Published online Feb 16, 2024. doi: 10.12998/wjcc.v12.i5.1029
Peer-review started: October 26, 2023
First decision: December 7, 2023
Revised: December 12, 2023
Accepted: January 24, 2024
Article in press: January 24, 2024
Published online: February 16, 2024
Processing time: 96 Days and 19.8 Hours
Radiological imaging findings may contribute to the differentiation of malignant biliary obstruction from choledocholithiasis in the etiology of acute cholangitis.
Core Tip: In malignant biliary obstructions, irregular walls, increased wall thickness, and blunt termination are seen in the choledochal duct. In choledocholithiasis, stones are seen in the lumen and the choledochal walls are regular.
- Citation: Aydin S, Irgul B. Response letter to “Acute cholangitis: Does malignant biliary obstruction vs choledocholithiasis etiology change the outcomes?” with imaging aspects. World J Clin Cases 2024; 12(5): 1029-1032
- URL: https://www.wjgnet.com/2307-8960/full/v12/i5/1029.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i5.1029
We were intrigued by the paper “Acute cholangitis: Does malignant biliary obstru
In the current era of medical imaging, which offers a wide range of imaging techniques from basic radiographs to advanced magnetic resonance imaging (MRI) scans, the role of the radiologist is to assist the physician in choosing the appropriate imaging method and addressing important patient care issues. Ultrasound (US) is used as a preliminary method to screen for biliary obstruction, but it cannot accurately establish the severity and cause of obstructive jaundice. Therefore, further imaging with techniques like contrast enhanced computerized tomography and magnetic resonance cholangiopancreatography (MRCP) are necessary as they are more effective in providing accurate diagnostic information. MRCP has become the preferred method for examining biliary obstruction, with endoscopic retrograde cholangiopancreatography being reserved for patients who are more likely to require therapeutic intervention[2].
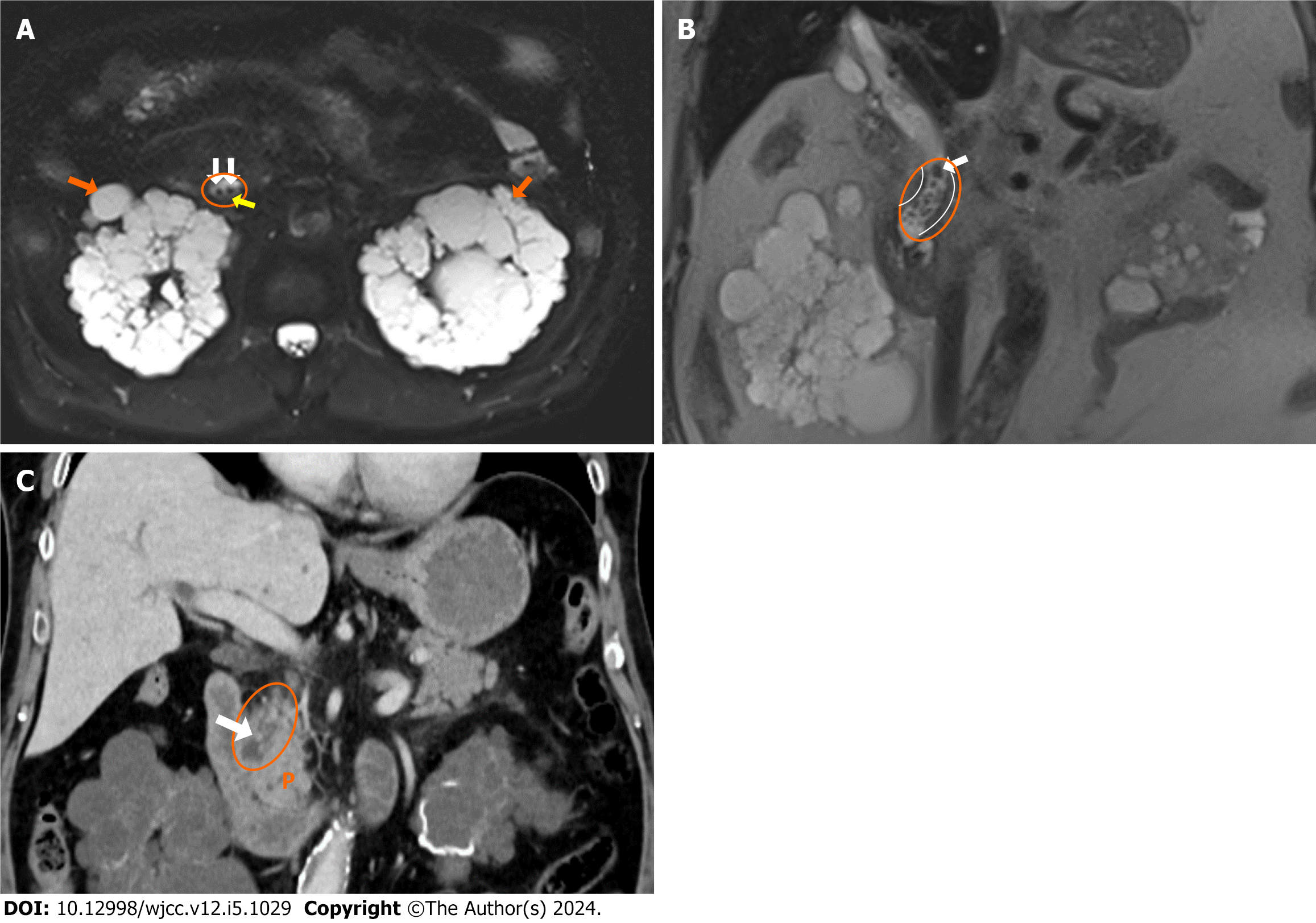
The Tokyo Guidelines are employed for the diagnosis of acute cholangitis. According to these criteria, acute cholangitis can be diagnosed based on signs of systemic inflammation, cholestasis, and imaging results[3]. Calculi and dilatation can be observed in the bile ducts on US and computed tomography (CT) scans due to the presence of stones in acute cholangitis caused by choledocholithiasis. MRCP scans reveal signal attenuation caused by the presence of calculi. The bile duct walls exhibit a rather slender and sleek shape[4] (Figure 1).
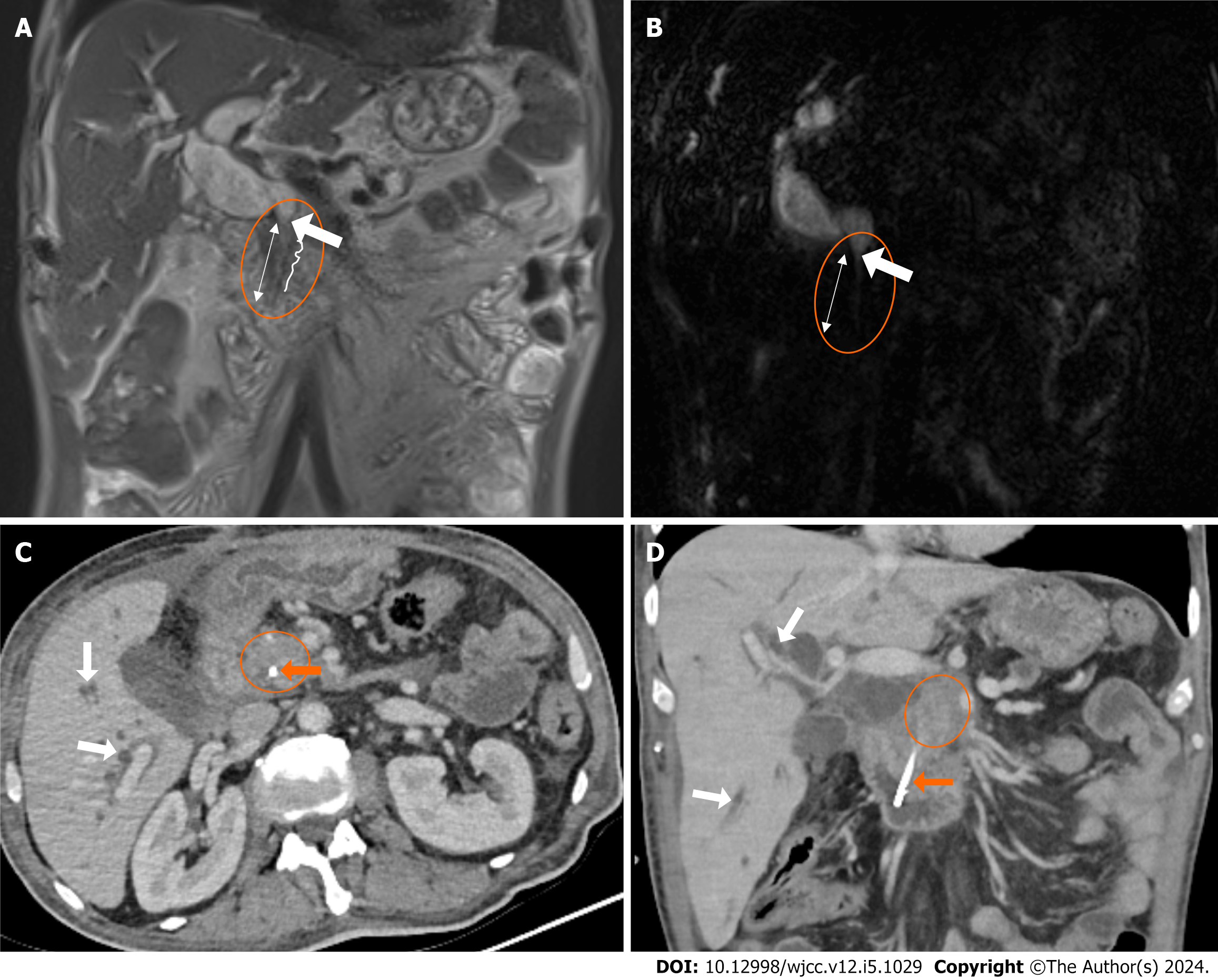
Acute cholangitis caused by malignant biliary obstructions is characterized by the enlargement of the biliary tract, which can be detected using US, CT, and MRCP, similar to the presentation in cases of choledocholithiasis. Furthermore, intraductal mass lesions are present, with extensive segments of contrasting bile duct walls that are uneven and thicker (> 1.5 mm). Additionally, blunt terminations in the bile ducts caused by distal tumoral lesions are visible[4] (Figure 2).
In conclusion, while certain imaging findings have been identified to distinguish between cancer and stone-induced blockages, there is currently no universally accepted approach or finding to definitively differentiate between the two. If a routinely used imaging modality like MRCP reveals any secondary finding that indicates malignant blockage, multiphase-dynamic CT/MRI is recommended for optimal evaluation of nearby organs such as the biliary system and pancreas. In addition, US is sufficient to explain the etiology of biliary obstructions such as stones. When the cause of obstruction cannot be found with US, second- and third-level imaging techniques such as CT, MRI, or endoscopic ultrasonography are needed; however, their unnecessary overuse should be avoided.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: Turkey
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): E
P-Reviewer: Dabbous H, Egypt; Salerno R, Italy; Wen XL, China S-Editor: Qu XL L-Editor: Filipodia P-Editor: Zhao S
| 1. | Tsou YK, Su YT, Lin CH, Liu NJ. Acute cholangitis: Does malignant biliary obstruction vs choledocholithiasis etiology change the clinical presentation and outcomes? World J Clin Cases. 2023;11:6984-6994. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 6] [Reference Citation Analysis (0)] |
| 2. | Joshi A, Rajpal K, Kakadiya K, Bansal A. Role of CT and MRCP in Evaluation of Biliary Tract Obstruction. Curr Radiol Rep. 2014;72:2. [RCA] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 1] [Article Influence: 0.1] [Reference Citation Analysis (0)] |
| 3. | Kiriyama S, Kozaka K, Takada T, Strasberg SM, Pitt HA, Gabata T, Hata J, Liau KH, Miura F, Horiguchi A, Liu KH, Su CH, Wada K, Jagannath P, Itoi T, Gouma DJ, Mori Y, Mukai S, Giménez ME, Huang WS, Kim MH, Okamoto K, Belli G, Dervenis C, Chan ACW, Lau WY, Endo I, Gomi H, Yoshida M, Mayumi T, Baron TH, de Santibañes E, Teoh AYB, Hwang TL, Ker CG, Chen MF, Han HS, Yoon YS, Choi IS, Yoon DS, Higuchi R, Kitano S, Inomata M, Deziel DJ, Jonas E, Hirata K, Sumiyama Y, Inui K, Yamamoto M. Tokyo Guidelines 2018: diagnostic criteria and severity grading of acute cholangitis (with videos). J Hepatobiliary Pancreat Sci. 2018;25:17-30. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 468] [Cited by in RCA: 425] [Article Influence: 60.7] [Reference Citation Analysis (0)] |
| 4. | Choi SH, Han JK, Lee JM, Lee KH, Kim SH, Lee JY, Choi BI. Differentiating malignant from benign common bile duct stricture with multiphasic helical CT. Radiology. 2005;236:178-183. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 90] [Cited by in RCA: 85] [Article Influence: 4.3] [Reference Citation Analysis (0)] |