Published online Feb 16, 2024. doi: 10.12998/wjcc.v12.i5.1010
Peer-review started: November 24, 2023
First decision: December 18, 2023
Revised: January 2, 2024
Accepted: January 15, 2024
Article in press: January 15, 2024
Published online: February 16, 2024
Processing time: 67 Days and 17.8 Hours
Ultrasound guide technology, which can provide real-time visualization of the needle tip and tissues and avoid many adverse events, is widely used in mini
A 65-year-old patient complained of low back pain accompanied occasionally by pain and numbness in the left lower limb. Physical examination showed ten
This is the first report on the LRS treatment with ultrasound-guided LRB from the contralateral spinous process along the inner side of the articular process by out-plane technique. Further studies are expected to investigate the efficacy and safety of ultrasound-guided LRB for patients with LRS.
Core Tip: Lateral recess block (LRB) is a common treatment method for lateral recess stenosis (LRS). However, it is an unsatisfactory method because of its high risk of side effects. Ultrasound-guided technology is widely used in minimally invasive therapy, but only a few studies have reported its use in LRB, this is probably because there is no recognized standard method for ultrasound scanning. In order to explore the standard method for ultrasound-guided LRB, we reported a novel ultrasound-guided LRB approach in treating a patient with LRS whose symptoms significantly improved without any complications.
- Citation: Yang J, Li XL, Li QB. Novel approach of ultrasound-guided lateral recess block for a patient with lateral recess stenosis: A case report. World J Clin Cases 2024; 12(5): 1010-1017
- URL: https://www.wjgnet.com/2307-8960/full/v12/i5/1010.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i5.1010
Lateral recess stenosis (LRS) is a common type of lumbar spinal stenosis in elderly individuals[1,2]. In spinal anatomy, the lateral recess is the outermost region of the spinal canal bordered laterally by the pedicle, posteriorly by the superior articular facet and ligamentum flavum, and anteriorly by the vertebral body, endplate, and disc margin[3], which is considered stenotic when the anteroposterior measurement is < 4 mm[4]. Due to the close proximity within the spinal canal, stenosis in this region always leads to low back pain, numbness, neurogenic claudication and even urination-defecation impairment[2], which often affect mobility and walking ability, leading to a reduction in patients’ quality of life[3,5]. Lateral recess block (LRB) is commonly used for this condition due to its immediate analgesic effect in approximately 50%–87% of patients[6,7]. To improve efficacy and accuracy, computed tomography (CT), X-ray, and ultrasound guidance are widely used in minimally invasive therapy[8]. However, the studies on ultrasound-guided LRB are limited, this is probably because there is no recognized standard method for ultrasound scanning.
We reported a successful case of a patient with LRS who underwent ultrasound-guided LRB. This case report may provide a new exploration of the standard method of ultrasound-guided LRB. This study followed the CARE Guidelines for consensus-based clinical case reporting guideline development[9].
A 65-year-old patient complained of low back pain accompanied occasionally by pain and numbness in the left lower limb for at least 10 years.
In the past 10 years, his symptoms did not significantly affect his life and work and were relieved after rest or massage therapy. However, his low back pain gradually worsened, and he developed persistent soreness, numbness, and intermittent claudication on the left lower limb, mainly at the lateral thigh, posterolateral, instep, and foot top. Consequently, his life and work were severely affected because his symptoms were unrelieved even after rest or massage.
His medical history was unremarkable.
His family history was also unremarkable.
Physical examination showed tenderness on the spinous process and paraspinal muscles from L1 to S1, extensor hallucis longus and tibialis anterior weakness (muscle strength: 4−), and a positive straight leg raising test in the left lower limb (60°). The visual analog scale (VAS) and Oswestry disability index (ODI) were 8 mm and 51%, respectively.
No laboratory tests.
Magnetic resonance imaging (MRI) indicated L4–L5 disc degeneration with left LRS and nerve root entrapment (Figure 1).
Based on the clinical and imaging examination, the patient was diagnosed with LRS.
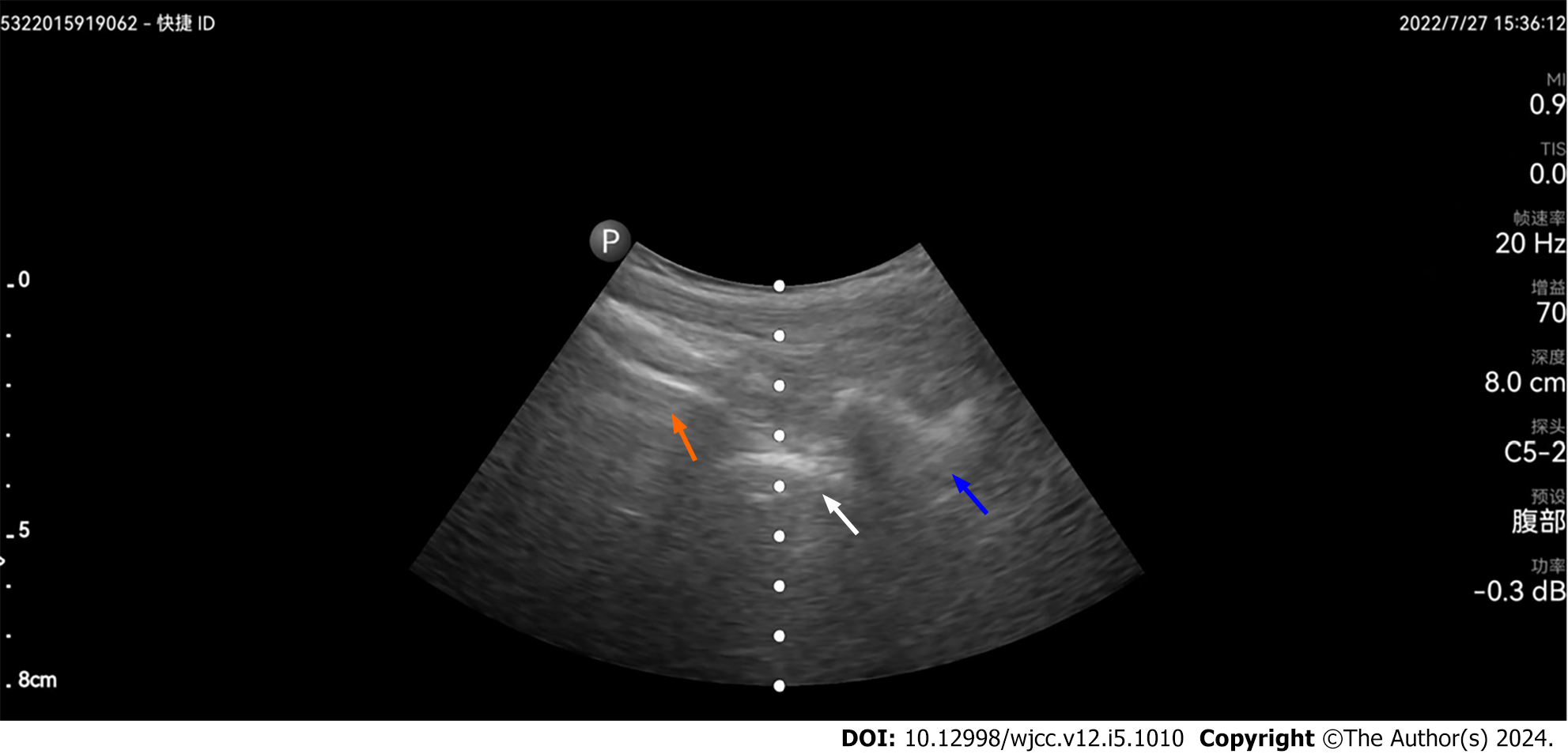
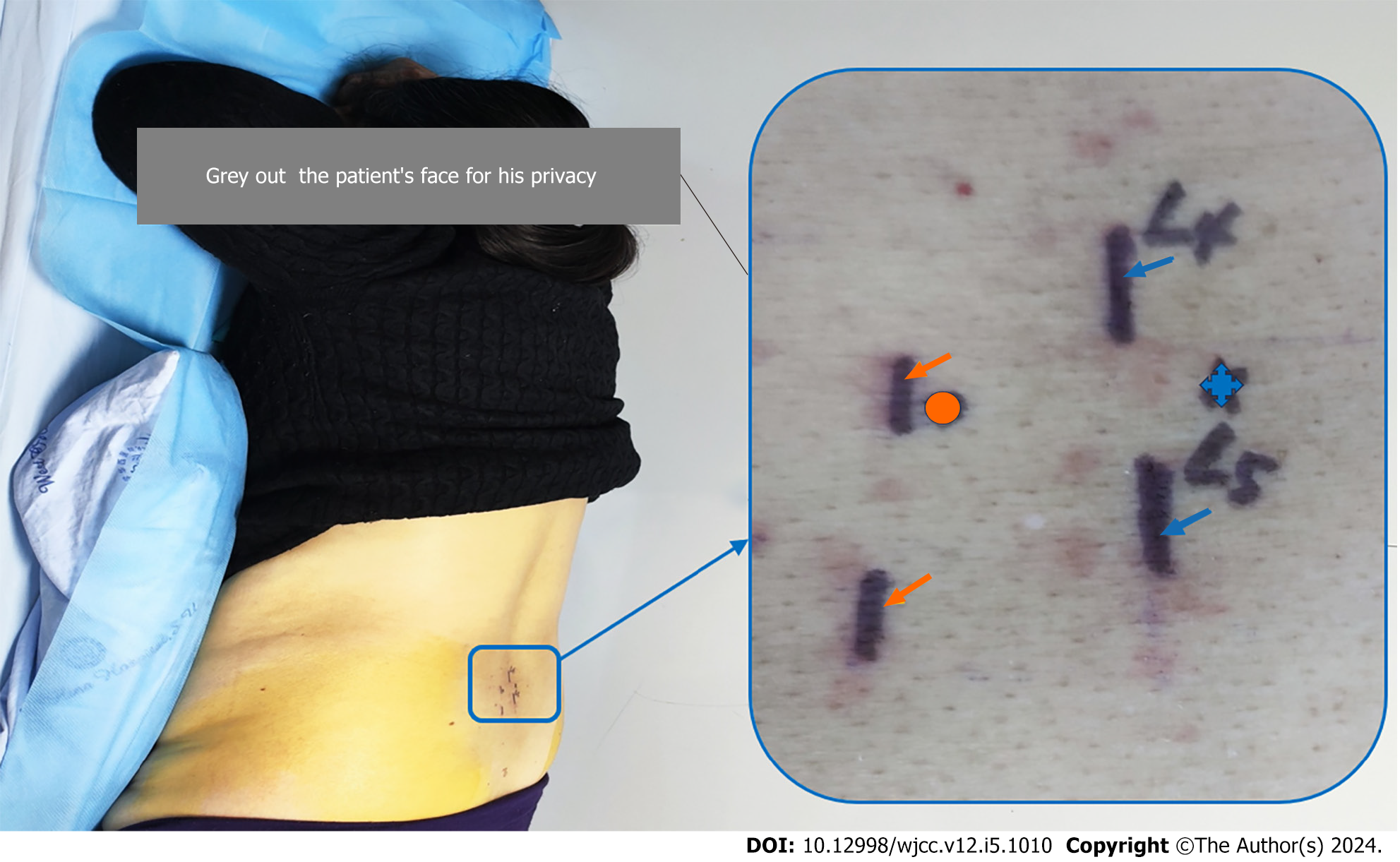
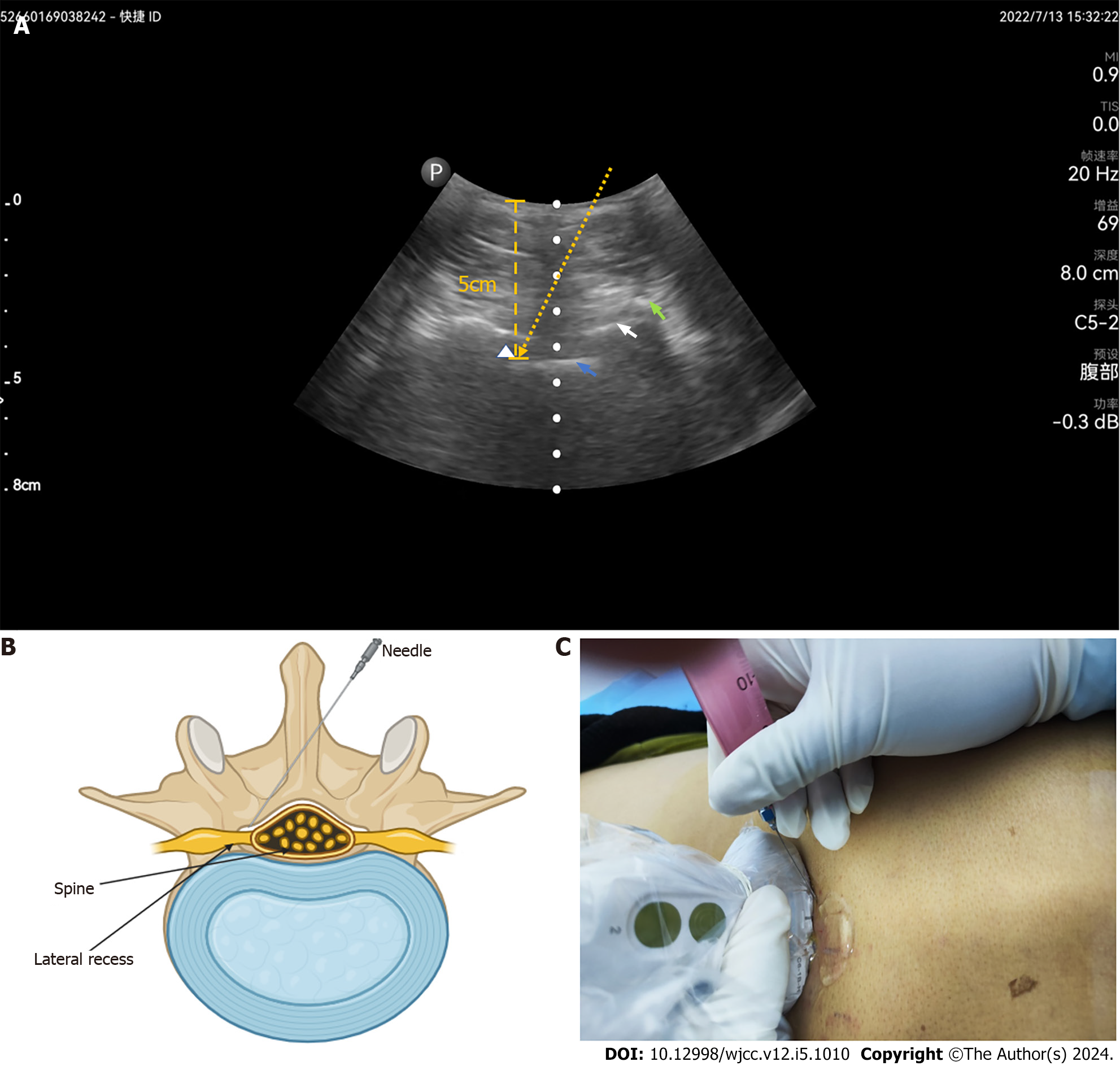
Oral analgesics and physiotherapy did not benefit the patient. Therefore, we planned to perform left L4–L5 LRB under ultrasound guidance. We used a portable ultrasound imaging device (Lumify, Philips, Shanghai, China) with a 5-2 MHz frequency round probe. Before the procedure, the patient was placed in a prone position with a pillow under the lower abdomen to reduce lumbar lordosis in the operating room and supervised via a continuous electrocardiogram, and his blood pressure and pulse oximetry were supervised using a noninvasive monitor. After the involved lumbar intervertebral space between L4 and L5 was confirmed, the physician’s hands, puncture sites, and ultrasound probe were sterilized. The physician stood on the left side of the patient. Subsequently, ultrasound-guided LRB was divided into four steps. First, the target L4 articular process was identified by locating the lumbosacral junction (L5-S1 gap; Figure 2) on paramedian sagittal scanning, and counting was performed cranially by numbering the lamina and transverse processes of the L5 and L4 vertebrae. Second, after marking the L4 vertebral level, the probe was rotated transversely to obtain the view of the L4 spinous process and interspinous process space between L4 and L5. Third, the probe was slightly moved toward the median line to obtain the view of the articular process, ligamentum flavum, and intraspinal anterior complex (posterior longitudinal ligament, dura mater and lumbar posterior margin) on median axis scanning. The puncture site was 0.8-1.0 cm away from the contralateral spinous process of L4 and L5 (Figure 3). Fourth, the puncture site was infiltrated using 1% lidocaine before insertion. Afterward, a needle was advanced along with the inner side of the articular process at 70°–80° guided by ultrasound in the out-plane technique. The lateral recess of L4 was the target of the needle tip. The needle was withdrawn to exclude vascular injection after the needle tip site was verified under ultrasound, and no blood or cerebrospinal fluid was aspirated. Hypoesthesia of the left medial malleolus was observed 5 min after injection of 2 mL of 0.25% lidocaine. Subsequently, 5 mL mixed injectate consisting of 1 mL triamcinolone, 4 mL 2% lidocaine, 1 mL mecobalamin and 14 mL 0.9% sodium chloride was injected into the lateral recess of L4. To display the needle trajectory more clearly, we used a diagram to illustrate the needle trajectory (Figure 4), but it was difficult to capture the ultrasonic image of the needle during the operation.
We carefully recorded the change in the patient’s symptoms with VAS and ODI before and 30 min, 1 wk, 1 month, and 3 months postoperatively. The patient’s symptoms greatly improved 1 wk postoperatively and at the 3-month follow-up (Table 1). The patient was satisfied with this treatment.
| Item | Pre-operation | 30 min postoperation | 1 wk postoperation | 1 month postoperation | 3 months postoperation |
| VAS | 8 | 6 | 4 | 4 | 5 |
| ODI, % | 51 | 51 | 31 | 31 | 33 |
We reported a novel approach of ultrasound-guided LRB for LRS treatment. We preliminarily established that ultrasound-guided LRB from the contralateral spinous process along with the inner side of the articular process with the out-plane technique is an effective, accurate, and safe method in LRS treatment.
Surgery, a commonly used treatment method, showed superior outcomes[10]. However, its complications and less satisfaction with the results of surgery in the elderly population make it a difficult choice for clinicians[11]. Thus, nonsurgical treatment is appropriate for patients with mild to moderate symptoms. Some of the commonly used treatment strategies include medication, physical therapy, massage, conventional transforaminal epidural steroid injection (CTFESI), selected nerve root block (SNRB), and LRB[12-17]. Medication, physical therapy, and massage are unsatisfactory choices because of their short-term effect and high recurrence rate[15]. CTFESI and SNRB are widely used in LRS treatment[16]; However, the effective rate of SNRB for patients with LRS has not been satisfactory due to the stenosis pathology occurring in the intraspinal lateral recess but not in the intervertebral foramen outside the spinal canal[8]. Generally, the injectate includes local anesthetics and glucocorticoids. Local anesthetics can achieve analgesic effects by blocking neurological activity. Meanwhile, glucocorticoids reduce inflammation and the immune response by inhibiting prostaglandin synthesis, reducing nociceptor stimulation and sensitization, and decreasing inflammatory mediator release. In addition, it plays an indirect role in decompressing and increasing the blood supply to the nerve, which alleviates the patient’s symptoms[18]. Therefore, accurate injection of the lateral recess is key to successful LRS treatment. The most common technique of SNRB is targeting the spinal nerve root[16], which is physically distant from the spinal nerve root to the lateral recess[2]. The injectate diffuses from the spinal nerve root to the lateral recess, resulting in a slow effect and weak efficacy, which leads to less satisfaction. Moreover, a retrospective study[7] reported that LRB was considerably safer, with a lower chance of nerve pricks[19] and intravascular dye spread than CTFESI. This study also revealed that a single LRB was significantly better than a single CTFESI in decreasing unilateral radiculopathy pain because the site of drug deposition was more proximal to the discovery interface.
LRB is effective in relieving pain and symptoms of nerve root entrapment[11,13]. However, the potential risk of subdural block, failure block, and intraspinal bleeding still makes it an entangled choice for many physicians[8]. CT, X-ray, and ultrasound guidance are widely used in minimally invasive therapy to improve efficacy, safety, and accuracy[8,16]. Exposure to radiation during the procedure under CT or X-ray guidance may be a problem. Sacaklidir et al[20] reported that radiation exposure for 37.3–46.7s results in a radiation dose between 0.057 and 0.218 mGym2. This is equivalent to 15–30 chest radiographs. Because of its real-time visualization of the needle tip and no radiation exposure, ultrasound-guided minimally invasive techniques have been widely adapted in clinical practice. Li et al[21] reported the efficacy of ultrasound-guided nerve blocks of the head and neck for chronic pain management. Takahashi et al[22] validated the efficacy of ultrasound-guided cervical nerve root block for frozen shoulder. However, only a few studies have reported ultrasound-guided LRB due to the lack of precise ultrasound scanning methods. Currently, no standard method of ultrasound-guided LRB exists. In our practice, we selected a new method. A previous study selected an injection point 0.8–1.0 cm away from the ipsilateral spinous process and then along the inner side of the articular pillar under ultrasound guidance[8]. This method increases the risk of total spinal paralysis caused by subdural block, particularly when LRS is associated with nerve root adhesion. In this case, the injection points were 0.8-1.0 cm away from the contralateral spinous process of L4 and L5. Then, the needle was advanced toward the inner side of the articular process at 70°–80° guided by ultrasound with the out-plane technique. This method increases the effectiveness, safety, and accuracy of surgery for patients and provides a new exploration into the standard method of ultrasound-guided LRB.
There are also some limitations in this study. It is difficult for us to capture the ultrasonic image of the needle during the operation. The lack of the ultrasonic image would decrease the illustration of this technology. Hence, we used a diagram to illustrate the needle trajectory in Figure 4. We expect that this image will help understand our needle trajectory more clearly. Moreover, we only reported one successful case, which may restrict the wide use of ultrasound-guided LRB. Further high-quality studies are expected to confirm the efficacy and safety of the use of ultrasound-guided LRB with this novel approach.
In conclusion, this study is the first report of the use of ultrasound-guided LRB from the contralateral spinous process along with the inner side of the articular process with the out-plane technique for LRS treatment, which was preliminarily proven to be effective, accurate, and safe. Further studies are needed to investigate the efficacy and safety of ultrasound-guided LRB for patients with LRS.
We reported a case of a patient with LRS who underwent ultrasound-guided LRB. This study is the first report of ultrasound-guided LRB from the contralateral spinous process along with the inner side of the articular process with the out-plane technique for LRS treatment. Further studies are expected to investigate the efficacy and safety of ultrasound-guided LRB for patients with LRS.
We would like to thank the patient for agreeing to participate in this study.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Corresponding Author's Membership(s) in Professional Societies: British Medical Acupuncture Society, 38259.
Specialty type: Integrative and complementary medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Gousheh M, Iran S-Editor: Liu JH L-Editor: A P-Editor: Yu HG
| 1. | Wang X, Wu L, Zhao K, Chen D, Su B, Kong Y, Li J, Kang K, Si D. Trephine-based foraminoplasty in PTED treatment of lumbar lateral recess stenosis. Adv Clin Exp Med. 2022;31:359-367. [RCA] [PubMed] [DOI] [Full Text] [Reference Citation Analysis (0)] |
| 2. | Deer TR, Grider JS, Pope JE, Lamer TJ, Wahezi SE, Hagedorn JM, Falowski S, Tolba R, Shah JM, Strand N, Escobar A, Malinowski M, Bux A, Jassal N, Hah J, Weisbein J, Tomycz ND, Jameson J, Petersen EA, Sayed D. Best Practices for Minimally Invasive Lumbar Spinal Stenosis Treatment 2.0 (MIST): Consensus Guidance from the American Society of Pain and Neuroscience (ASPN). J Pain Res. 2022;15:1325-1354. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 21] [Reference Citation Analysis (0)] |
| 3. | Lee BH, Moon SH, Suk KS, Kim HS, Yang JH, Lee HM. Lumbar Spinal Stenosis: Pathophysiology and Treatment Principle: A Narrative Review. Asian Spine J. 2020;14:682-693. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 17] [Cited by in RCA: 65] [Article Influence: 13.0] [Reference Citation Analysis (0)] |
| 4. | Liu X, Peng Y, Pei L, Zhu Y. Sufficient Lumbar Lateral Recess Decompression Acquired by Undercutting "Superior Articular Process Neck" Plus Intervertebral Disk Annuloplasty in Percutaneous Transforaminal Endoscopic Surgery. Med Sci Monit. 2020;26:e921119. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Reference Citation Analysis (0)] |
| 5. | Cheng X, Zhang K, Sun X, Zhao C, Li H, Ni B, Zhao J. Clinical and radiographic outcomes of bilateral decompression via a unilateral approach with transforaminal lumbar interbody fusion for degenerative lumbar spondylolisthesis with stenosis. Spine J. 2017;17:1127-1133. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 19] [Cited by in RCA: 32] [Article Influence: 4.0] [Reference Citation Analysis (0)] |
| 6. | Thiengwittayaporn S, Koompong P, Khamrailert S, Wetpiriyakul P. Comparison of Clinical Outcomes of Different Rates of Infusion in Caudal Epidural Steroid Injection: A Randomized Controlled Trial. Asian Spine J. 2021;15:244-251. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 1] [Reference Citation Analysis (0)] |
| 7. | Jain A, Agarwal A, Jain S, Waindeskar V. Comparison Between a Single Subpedicular Transforaminal Epidural Steroid Injection and Lateral Recess Steroid Injection in Reducing Paracentral Disc Herniation-Related Chronic Neuropathic Leg Pain: A Retrospective Study. World Neurosurg. 2021;149:e392-e399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 4] [Reference Citation Analysis (0)] |
| 8. | Liang G. Effect of ultrasound-guided lateral recess block in the treatment of patients with lumbar intervertebral disc herniation. Hennan Medical Research. 2021;30:1638-1640. |
| 9. | Gagnier JJ, Kienle G, Altman DG, Moher D, Sox H, Riley D; CARE Group. The CARE guidelines: consensus-based clinical case reporting guideline development. Headache. 2013;53:1541-1547. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 347] [Cited by in RCA: 864] [Article Influence: 78.5] [Reference Citation Analysis (0)] |
| 10. | Lurie J, Tomkins-Lane C. Management of lumbar spinal stenosis. BMJ. 2016;352:h6234. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 368] [Cited by in RCA: 343] [Article Influence: 38.1] [Reference Citation Analysis (0)] |
| 11. | Li X, Liu T, Fan J, Zhang H, Yang C, Yin X, Gao H, Qian J, Sun S. Outcome of lumbar lateral recess stenosis with percutaneous endoscopic transforaminal decompression in patients 65 years of age or older and in younger patients. Medicine (Baltimore). 2020;99:e21049. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 3] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 12. | Chen X, Zheng Z, Lin J. Clinical Effectiveness of Conservative Treatments on Lumbar Spinal Stenosis: A Network Meta-Analysis. Front Pharmacol. 2022;13:859296. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 1] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 13. | Kim HJ, Kim JH, Park YS, Suk KS, Lee JH, Park MS, Moon SH. Comparative study of the efficacy of limaprost and pregabalin as single agents and in combination for the treatment of lumbar spinal stenosis: a prospective, double-blind, randomized controlled non-inferiority trial. Spine J. 2016;16:756-763. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 27] [Article Influence: 3.0] [Reference Citation Analysis (0)] |
| 14. | Jang JH, Lee WY, Kim JW, Cho KR, Nam SH, Park Y. Ultrasound-Guided Selective Nerve Root Block versus Fluoroscopy-Guided Interlaminar Epidural Block versus Fluoroscopy-Guided Transforaminal Epidural Block for the Treatment of Radicular Pain in the Lower Cervical Spine: A Retrospective Comparative Study. Pain Res Manag. 2020;2020:9103421. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 9] [Cited by in RCA: 27] [Article Influence: 5.4] [Reference Citation Analysis (0)] |
| 15. | Zhang Y. Effects of lateral recess block on pain and functional recovery in patients with lumbar disc herniation. Shiyong Zhongxiyi Jiehe Linchuang. 2020;20:28-29. |
| 16. | Yue B, Shen F, Ye ZF, Wang ZH, Yang HL, Jiang GQ. Accurate location and minimally invasive treatment of lumbar lateral recess stenosis with combined SNRB and PTED. J Int Med Res. 2020;48:300060519884817. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 1] [Article Influence: 0.2] [Reference Citation Analysis (0)] |
| 17. | Schneider MJ, Ammendolia C, Murphy DR, Glick RM, Hile E, Tudorascu DL, Morton SC, Smith C, Patterson CG, Piva SR. Comparative Clinical Effectiveness of Nonsurgical Treatment Methods in Patients With Lumbar Spinal Stenosis: A Randomized Clinical Trial. JAMA Netw Open. 2019;2:e186828. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 45] [Cited by in RCA: 60] [Article Influence: 10.0] [Reference Citation Analysis (0)] |
| 18. | Guyot JP. Lumbar Selective Nerve Root Block: Comparative Study Using Two Pharmacological Formulae. Global Spine J. 2018;8:374-377. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 5] [Cited by in RCA: 9] [Article Influence: 1.3] [Reference Citation Analysis (0)] |
| 19. | Kim HJ, Park JH, Shin KM, Kang SS, Kim IS, Hong SJ, Song CK, Park JC, Yeom JS. The efficacy of transforaminal epidural steroid injection by the conventional technique in far-lateral herniation of lumbar disc. Pain Physician. 2012;15:415-420. [PubMed] |
| 20. | Sacaklidir R, Ozturk EC, Sencan S, Gunduz OH. Radiation Doses for Different Approaches of Fluoroscopy-Guided Epidural Injections: An Observational Clinical Study. Pain Physician. 2022;25:E67-E72. [PubMed] |
| 21. | Li J, Szabova A. Ultrasound-Guided Nerve Blocks in the Head and Neck for Chronic Pain Management: The Anatomy, Sonoanatomy, and Procedure. Pain Physician. 2021;24:533-548. [PubMed] |
| 22. | Takahashi R, Kajita Y, Harada Y, Iwahori Y, Miyashita N, Deie M. Does the timing of shoulder manipulation under ultrasound-guided cervical nerve root block for frozen shoulder affect the clinical outcome? J Orthop Sci. 2022;27:122-125. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Cited by in RCA: 3] [Article Influence: 1.0] [Reference Citation Analysis (0)] |