Published online Feb 6, 2024. doi: 10.12998/wjcc.v12.i4.801
Peer-review started: October 7, 2023
First decision: November 21, 2023
Revised: December 2, 2023
Accepted: January 15, 2024
Article in press: January 15, 2024
Published online: February 6, 2024
Processing time: 110 Days and 1.6 Hours
Acute appendicitis is the most common abdominal emergency. At present, the main treatments for periappendiceal abscess include antibiotics and surgery. However, the complications and mortality of emergency surgery are high. The preferred therapy is conservative treatment with antibiotics first, ultrasound-guided puncture drainage or surgical treatment is followed when necessary. Endoscopic retrograde appendicitis therapy (ERAT) for acute uncomplicated appendicitis have been proved clinically effective, but it is rarely used in periappendiceal abscess.
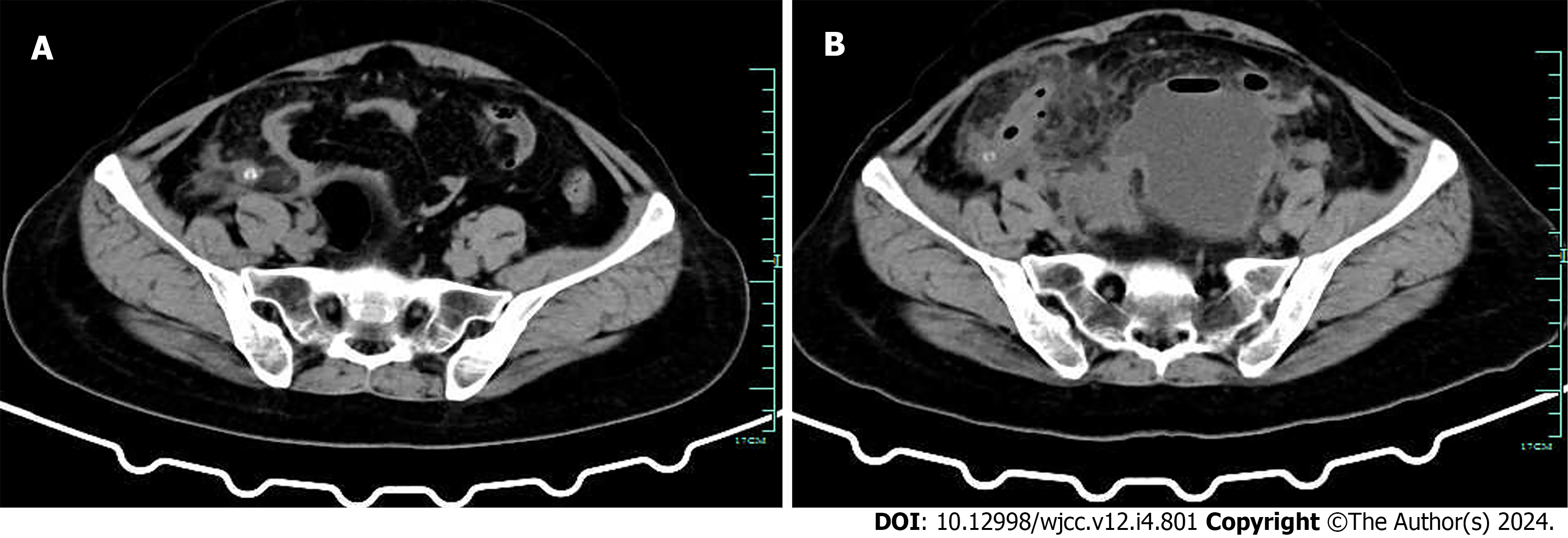
We report a patient admitted to hospital because of “right lower abdominal pain for six days”. The computerized tomography (CT) of patient showed that appendicitis with fecaliths and abscess in the pelvis. The patient was treated by CT-guided puncture and drainage of abdominal abscess combined with ERAT to remove appendiceal fecaliths, irrigation and stent placement.
The patient did not receive surgery because of impoverished family. Abdominal pain did not recur during the follow-up period. This case confirms the value of ERAT in the treatment of periappendiceal abscess.
Core Tip: We report a patient admitted to hospital because of “right lower abdominal pain for six days”. The computerized tomography of patient showed that appendicitis with fecaliths and abscess in the pelvis. This case is appendiceal abscess treated by puncture drainage combined with endoscopic retrograde appendicitis therapy (ERAT) to prevent the recurrence of acute appendicitis, suggesting the feasibility of combining these two methods to treat patients with appendiceal abscess, and providing option for elderly patients who refuse surgery or cannot receive surgery because of poor health. Recently, research has confirmed that ERAT group has shorter hospitalization time, faster pain relief and lower acute appendicitis recurrence rate compared with antibiotic treatment alone, and ERAT can take out appendiceal fecaliths, which is a common cause of appendicitis. Therefore, we believe that ERAT can benefit for these patients.
- Citation: Li QM, Ye B, Liu JW, Yang SW. Endoscopic retrograde appendicitis treatment for periappendiceal abscess: A case report. World J Clin Cases 2024; 12(4): 801-805
- URL: https://www.wjgnet.com/2307-8960/full/v12/i4/801.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i4.801
Achieving an accurate diagnosis of acute appendicitis is still difficult for some patients nowadays. Endoscopic retrograde appendicitis therapy (ERAT) might have some value in diagnosing patients with acute appendicitis, and the value of ERAT in the treatment of acute uncomplicated appendicitis has been confirmed[1-5]. However, there is little research on ERAT in the treatment of periappendiceal abscess.
A 48-year-old female complained of pain in the right lower abdomen, nausea and vomiting for 6 d.
The pain was constant, localized to right lower abdomen, no fever, and no diarrhea. Initially, the patient refused operation and was managed conservatively with antibiotic of levofloxacin.
The patient had a history of hyperthyroidism and was cured. The patient had no history of abdominal surgery, toxicity, or radiation exposure.
There was no family history of malignant tumors or other diseases.
Temperature was 38.4 °C, pulse was 131 beats/min, respiration was 20 times/min, blood pressure was 106/67 mmHg. No jaundice was observed. The abdomen was flat. Physical examination revealed tenderness with rebound tenderness in the lower abdomen. Murphy’s sign was negative. Bowel sounds 3 times/min, shifting dullness was negative.
Serum C-reactive protein, 116.18 mg/L (normal: 0-8 mg/L); white blood cell count, 11.2 × 109/L [(4-10) × 109/L]; percentage of neutrophils, 88% (40%-75%); hemoglobin, 122 g/L (115-150 g/L); platelet, 247 × 109/L [(100-300) × 109/L]; procalcitonin, 1.25 ng/mL (0-0.05 ng/mL); aspartate aminotransferase, 33 U/L (7-40 U/L); alanine aminotransferase, 37 U/L (13-35 U/L); total bilirubin, 9.6 μmol/L (< 23.0 μmol/L).
The computerized tomography (CT) scan of the whole abdomen showed “acute appendicitis with fecaliths” (Figure 1A). 6 d later, The CT scan of the whole abdomen showed that “acute appendicitis, appendiceal abscess, pelvic encapsulated effusion formation” (Figure 1B). The patient was admitted to hospital.
The final diagnosis was acute appendicitis with fecaliths, periappendiceal abscess, pelvic encapsulated effusion.
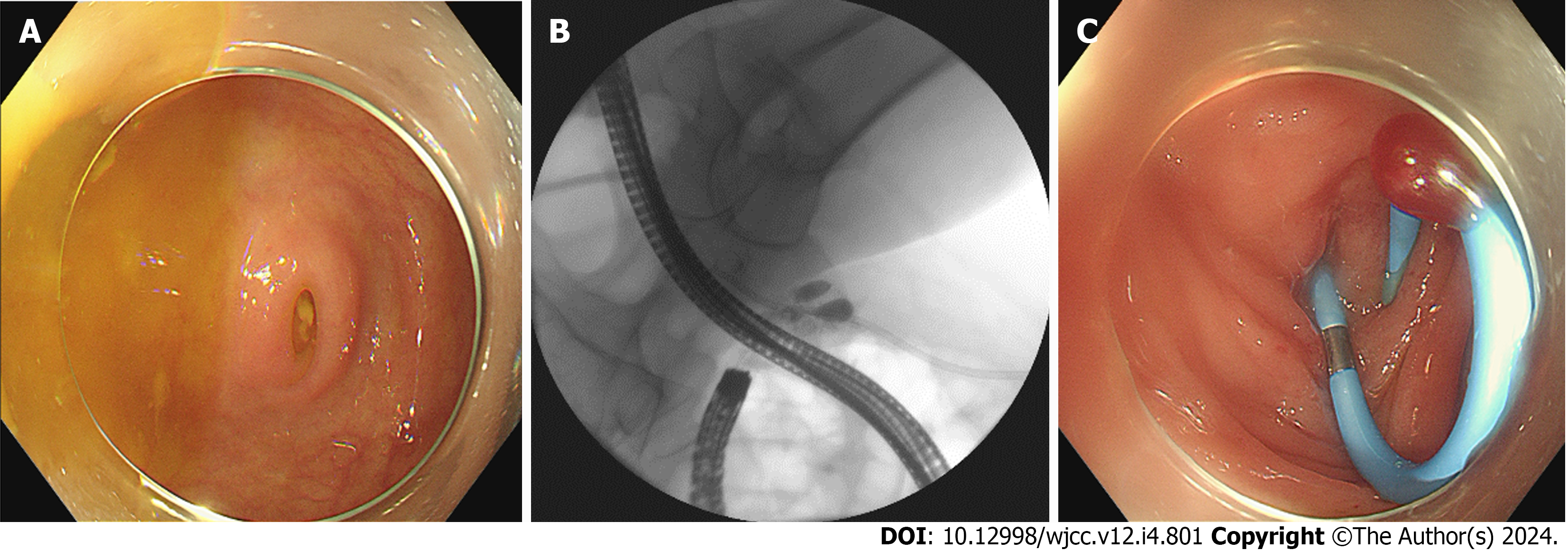
The antibiotic had been changed to imipenem and cilastatin sodium at admission. Surgical intervention was preferred to carry out 6-12 wk later[6,7]. As is known to surgeons, immediate appendectomy may be technically demanding because of the distorted anatomy and the difficulties to close the appendiceal stump because of the inflamed tissues. The complications and mortality of emergency surgical treatment are high. Even worse, it may result in an unnecessary ileocecal resection or right-sided hemicolectomy for technical reasons or suspicion of malignancy in about 3% of the patients[8]. So CT-guided periappendiceal abscess puncture and drainage was performed. After the treatment, the patient still had tenderness in the right lower abdomen, at the same time, she had incomplete intestinal obstruction and appendiceal fecaliths, so she was transferred to gastroenterology department for further treatment. ERAT was given immediately after the symptoms of intestinal obstruction relieved. In preparation for ERAT, the bowel was prepared according to the requirements of colonoscopy. 1 L polyethylene glycol (PEG) electrolyte solution was administered at 8:00 pm the day before ERAT, 2 L PEG electrolyte solution was administered to the patient 4 h before the procedures of ERAT. When the remaining PEG electrolyte solution was 300 mL, 15 mL of simethicone was added and taken together. ERAT was performed as described as follows: Colonoscope (CF-H260, Olympus, Japan) attached by a transparent cap was used. When the colonoscope entered the cecum, endoscopic findings in the patient showed mucosal hyperemia, obvious swollen of surrounding mucosa, and purulent discharge from the appendiceal orifice (Figure 2A). After finding Gerlach’s valve in the cecum, colonoscope was positioned close to the appendiceal orifice, the tip of a catheter (PR-104Q-1, Olympus, Japan) could be wedged into the appendiceal orifice, then a guide wire was inserted in to the appendiceal lumen. After that, iobitridol was used to fill the appendix (Figure 2B), the procedures to relieve the appendiceal lumen obstruction including appendiceal luminal irrigation with 50 mL ornidazole sodium chloride solution, fecaliths extraction with stone basket, finally, a stent (7F; Boston Scientific) was placed into the lumen over the guide wire for luminal decompression (Figure 2C). The patient abdominal pain was relieved immediately, and took fluid one hour after operation. After four days of antibiotic treatment, the abdominal puncture drainage tube was removed.
The patient was reexamined one month later, and the stent at appendiceal lumen fell off by itself. The patient refused surgery because of poverty, so no appendectomy was performed afterwards. The patient was followed up for more than one year, there was no recurrence of abdominal pain.
Appendicitis is one of the most common surgical emergencies. Periappendiceal abscess is often caused by misdiagnosis or a delay in treatment. It is well-known that differentiation among the nonperforated and perforated appendicitis is important. Phlegmon or abscess after appendiceal perforation may be managed by conservative treatment or percutaneous drainage to decrease the patient’s morbidity and surgical intervention may be carried out 6-12 wk later.
Reviewing the diagnosis and treatment process of this patient, the appendix abscess was related to the improper selection of antibiotic in the early stage, and appendiceal fecaliths were also a factor in the progression of the disease. The literatures have made it clear that appendicitis with fecaliths is mostly obstructive, with severe clinical symptoms and rapid development, which is easy to form abscess or perforation[9-12]. In the past few years, there were some articles reported cases of periappendiceal abscess treated by ERAT[13,14]. ERAT includes appendicography to provide visualization of appendiceal lumen and identification lumen stenosis or dilation or fecaliths blocking lumen, and can confirm the patency of the appendiceal lumen with a plastic stent to drain pus.
This case gives us a warning: We should pay more attention to the patient with appendicitis with fecaliths, there disease progress faster and are more likely to need surgery. For patients with abscess, CT-guided or ultrasound-guided puncture and drainage showed good effect in the treatment of abscess. In this case, the pain was obviously relieved after abscess drainage, and the abscess shrank obviously, but the patient still had tenderness in the right lower abdomen. Considering that the patient had appendiceal fecaliths, and the patient was not willing to have appendicectomy in a few weeks. In addition, ERAT for uncomplicated acute appendicitis with fecaliths was effective in all cases we had done, and without complication. We believed that ERAT can take out the fecaliths and relieve the pain of the patient. We recommended the patient ERAT can be another good choice, she choose ERAT.
This case is appendiceal abscess treated by puncture drainage combined with ERAT to prevent the recurrence of acute appendicitis, suggesting the feasibility of combining these two methods to treat patients with appendiceal abscess, and providing option for elderly patients who refuse surgery or cannot receive surgery because of poor health. Recently, research has confirmed that ERAT group has shorter hospitalization time, faster pain relief and lower acute appendicitis recurrence rate compared with antibiotic treatment alone, and ERAT can take out appendiceal fecaliths, which is a common cause of appendicitis[15]. Therefore, we believe that ERAT can benefit for these patients.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Medicine, research and experimental
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): 0
Grade C (Good): C
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Khokha V, Belarus S-Editor: Wang JJ L-Editor: A P-Editor: Cai YX
| 1. | Liu CH, Tsai FC, Hsu SJ, Yang PM. Successful colonoscopic drainage of appendiceal pus in acute appendicitis. Gastrointest Endosc. 2006;64:1011; discussion 1012. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 7] [Cited by in RCA: 5] [Article Influence: 0.3] [Reference Citation Analysis (0)] |
| 2. | Liu BR, Song JT, Han FY, Li H, Yin JB. Endoscopic retrograde appendicitis therapy: a pilot minimally invasive technique (with videos). Gastrointest Endosc. 2012;76:862-866. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 29] [Cited by in RCA: 54] [Article Influence: 4.2] [Reference Citation Analysis (0)] |
| 3. | Liu BR, Ma X, Feng J, Yang Z, Qu B, Feng ZT, Ma SR, Yin JB, Sun R, Guo LL, Liu WG. Endoscopic retrograde appendicitis therapy (ERAT): a multicenter retrospective study in China. Surg Endosc. 2015;29:905-909. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 28] [Cited by in RCA: 51] [Article Influence: 4.6] [Reference Citation Analysis (0)] |
| 4. | Li Y, Mi C, Li W, She J. Diagnosis of Acute Appendicitis by Endoscopic Retrograde Appendicitis Therapy (ERAT): Combination of Colonoscopy and Endoscopic Retrograde Appendicography. Dig Dis Sci. 2016;61:3285-3291. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 17] [Cited by in RCA: 25] [Article Influence: 2.8] [Reference Citation Analysis (0)] |
| 5. | Jarrett RF, Mitsuya H, Mann DL, Cossman J, Broder S, Reitz MS. Configuration and expression of the T cell receptor beta chain gene in human T-lymphotrophic virus I-infected cells. J Exp Med. 1986;163:383-399. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 16] [Cited by in RCA: 17] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 6. | Friedell ML, Perez-Izquierdo M. Is there a role for interval appendectomy in the management of acute appendicitis? Am Surg. 2000;66:1158-1162. [PubMed] |
| 7. | Yamini D, Vargas H, Bongard F, Klein S, Stamos MJ. Perforated appendicitis: is it truly a surgical urgency? Am Surg. 1998;64:970-975. [PubMed] |
| 8. | Andersson RE, Petzold MG. Nonsurgical treatment of appendiceal abscess or phlegmon: a systematic review and meta-analysis. Ann Surg. 2007;246:741-748. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 269] [Cited by in RCA: 267] [Article Influence: 14.8] [Reference Citation Analysis (1)] |
| 9. | Horrow MM, White DS, Horrow JC. Differentiation of perforated from nonperforated appendicitis at CT. Radiology. 2003;227:46-51. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 116] [Cited by in RCA: 99] [Article Influence: 4.5] [Reference Citation Analysis (0)] |
| 10. | Foley TA, Earnest F 4th, Nathan MA, Hough DM, Schiller HJ, Hoskin TL. Differentiation of nonperforated from perforated appendicitis: accuracy of CT diagnosis and relationship of CT findings to length of hospital stay. Radiology. 2005;235:89-96. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 61] [Cited by in RCA: 63] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 11. | Lin CJ, Chen JD, Tiu CM, Chou YH, Chiang JH, Lee CH, Chang CY, Yu C. Can ruptured appendicitis be detected preoperatively in the ED? Am J Emerg Med. 2005;23:60-66. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 25] [Cited by in RCA: 28] [Article Influence: 1.4] [Reference Citation Analysis (0)] |
| 12. | Williams RF, Blakely ML, Fischer PE, Streck CJ, Dassinger MS, Gupta H, Renaud EJ, Eubanks JW, Huang EY, Hixson SD, Langham MR. Diagnosing ruptured appendicitis preoperatively in pediatric patients. J Am Coll Surg. 2009;208:819-25; discussion 826. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 57] [Cited by in RCA: 52] [Article Influence: 3.3] [Reference Citation Analysis (0)] |
| 13. | Wu R, Fu M, Fan WT, Tao YW, Fan ZN. The endoscopic retrograde appendicitis therapy in the treatment of appendiceal abscess: a preliminary exploration. Eur J Gastroenterol Hepatol. 2022;34:1195. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1] [Reference Citation Analysis (0)] |
| 14. | Song M, Ullah S, Liu B. Endoscopic Retrograde Appendicitis Therapy for Treating Periappendiceal Abscess: First Human Case Report. Am J Gastroenterol. 2021;116:1119. [RCA] [PubMed] [DOI] [Full Text] [Cited by in RCA: 7] [Reference Citation Analysis (0)] |
| 15. | Li D, Yang B, Liao J, Li Y, Liu D, Zhao L, Meng X, Hu H, Kong L, Podda M, Ullah S, Liu B. Endoscopic retrograde appendicitis therapy or antibiotics for uncomplicated appendicitis. Br J Surg. 2023;110:635-637. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 6] [Cited by in RCA: 17] [Article Influence: 8.5] [Reference Citation Analysis (0)] |