then opens the eyes to see if the eyes are looking at the finger, starting with the head in the center position. The patient keeps gazing at the fixed target in front while moving the head up and down and repeating the previous movements. Each movement is practiced for 1-2 min, 2-3 times a day. Patients stand with eyes open, gradually reduce the distance between the feet, and practice standing with eyes closed after being able to maintain stability. Patients open their eyes and stand on their toes next to their heels and walk with their feet back and forth, and practice walking with eyes closed after being able to maintain balance, and instruct patients to intersperse head movements (e.g., head twisting, turning, etc.) while walking. Each posture for 15-30 s, 2-3 times a day. The patient's upper body is upright and sits on the edge of the bed with legs naturally hanging down; quickly lie on the bed to the right side, turn the face 45° to the opposite side in front and above, keep the position of legs unchanged, sit up for 30 s after waiting for the vertigo to disappear, if the patient does not feel vertigo, sit up for 30 s after resting, quickly lie on the bed to the left side, turn the face 45° to the opposite side in front and above, sit up after 30 s, alternate sides. Repeat each movement 10-20 times, 2-3 times a day.
The Self-Efficacy Scale (SES) consists of 10 items, each with 4 options and a score range of 1 to 4. The total score of the scale is the sum of the items divided by 10, and the higher the score, the higher the patient's self-efficacy. The consistency coefficient was 0.87, the retest reliability was 0.83, and the half reliability was 0.82, which had good reliability and validity. The Dizziness Handicap Inventory (DHI) is a 25-item, 3-dimensional scale that assesses the functional, emotional and physical impairment and quality of life of patients with vertigo, with 3 answers for each item: "yes (4 points), sometimes (2 points), no (0 points)"; the total score ranges from 0 to 100. The higher the score, the higher the impact of vertigo on the patient. The Hospital Anxiety and Depression Scale (HADS) is used to screen patients attending general medical clinics for anxiety and depression. It has the advantage of being simple, quick and easy to use, and consists of two subscales that rate depression and anxiety, each with 7 entries, 4 answers per entry, and a score of 0 to 3. The scores of the two subscales of anxiety and depression are divided as follows: 0-7 for asymptomatic; 8-10 for suspicious symptoms; and 11-21 for definitely present symptoms.
All data from our study were checked using Excel double entry, and SPSS 23.0 was used for statistical analysis, setting the test level α = 0.05 and considering P < 0.05 as a statistically significant difference. Statistical descriptions of measurement data obeyed normal distribution were described by mean ± SD, and those not obeying normal distribution were described by median (interquartile spacing), and count data were described by frequency and composition ratio. General patient data were analyzed: Categorical data were analyzed by chi-square test, continuity-corrected chi-square test, and Fisher's exact probability method; measurement data were analyzed by t-test. Obedience to normal distribution, paired samples t-test was used for within-group comparisons and two independent samples t-test for between-group comparisons; disobedience to normal distribution, nonparametric test-Wilcoxon signed-rank test was used for within-group comparisons and rank sum test was used for between-group comparisons for analysis.
The mean age, gender, and education of the patients in the observation group were not significantly different from those in the weight comparison group, and none of the comparative differences were statistically significant (P > 0.05) (Table 1).
| Group | Average age (yr) | Gender (male/female) | Body weight (kg) | Education level | ||
| Junior high school | High school | University and above | ||||
| Comparison group (40) | 60.90 ± 1.71 | 24/26 | 66.35 ± 2.10 | 12 | 12 | 16 |
| Observation group (40) | 61.10 ± 1.62 | 23/27 | 64.10 ± 1.10 | 13 | 10 | 17 |
| t value | 0.377 | 0.731 | 2.107 | 0.252 | ||
| P value | 0.051 | 0.067 | 0.079 | 0.882 | ||
The difference between the General SES (GSES) scores of the two groups of patients before care was not statistically significant (P > 0.05) and was comparable; the GSES scale scores of the two groups of patients after care were higher than those before care, and the difference between the GSES scale scores of the two groups of patients after care was higher than that of the control group (P < 0.05) (Figure 1).
There was no significant difference in the scores of HADS and anxiety and depression subscales between the two groups before nursing (P > 0.05). After nursing, the HADS score, anxiety (HADS-A), and depression (HADS-D) subscale scores of the two groups of patients were lower than those before nursing, and the nursing group was lower than the control group, and the difference was statistically significant (P < 0.05) (Figure 2).
Before nursing, there was no significant difference in the total DHI scale score and DHI-P, DHI-E and DHI-F dimension scores between the two groups (P > 0.05). After nursing, the DHI scale and DHI-P, DHI-E and DHI-F scores in the two groups were all decreased, and the scores in the nursing group were lower than those in the control group, and the difference was statistically significant (P < 0.05) (Figure 3).
Initially, care for vertigo in China was mainly directed at the etiology of the disease, but different etiologies often leave similar dysfunctions, which continue to have an impact on the quality of life of patients[10]. In recent years, research on the care of VH has gradually increased, and studies by scholars have confirmed that vestibular rehabilitation exercises can reduce clinical symptoms such as vertigo and improve the quality of life of patients[11]. Some scholars used the medical-nursing cooperation model to care for patients with VH, and the results showed that this model can effectively promote the functional recovery of patients[12]. The effect of health guidance based on the WeChat platform on the rehabilitation management of patients with vestibular function was investigated[13]. The rehabilitation management based on the WeChat platform enhanced the supervision of patients' rehabilitation training and promoted the improvement of patients' vertigo symptoms[14].
In our study, the GSES scale scores of patients in both groups were higher after care than before care, and the GSES scale scores of patients in both groups were higher in the care group than in the control group after care, with statistically significant differences. It indicates that both intervention methods have a certain effect on improving patients' self-efficacy. The reasons for this were analyzed as, on the one hand, the patients did not know much about vestibular hypofunction before the consultation and knew little about the management of vertigo and dizziness episodes, and the repeated vertigo and dizziness episodes affected the patients' work and life[15]. After the consultation patients received more information about the disease, learned the appropriate skills to relieve vertigo and dizziness, and improved their self-confidence to cope with the disease[16]. On the other hand, IMB mode health education was provided to patients through disease knowledge, communication through WeChat, video explanation of rehabilitation exercises, knowledge booklet distribution, case sharing, and motivational interventions[7]. It enables patients to receive more professional and comprehensive information and participate in the rehabilitation training of the disease, so that they have a more positive attitude and more confidence to cope with the current disease condition[17]. No domestic studies on the intervention of IMB model health education for patients with vestibular hypofunction have been retrieved.
The HADS-A and HADS-D subscale scores of patients in both groups after our study care were lower than before care, and both care groups were lower than the control group, and the differences were statistically significant. The classical treatment of VH relies on vestibular rehabilitation and symptomatic medication, of which vestibular rehabilitation is an exercise-based dizziness treatment that is mainly used to reduce vestibular symptoms[18]. Studies by scholars have shown that nurse-led vestibular rehabilitation exercises improve patients' vestibular discomfort symptoms earlier and enhance their balance confidence[19]. The patients' DHI scale scores decreased significantly, similar to the results of our study[20]. Conventional health education is mostly delivered verbally; in our study, IMB model-based health education was used to train patients on rehabilitation exercises and explain the exercise steps to them in detail[21]. Not only is the appropriate exercise method selected according to the individual patient, but it is also adjusted according to the patient's rehabilitation progress at the time of review[16]. Patients were also intervened through personal motivation and social motivation aspects to enhance their self-efficacy, strengthened their understanding of the importance of vestibular rehabilitation, and given appropriate guidance by understanding the reasons that prevented them from performing rehabilitation training[22]. The patients and their families were made to actively participate in vertigo treatment and rehabilitation exercises, and the patients had more motivation and confidence to adhere to the exercises[23]. With the relief of vertigo and dizziness symptoms and functional recovery, the patients' DHI scale scores decreased in all dimensions and their quality of life improved[24]. Meanwhile, in addition to vestibular rehabilitation exercises, IMB model health education also intervened in some of the patients' high-risk factors, corrected their bad habits, and reduced the triggering factors of vertigo and dizziness, so that the patients' quality of life was improved[25].
The DHI scale and DHI-P, DHI-E and DHI-F scores were reduced in both groups after care in our study, and the scores in the care group were lower than those in the control group, with statistically significant differences. The reason for this analysis is that patients with vertigo often face dizziness attacks and somatic discomfort with unpredictable occurrence times, which seriously affect the ability to work and social activities, and cause mood changes that lead to physical and mental health disorders[26]. Vertigo treatment and vestibular rehabilitation exercises promoted vestibular function compensation and relieved patients' symptoms of vertigo and dizziness, therefore, patients' anxiety and depression were significantly improved[27]. Moreover, our study intervened with patients through three aspects: information, motivation, and behavioral skills, patients deepened their understanding of the disease, acquired skills to relieve symptoms, and through repeated communication and encouragement, patients received more attention and support, had more opportunities to express their concerns and worries, and their anxiety and depression were further relieved[28].
Our study has some innovation and some limitations. The patients included in our study were outpatients attending the clinic without hospital admission, the level of vertigo disability was mostly mild and moderate, and there were fewer severe patients; a stratified study should be conducted and inpatients should be included to make the data more comprehensive. Our study was limited by the time factor, the intervention time was only six weeks, and the follow-up and evaluation of long-term intervention effects were lacking. Our study only explored the effect of health education and guidance based on the IMB model on the rehabilitation of patients with unilateral vestibular hypofunction, and failed to comprehensively assess the reliability of care for patients with unilateral vestibular hypofunction, as well as failed to thoroughly study and follow up the rehabilitation of patients with unilateral vestibular hypofunction after care for a long period of time.
In conclusion, health education based on the IMB model can effectively improve patients' quality of life, increase self-efficacy of patients with unilateral hypovestibular function, enhance patients' confidence, enable patients to resume normal work and life as soon as possible, reduce patients' anxiety and depression, and effectively improve patients' psychological status.
Vestibular dysfunction (VH) can have a significant impact on a person's quality of life, as it can result in dizziness, imbalance, nausea, and fatigue. In addition, vestibular hypofunction can lead to a decrease in activity levels and an increase in anxiety and depression symptoms. As such, it is important for healthcare professionals to recognize the signs and symptoms of vestibular hypofunction and to provide appropriate treatment and support to patients who are experiencing these symptoms.
VH is a common concomitant of advanced peri-court disease and may be due to trauma, poisoning, infection, genetic and neurodegenerative changes, but the cause is unknown in about 50%. In recent years, with the increase of various unfavorable factors and the aging of the population, the incidence of vestibular vertigo has been increasing. The advantage of information-motivation-behavioral skills (IMB) model is that it integrates self-efficacy theory, draws on the understanding of motivation from rational behavior theory, integrates various factors that affect behavior, and has higher feasibility. Therefore, there is an urgent need to study the effects of health education based on the IMB model on the degree of vertigo, disability, anxiety and depression in patients with unilateral VH.
In order to explore the effect of health education based on the IMB model on vertigo, disability, anxiety, and depression in patients with unilateral VH, a study was conducted.
Patients with lateral VH from January 2019 to December 2021 were selected as the retrospective study objects and divided into control group (n = 40) and observation group (n = 40) according to nursing methods. The control group received usual care and health education guidance, and the observation group received health education and guidance based on the IMB model. Changes in self-efficacy, anxiety and depression were compared between the two groups.
Before nursing, there was no significant difference in General Self-Efficacy Scale, Hospital Anxiety and Depression Scale, anxiety and depression; they were higher/lower than those before nursing and lower than the control group, the difference was statistically significant. After nursing, the Dizziness Handicap Inventory (DHI) and DHI-P, DHI-E and DHI-F scores decreased in both groups; the nursing group was lower than the control group, and the difference was statistically significant.
IMB model-based health education can effectively improve patients 'quality of life, improve the self-efficacy of patients with unilateral vestibular function, enhance their self-confidence, restore their normal work and life as soon as possible, reduce patients' anxiety and depression, and effectively improve the psychological state of patients.
The treatment of VH remains challenging, and future research should depend on the type and severity of symptoms experienced by patients, which may involve vestibular rehabilitation therapy, medication, or surgical intervention.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Karras S, Greece S-Editor: Qu XL L-Editor: A P-Editor: Zheng XM
| 1. | Kim SH, Lee SY, Kim JS, Koo JW. Parameters of Off-Vertical Axis Rotation in Unilateral and Bilateral Vestibulopathy and Their Correlation with Vestibular Evoked Myogenic Potentials. J Clin Med. 2021;10. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 2. | Kitazawa M, Morita Y, Yagi C, Takahashi K, Ohshima S, Yamagishi T, Izumi S, Koizuka I, Horii A. Test Batteries and the Diagnostic Algorithm for Chronic Vestibular Syndromes. Front Neurol. 2021;12:768718. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 11] [Reference Citation Analysis (0)] |
| 3. | Abu-Halima M, Meese E, Saleh MA, Keller A, Abdul-Khaliq H, Raedle-Hurst T. MicroRNA-29b/c-3p Indicate Advanced Liver Fibrosis/Cirrhosis in Univentricular Heart Patients With and Without Fontan Palliation. Front Cardiovasc Med. 2020;7:619083. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 6] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Chen PY, Jheng YC, Huang SE, Po-Hung Li L, Wei SH, Schubert MC, Kao CL. Gaze shift dynamic visual acuity: A functional test of gaze stability that distinguishes unilateral vestibular hypofunction. J Vestib Res. 2021;31:23-32. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Micarelli A, Viziano A, Granito I, Micarelli RX, Felicioni A, Alessandrini M. Changes in body composition in unilateral vestibular hypofunction: relationships between bioelectrical impedance analysis and neuro-otological parameters. Eur Arch Otorhinolaryngol. 2021;278:2603-2611. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 4] [Cited by in RCA: 3] [Article Influence: 0.8] [Reference Citation Analysis (0)] |
| 6. | Idorn L, Olsen M, Jensen AS, Juul K, Reimers JI, Sørensen K, Johnsen SP, Søndergaard L. Univentricular hearts in Denmark 1977 to 2009: incidence and survival. Int J Cardiol. 2013;167:1311-1316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 31] [Cited by in RCA: 43] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 7. | Hall CD, Herdman SJ, Whitney SL, Anson ER, Carender WJ, Hoppes CW, Cass SP, Christy JB, Cohen HS, Fife TD, Furman JM, Shepard NT, Clendaniel RA, Dishman JD, Goebel JA, Meldrum D, Ryan C, Wallace RL, Woodward NJ. Vestibular Rehabilitation for Peripheral Vestibular Hypofunction: An Updated Clinical Practice Guideline From the Academy of Neurologic Physical Therapy of the American Physical Therapy Association. J Neurol Phys Ther. 2022;46:118-177. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 10] [Cited by in RCA: 149] [Article Influence: 37.3] [Reference Citation Analysis (0)] |
| 8. | Hillier S, McDonnell M. Is vestibular rehabilitation effective in improving dizziness and function after unilateral peripheral vestibular hypofunction? An abridged version of a Cochrane Review. Eur J Phys Rehabil Med. 2016;52:541-556. [PubMed] |
| 9. | Dunlap PM, Holmberg JM, Whitney SL. Vestibular rehabilitation: advances in peripheral and central vestibular disorders. Curr Opin Neurol. 2019;32:137-144. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 65] [Article Influence: 10.8] [Reference Citation Analysis (0)] |
| 10. | Erikssen G, Aboulhosn J, Lin J, Liestøl K, Estensen ME, Gjesdal O, Skulstad H, Døhlen G, Lindberg HL. Survival in patients with univentricular hearts: the impact of right versus left ventricular morphology. Open Heart. 2018;5:e000902. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 15] [Cited by in RCA: 25] [Article Influence: 3.6] [Reference Citation Analysis (0)] |
| 11. | Paul SS, Dibble LE, Walther RG, Shelton C, Gurgel RK, Lester ME. Reduced Purposeful Head Movements During Community Ambulation Following Unilateral Vestibular Loss. Neurorehabil Neural Repair. 2018;32:309-316. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 12. | Sasaki T, Asou T, Takeda Y, Onakatomi Y, Tominaga T, Yamamoto Y. Extracorporeal life support after cardiac surgery in children: outcomes from a single institution. Artif Organs. 2014;38:34-40. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 22] [Article Influence: 1.8] [Reference Citation Analysis (0)] |
| 13. | Hautala J, Gissler M, Ritvanen A, Vahlberg T, Ojala T. Monthly variation in univentricular heart and transposition of the great arteries - 10-year national population-based cohort study. Eur J Obstet Gynecol Reprod Biol. 2021;258:418-423. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Micarelli A, Viziano A, Micarelli B, Di Fulvio G, Alessandrini M. Usefulness of postural sway spectral analysis in the diagnostic route and clinical integration of cervicogenic and vestibular sources of dizziness: A cross-sectional preliminary study. J Vestib Res. 2021;31:353-364. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Alessandrini M, Viziano A, Pistillo R, Granito I, Basso L, Preziosi N, Micarelli A. Changes in daily energy expenditure and movement behavior in unilateral vestibular hypofunction: Relationships with neuro-otological parameters. J Clin Neurosci. 2021;91:200-208. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.5] [Reference Citation Analysis (0)] |
| 16. | Micarelli A, Viziano A, Pistillo R, Granito I, Micarelli B, Alessandrini M. Sleep Performance and Chronotype Behavior in Unilateral Vestibular Hypofunction. Laryngoscope. 2021;131:2341-2347. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 3] [Reference Citation Analysis (0)] |
| 17. | Meldrum D, Jahn K. Gaze stabilisation exercises in vestibular rehabilitation: review of the evidence and recent clinical advances. J Neurol. 2019;266:11-18. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 29] [Article Influence: 4.8] [Reference Citation Analysis (0)] |
| 18. | Meldrum D, Burrows L, Cakrt O, Kerkeni H, Lopez C, Tjernstrom F, Vereeck L, Zur O, Jahn K. Vestibular rehabilitation in Europe: a survey of clinical and research practice. J Neurol. 2020;267:24-35. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 12] [Cited by in RCA: 28] [Article Influence: 5.6] [Reference Citation Analysis (0)] |
| 19. | Pérez-Fernández N, Alvarez-Gomez L, Manrique-Huarte R. Bilateral Vestibular Hypofunction in the Time of the Video Head Impulse Test. Audiol Neurootol. 2020;25:72-78. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 2] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 20. | Sestak A, Maslovara S, Zubcic Z, Vceva A. Influence of vestibular rehabilitation on the recovery of all vestibular receptor organs in patients with unilateral vestibular hypofunction. NeuroRehabilitation. 2020;47:227-235. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 2] [Cited by in RCA: 6] [Article Influence: 1.2] [Reference Citation Analysis (0)] |
| 21. | Likhachev SA, Maryenko IP. [Statokinetic characteristics of vestibular dysfunction in patients with vascular compression of the cochleo-vestibular nerve]. Zh Nevrol Psikhiatr Im S S Korsakova. 2015;115:35-39. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 22. | Castellucci A, Malara P, Brandolini C, Del Vecchio V, Giordano D, Ghidini A, Ferri GG, Pirodda A. Isolated horizontal canal hypofunction differentiating a canalith jam from an acute peripheral vestibular loss. Am J Otolaryngol. 2019;40:319-322. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 18] [Cited by in RCA: 26] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 23. | Barreto RG, Yacovino DA, Cherchi M, Nader SN, Teixeira LJ, Silva DAD, Verdecchia DH. The Role of the Smartphone in the Diagnosis of Vestibular Hypofunction: A Clinical Strategy for Teleconsultation during the COVID-19 Pandemic and Beyond. Int Arch Otorhinolaryngol. 2021;25:e602-e609. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 8] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 24. | Ramos BF, Cal R, Carmona S, Weber KP, Zuma E Maia F. Corrective Saccades in Unilateral and Bilateral Vestibular Hypofunction During Slow Rotation Expressed by Visually Enhanced VOR and VOR Suppression: Role of the Cerebellum. Cerebellum. 2021;20:673-677. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 3] [Cited by in RCA: 4] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 25. | Balami AD, Said SM, Zulkefli NAM, Norsa'adah B, Audu B. Improving malaria preventive practices and pregnancy outcomes through a health education intervention: A randomized controlled trial. Malar J. 2021;20:55. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 8] [Cited by in RCA: 6] [Article Influence: 1.5] [Reference Citation Analysis (0)] |
| 26. | Porta Etessam J, González N, García-Azorín D, Silva L. Bilateral vestibular hypofunction occurring between migraine attacks: toward an integrative hypothesis. Neurologia (Engl Ed). 2020;35:448-449. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 27. | Stewart CE, Bauer DS, Altschuler RA, King WM. Transient peripheral vestibular hypofunction measured with vestibular short-latency evoked potentials following noise exposure in rats. J Neurophysiol. 2021;126:1547-1554. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 28. | Chow MR, Ayiotis AI, Schoo DP, Gimmon Y, Lane KE, Morris BJ, Rahman MA, Valentin NS, Boutros PJ, Bowditch SP, Ward BK, Sun DQ, Treviño Guajardo C, Schubert MC, Carey JP, Della Santina CC. Posture, Gait, Quality of Life, and Hearing with a Vestibular Implant. N Engl J Med. 2021;384:521-532. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 33] [Cited by in RCA: 69] [Article Influence: 17.3] [Reference Citation Analysis (0)] |