Published online Feb 6, 2024. doi: 10.12998/wjcc.v12.i4.828
Peer-review started: October 16, 2023
First decision: December 5, 2023
Revised: December 22, 2023
Accepted: January 15, 2024
Article in press: January 15, 2024
Published online: February 6, 2024
Processing time: 101 Days and 4.1 Hours
Pedicled abdominal flaps are a widely used surgical technique for forearm reconstruction in patients with soft tissue defects. However, some drawbacks include restricted flap size, partial flap loss, and donor-site morbidity. To address these concerns, we present a case of a pedicled abdominal flap using the deep inferior epigastric artery perforators (DIEP) for forearm reconstruction in a patient with a large soft tissue defect.
A 46-year-old male patient was admitted to our hospital with forearm injury caused by a pressing machine. A 15 cm × 10 cm soft tissue defect with complete rupture of the ulnar side structures of the forearm was found. One week after orthopedic management of the neurovascular injury and fractures using the first stage of Masquelet technique, the patient was referred to the plastic and recon
Pedicled abdominal flap using the DIEP provides a reliable option for forearm reconstruction in patients with large soft tissue defects.
Core Tip: Compared to traditional pedicled groin and abdominal flaps for forearm reconstruction, pedicled abdominal flap with the deep inferior epigastric artery perforators offer a more robust blood supply and larger soft tissue, reducing the risk of flap necrosis. In addition, it eliminates the need for anastomoses, reduces operative time, and allows direct closure of the donor site aesthetically without skin grafts. Using computed tomography angiography and handheld Doppler can help surgeons find appropriate perforators vessels during surgery. This report provides a suitable option for managing complex upper extremity injuries and providing adequate soft tissue coverage with minimal donor-site morbidity.
- Citation: Jeon JH, Kim KW, Jeon HB. Pedicled abdominal flap using deep inferior epigastric artery perforators for forearm reconstruction: A case report. World J Clin Cases 2024; 12(4): 828-834
- URL: https://www.wjgnet.com/2307-8960/full/v12/i4/828.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i4.828
Soft-tissue defects in the upper extremities may be challenging for reconstructive surgeons. In particular, when these defects are severe and involve functional structures, such as vessels, tendons, nerves, bones, and joints, immediate reconstruction is essential to minimize the risk of infection, reduce patient morbidity, and restore function in the affected limb[1,2].
Various reconstructive techniques, such as local, regional, distant, and free flaps, have been developed to address soft tissue defects in the hand and upper extremities. Before the introduction of free flaps, pedicle flaps from the abdomen and groin were considered the standard approach for successful upper limb reconstruction[2]. However, these flaps have drawbacks, such as the need for flap division, patient discomfort, longer hospital stays, and stiffness of the extremities[3]. Moreover, there are some limitations, including flap size restrictions, potential partial loss of the flap, and donor-site morbidities. Since the introduction of microsurgery in the 1970s, free tissue transfers using microsurgical techniques have been widely used for the functional reconstruction of the upper extremities. These offer early and customized reconstructive solutions for upper-limb injuries. However, they may not always be accessible because of their high costs and technical requirements[4]. Furthermore, in cases involving extensive vascular injury, free tissue transfer may not be ideal in cases involving extensive vascular injury[5]. Hence, pedicled abdominal flaps can be considered a safe and effective alternative for upper-extremity reconstruction in such situations.
The deep inferior epigastric artery perforators (DIEP) flap, first described in 1989, has been the preferred free flap in reconstructive surgery, mainly for breast reconstruction, owing to minimal donor-site morbidity and abundant soft tissue supply[6]. However, this flap has rarely been used as a pedicle flap to cover defects of the upper extremities, with only a few reported studies[7]. In this report, we present our case of upper extremity reconstruction using a pedicled DIEP flap.
The study was approved by the Institutional Review Board of Dankook University hospital (IRB No.2023-08-004) and performed in accordance with the principles of the Declaration of Helsinki.
A 46-year-old man was referred to our tertiary referral hospital, a level I trauma center, complaining of a large soft tissue crush injury to the forearm caused by a pressing machine.
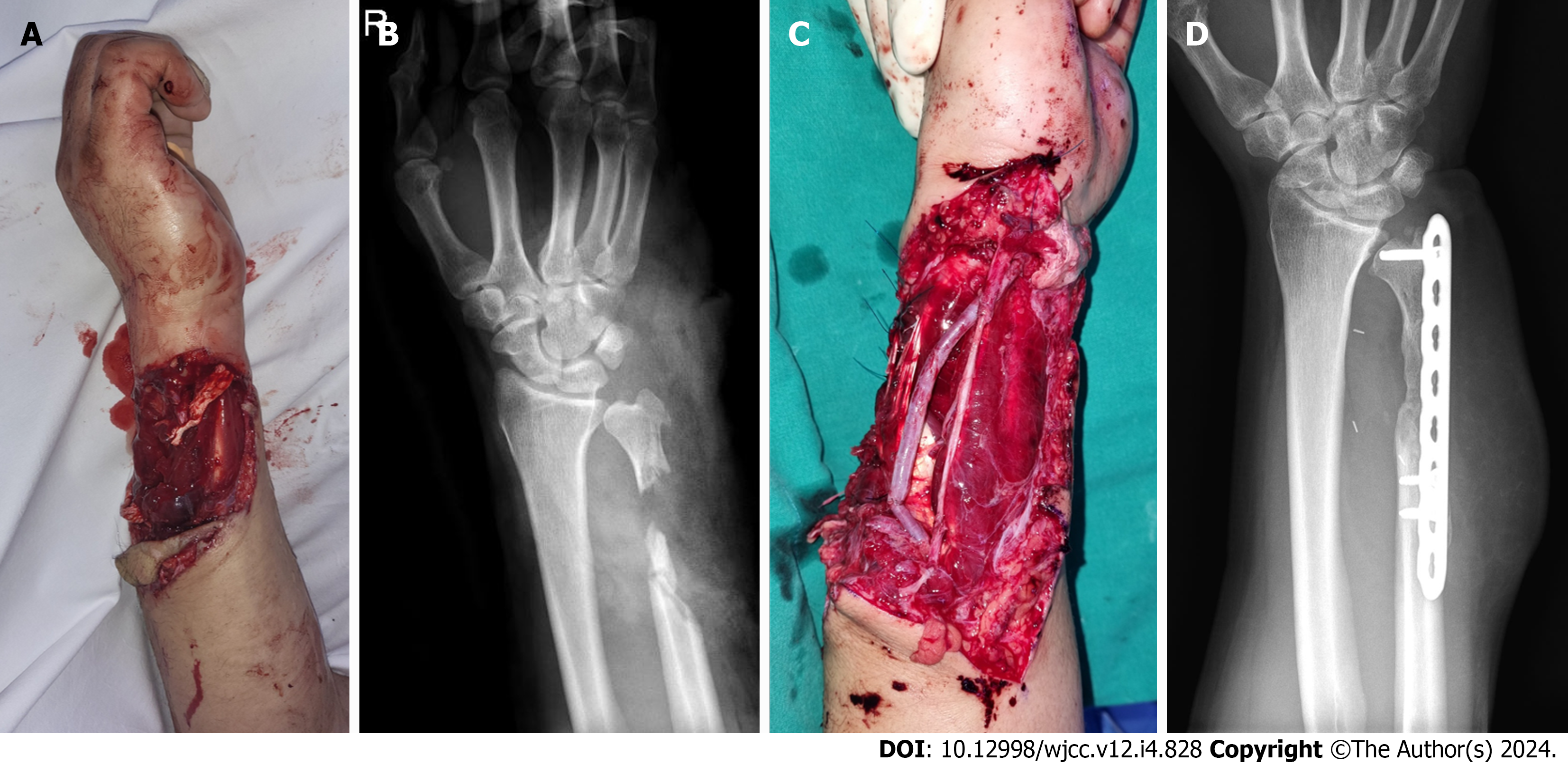
A 15 cm × 10 cm soft tissue defect with complete rupture of the ulnar side structures of the forearm was found, including multiple tendons [4th and 5th extensor digitorum communis (EDC), 4th and 5th flexor digitorum superficialis (FDS), extensor digiti minimi, extensor carpi ulnaris, and flexor carpi ulnaris], ulnar artery, vein, and nerve, and cephalic vein (Figure 1A).
No significant past medical history was reported.
No significant personal or family history was reported.
Distal motor functions of the median and radial nerves were preserved. However, ulnar nerve function tests such as Froment’s test and Egawa’s sign were positive. The sensory dermatomes of the median and radial nerves were 100%, but those of the ulnar nerve dermatome could not be checked. Pulse was detected in the radial artery but not in the ulnar artery. The capillary refill time was delayed by 3 seconds.
The patient’s preoperative laboratory tests were within normal ranges.
Plain radiography revealed a distal ulnar fracture (Figure 1B).
The patient was diagnosed with a soft tissue defect in the right forearm with the destruction of multiple functional structures.
Large segmental ulnar artery and ulnar nerve defects were primarily reconstructed by an orthopedic surgeon using the autologous saphenous vein and sural nerve, respectively. The 4th and 5th FDS and 4th EDC could be directly repaired. However, the proximal ends of the remaining tendons were augmented to the adjacent tendons. Additionally, the Masquelet technique was adopted because of the extensive soft tissue damage and bone defects[8]. The first stage of the Masquelet technique included complete debridement, stabilization of the fracture site, placement of bone cement, and closure of the fracture site using the adjacent muscles (Figure 1C and D). The second stage lasted for a few weeks.
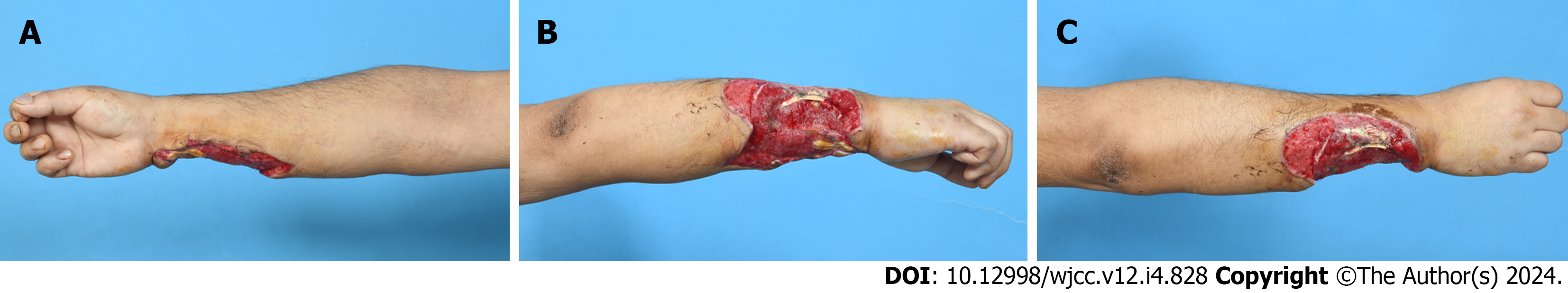
One week after the initial orthopedic management of the neurovascular injury and fractures, the patient was referred to the plastic and reconstructive surgery department for wound management and coverage (Figure 2). Surgical debridement and negative-pressure wound therapy were performed to prepare the wound bed. Final debridement revealed a 20 cm × 15 cm soft tissue defect with flexor and extensor tendons exposure. Computed tomography (CT) angiography was performed to evaluate the condition of the reconstructed ulnar artery for reconstruction using free flap. It showed limited visibility of blood flow in reconstructed ulnar artery. Therefore, a pedicled DIEP flap was planned for forearm reconstruction in the patient with large soft tissue defect 10 days after the initial surgery.
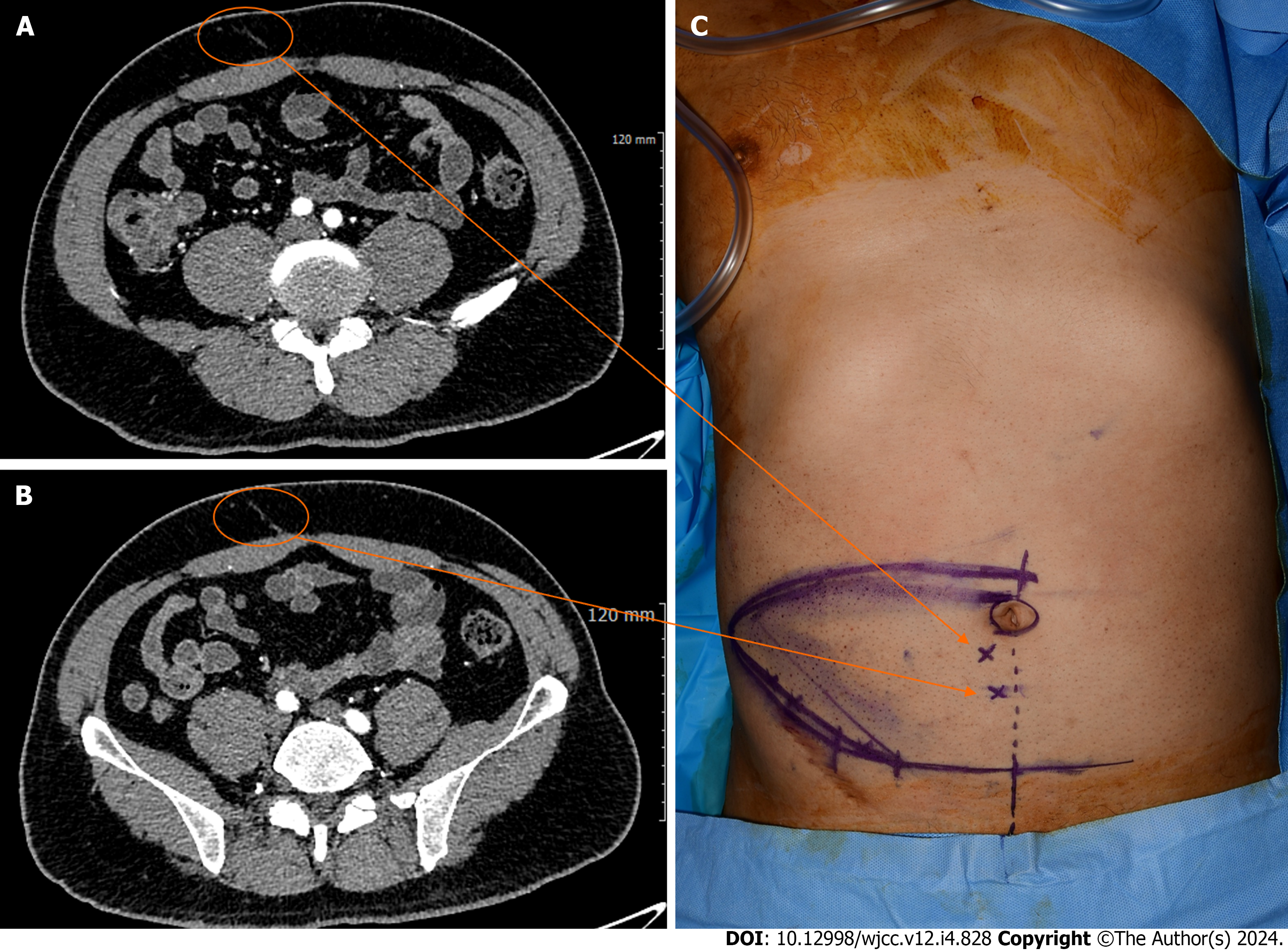
Preoperative CT findings using a slice thickness of 1 mm showed appropriate localization of the most favorable perforators (Figure 3A and B). Intraoperatively, perforators from the deep inferior epigastric artery (DIEA) were detected in the paraumbilical area using a handheld Doppler probe, and their positions were marked on the skin (Figure 3C). Under general anesthesia, an incision was made along the subcutaneous tissues to the deep fascia. The flap was then elevated from the lateral to the medial side of the deep fascial surface. Two large perforators of sufficient caliber were preserved, whereas the smaller perforators were cauterized. Dissection was continued until an appropriate length of the pedicle was obtained.
We performed the defatting procedure on sub-Scarpa fat layer to reduce the thickness of the DIEP flap. The flap was inserted into the donor and sutured. After soft tissue coverage surgery, the upper limb was strapped to the abdominal wall using a splint and elastic bandage, exposing part of the flap for inspection. Daily moisture dressings using Bactigras® gauze, Vaseline gauze, and mupirocin ointment were used to cover the raw surface of the flap and the suture margin. Flap division was performed 3 wk later under general anesthesia. New sutures were placed at the site of the divided flap, and the remnant abdominal defect was closed directly.
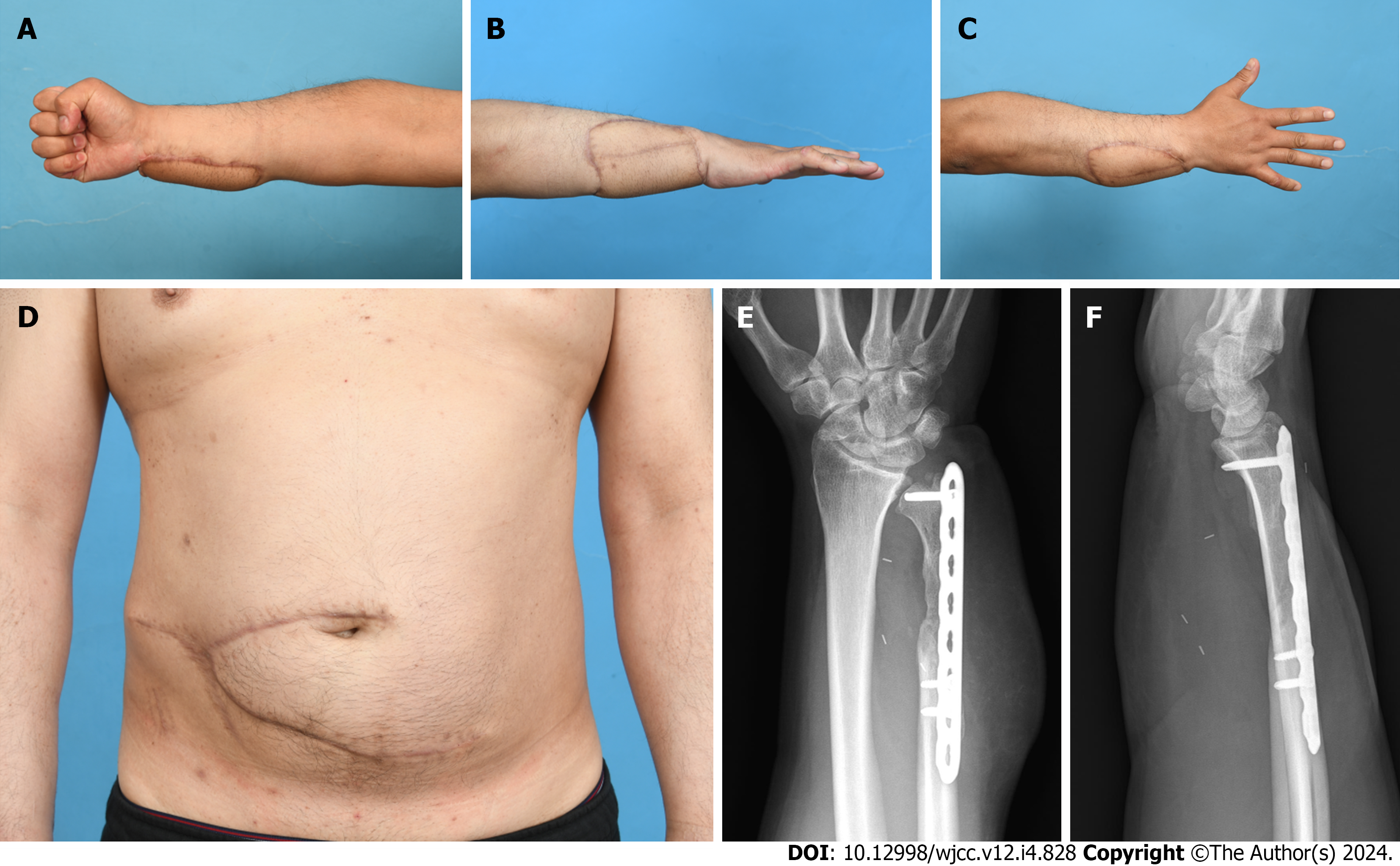
The flap survived and healed completely, with no morbidity at the donor site during the perioperative period. Ten weeks later, in the second stage of the Maquelet technique, the induction membrane was cut open, and autologous bone grafting after removal of the bone cement was performed in the orthopedic department. Six months later, the right forearm and abdominal donor site flaps healed well, had good contours and the bone union was achieved (Figure 4). No stiffness was observed in the shoulders or elbows. Furthermore, flexion and extension of the 4th and 5th fingers were possible. However, the ulnar nerve palsy symptoms persisted.
Pedicled groin flaps have limited usability due to their small size, which makes them inadequate for covering large defects. Furthermore, vascularity of the groin flap beyond the anterior superior iliac spine cannot be ensured. Hence, it cannot reconstruct large soft-tissue defects in the proximal forearm, elbow, and upper arm. Pedicled abdominal flaps are larger than groin flaps. However, they are random-pattern skin flaps that rely on unnamed vessels, which may cause partial flap necrosis[1]. The combination of CT angiography and handheld Doppler can help detect the presence of a large-caliber DIEP, allowing surgeons to find perforator vessels during surgery, potentially reducing the risk of partial flap necrosis.
The DIEA originates from the external iliac artery. As it approaches the arcuate line, it is divided into medial and lateral branches. The DIEA ascends from the lateral side of the rectus abdominis muscle towards the umbilicus. It runs between the transverse fascia and peritoneum before penetrating the posterior side of the rectus abdominis muscle. After penetrating the muscle, it exhibits various branching patterns, typically having an average of five perforators (with a range of ± 2) that supply blood to the skin. These perforating vessels were primarily concentrated within 2 cm above and 6 cm below the umbilicus, extending approximately 1–6 cm around the lateral aspect of the umbilicus. Recently, CT angiography has been used to assess the blood supply and map perforators of the lower abdominal wall. Using a slice thickness of 1 mm, CT scans provide precise localization of the most favorable perforators, which reduces surgical time and assists with intraoperative decision-making.
In this case, the patient was not the most suitable candidate for a free microvascular flap. Due to restricted blood flow in the reconstructed ulnar artery, an end-to-side anastomosis on the remaining radial artery became necessary for the free flap, which poses a technical challenge. We also did not consider the free flap using proximal vascular loop because saphenous vein interposition graft has already been performed and there is a risk of thrombosis in free flap using proximal vascular loop. Therefore, we designed a pedicled abdominal flap using the DIEP to achieve extensive and durable coverage of the reconstructed structures. The advantage of this option is that it eliminates the need for anast
This flap type has several advantages. First, because of the identification of DIEP, this flap allows for using a greater amount of soft tissue and reduces partial flap necrosis due to a robust blood supply. Second, compared to microsurgery, the procedure is relatively straightforward. Although the flap elevation process was the same as that of the free DIEP flap, microvascular anastomosis was not required. Consequently, the operative time was reduced and complications associated with microsurgery were eliminated. Regarding donor-site morbidity, a pedicled DIEP flap can improve the appearance of the abdominal wall with minimal damage to its function. Previous abdominal flap techniques resulted in large donor-site wounds that necessitated further coverage, such as skin grafts. However, this approach is not ideal because of contour irregularities and the need for additional surgeries. In our method, the donor site was aesthetically closed during pedicle division, eliminating the need for a skin graft.
However, the thickness of DIEP flap may be a disadvantage, particularly in obese patients. This may require additional procedure like defatting or fat resection for refinement. If smaller flaps are required for reconstruction, the DIEP flap might not be the most suitable option. Another disadvantage of pedicled DIEP flap is being a 2-stage procedure, leading to a long period of immobilization. This process poses a potential risk of the shoulder or elbow joint stiffness, particularly in old patients. In addition, the flap manipulation is technically demanding[9]. It requires the surgeon to have prior experience with a free DIEP operation; therefore, in the event of pedicle injury, the flap can be salvaged using a microsurgical approach without delay. However, these disadvantages are outweighed by the advantages of the pedicled DIEP flap in soft-tissue reconstruction of the upper extremities.
In conclusion, the pedicled DIEP flap is a reliable and suitable option for managing complex upper extremity injuries and providing adequate soft tissue coverage with minimal donor-site morbidity.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: South Korea
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Malagón-López P, Spain S-Editor: Gao CC L-Editor: A P-Editor: Cai YX
| 1. | Anil R, Prabhu A, Kumar N. Abdominal Flaps in the Management of Upper Limb Defect- Our Experience. J Evol Med Dent Sci. 2017;6:4711-4716. [DOI] [Full Text] |
| 2. | Herter F, Ninkovic M. Rational flap selection and timing for coverage of complex upper extremity trauma. J Plast Reconstr Aesthet Surg. 2007;60:760-768. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 39] [Cited by in RCA: 43] [Article Influence: 2.4] [Reference Citation Analysis (1)] |
| 3. | Al-Qattan MM, Al-Qattan AM. Defining the Indications of Pedicled Groin and Abdominal Flaps in Hand Reconstruction in the Current Microsurgery Era. J Hand Surg Am. 2016;41:917-927. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 48] [Article Influence: 5.3] [Reference Citation Analysis (0)] |
| 4. | Jabaiti S, Ahmad M, AlRyalat SA. Reconstruction of Upper Extremity Defects by Random Pedicle Abdominal Flaps: Is It Still a Valid Option? Plast Reconstr Surg Glob Open. 2020;8:e2687. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 1] [Cited by in RCA: 7] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 5. | Adidharma W, Tandon V, Grant D, Chung KC. Extended Abdominal Pedicled Flap Using a Modified Abdominoplasty Incision for Reconstruction of an Extensive Forearm Defect. J Hand Surg Glob Online. 2022;4:367-371. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in RCA: 3] [Reference Citation Analysis (1)] |
| 6. | Koshima I, Soeda S. Inferior epigastric artery skin flaps without rectus abdominis muscle. Br J Plast Surg. 1989;42:645-648. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 800] [Cited by in RCA: 811] [Article Influence: 22.5] [Reference Citation Analysis (0)] |
| 7. | Zeng A, Xu J, Yan X, You L, Yang H. Pedicled deep inferior epigastric perforator flap: an alternative method to repair groin and scrotal defects. Ann Plast Surg. 2006;57:285-288. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 35] [Cited by in RCA: 41] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 8. | Masquelet A, Kanakaris NK, Obert L, Stafford P, Giannoudis PV. Bone Repair Using the Masquelet Technique. J Bone Joint Surg Am. 2019;101:1024-1036. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 102] [Cited by in RCA: 168] [Article Influence: 28.0] [Reference Citation Analysis (0)] |
| 9. | Seyhan T, Borman H. Pedicled deep inferior epigastric perforator flap for lower abdominal defects and genital reconstructive surgery. J Reconstr Microsurg. 2008;24:405-412. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 15] [Cited by in RCA: 15] [Article Influence: 0.9] [Reference Citation Analysis (0)] |