Published online Feb 6, 2024. doi: 10.12998/wjcc.v12.i4.782
Peer-review started: September 13, 2023
First decision: December 5, 2023
Revised: December 14, 2023
Accepted: January 8, 2024
Article in press: January 8, 2024
Published online: February 6, 2024
Processing time: 133 Days and 21.7 Hours
Venovenous extracorporeal membrane oxygenation (V-V ECMO) has become an important treatment for severe pneumonia, but there are various complications during the treatment. This article describes a case with severe pneumonia success
A 64-year-old man had severe pulmonary infection and respiratory failure. He was admitted to our hospital and was given ventilation support (fraction of inspired oxygen 100%). The respiratory failure was not improved and he was treated by V-V ECMO, during which the venous return catheter, which was supposed to be in the right internal vein, entered the superior vena cava directly in the mediastinum. There was a risk of massive mediastinal bleeding if the catheter was removed directly when the ECMO was withdrawn. Finally, the patient underwent vena cava angiography + balloon attachment + ECMO with
Patients may have different vascular conditions. Multidisciplinary cooperation can ensure patient safety. Our experience will provide a reference for similar cases.
Core Tip: Our paper provides a rare complication in the course of extracorporeal membrane oxygenation treatment, and our experience with this case can provide a great reference for colleagues who encounter the same situation.
- Citation: Song XQ, Jiang YL, Zou XB, Chen SC, Qu AJ, Guo LL. Accidental placement of venous return catheter in the superior vena cava during venovenous extracorporeal membrane oxygenation for severe pneumonia: A case report. World J Clin Cases 2024; 12(4): 782-786
- URL: https://www.wjgnet.com/2307-8960/full/v12/i4/782.htm
- DOI: https://dx.doi.org/10.12998/wjcc.v12.i4.782
Venovenous extracorporeal membrane oxygenation (V-V ECMO) has become a routine operation for the treatment of severe pneumonia that cannot be relieved by mechanical ventilation[1], but various complications during ECMO have been reported, including hemorrhage and incorrect catheter placement[2-4]. A patient with severe pneumonia compli
A 64-year-old man visited our hospital with cough and wheezing for 6 d, and fever for 1 d.
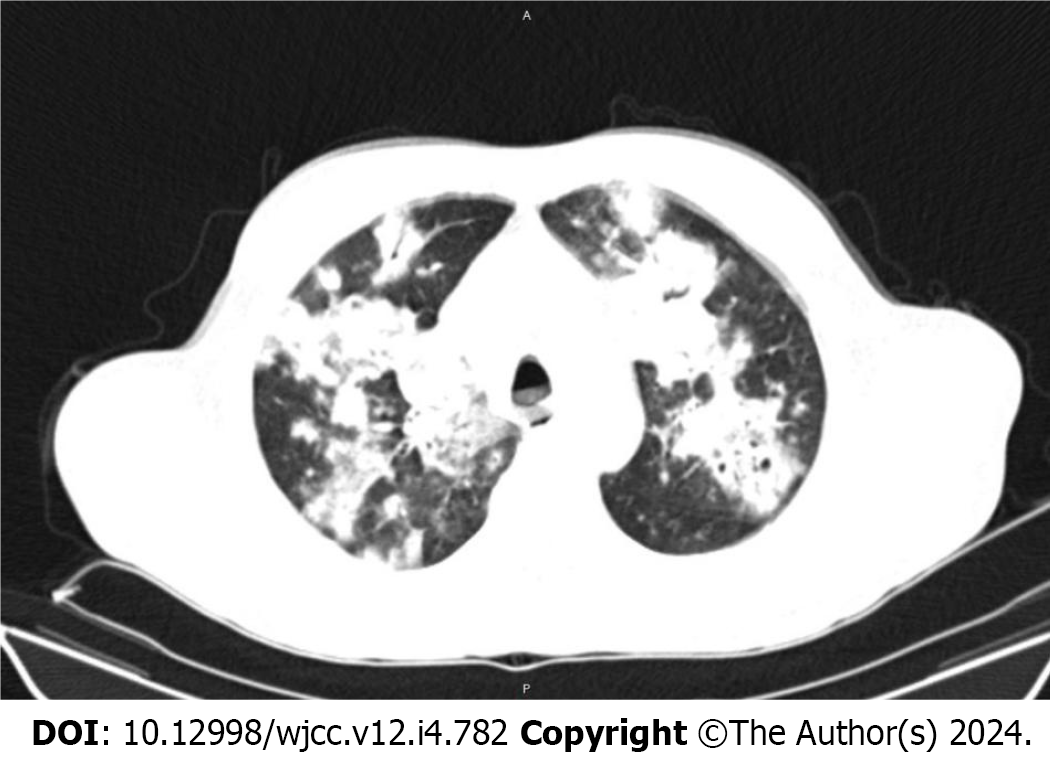
The man caught a cold on holiday. Symptoms were sneezing and coughing white sputum, but there was no chest pain or hemoptysis, and the patient was normothermic. The cough became worse and he began to wheeze and could not lie down at night, occasionally with blood in the sputum, with a fever of 38.5 °C. Oral medication had no effect. When he arrived at our hospital, his arterial oxygen saturation (SaO2) was < 90% under mask oxygen inhalation, and chest computed tomography (CT) showed severe pulmonary infection (Figure 1). The patient was admitted to our respiratory intensive care unit (RICU) with mechanical ventilation on August 19, 2022.
No smoking history or other chronic disease history.
The patient had no previous or family history of similar illnesses.
The patient weighed 70 kg, and his height was 170 cm. His vital signs were: Body temperature, 37 °C; blood pressure, 153/101 mmHg; heart rate, 162 beats/min; respiratory rate, 36 breaths/min (ventilator); SaO2, 92% [fraction of inspired oxygen (FiO2) 100%]. He was in a sedative state, and both lungs had audible dry and wet rales. No other positive signs were found during physical examination.
Laboratory tests at the time of admission to the RICU were as follows: White blood cell count, 7.63 × 109/L (reference range, 4 × 109-10 × 109/L); neutrophil percentage, 89.9% (reference range, 50.0%-70.0%); procalcitonin, 12.62 ng/mL (reference range, < 0.05 ng/mL); C-reactive protein, > 200 mg/L (reference range, 0-5 ng/mL); arterial blood gas pH, 7.21; arterial CO2 pressure, 65 mmHg; arterial oxygen pressure, 80 mmHg; K+, 3.3 mmol/L; glucose concentration, 15.4 mmol/L; and lactate, 3.1 mmol/L. No other abnormal results were found in routine blood biochemical analyses. The bronchoalveolar lavage fluid was collected on the day of admission and tested positive for influenza A.
Chest CT showed multiple inflammatory manifestations in both lungs (Figure 1).
The patient was diagnosed with severe pneumonia, respiratory failure, type A influenza, and electrolyte disturbance.
The patient was admitted to the RICU in our hospital on August 19, 2022 due to cough and expiratory dyspnea for 6 d, complicated with a fever of 38.5 °C for 1 d. Chest CT showed severe pneumonia in both lungs (Figure 1). After admission, the patient was given tracheal intubation and ventilator-assisted respiration, and because the pathogen was unknown, the anti-infective drugs were imipenem-cilastatin sodium, vancomycin, voriconazole, and oseltamivir. He was transferred to our Emergency ICU for V-V ECMO because of continuous hypoxia on the day of admission.
A right femoral vein blood drainage catheter and a right internal jugular vein blood return catheter was placed under ultrasound guidance. After catheterization, no catheter was found in the right internal jugular vein on routine ultrasound. The metallic catheter, which should have entered the right internal carotid artery, entered the superior vena cava directly in the mediastinum, which was confirmed by CT (Figure 2). Because the patient’s condition was serious, we decided to let ECMO run its course, with a rotational speed of approximately 3900 r/min, blood flow of approximately 5 L/min, FiO2 of 100%, and blood oxygen saturation increased to 100%. Follow-up treatments were adjusted according to the test results and the patient’s condition during the entire ECMO process was normal.
On September 1, 2022, the patient reached the standard for ECMO withdrawal. Chest CT was performed again and image reconstruction was performed before withdrawal, which showed that the catheter used for blood retrieval was only 2 cm in the superior vena cava (Figure 3). The following questions were encountered: (1) Could the internal jugular vein catheter be removed directly and compressed to stop bleeding? (2) What would happen if there were more bleeding after the catheter was removed? Did we need to stop bleeding by thoracotomy? and (3) Was it necessary to directly open the chest and remove the catheter? In order to ensure the safe withdrawal, our EICU organized multidisciplinary consultations including experts from thoracic surgery, cardiac surgery, vascular surgery, interventional surgery, and CT departments. Finally, two opinions were proposed: (1) Referral of the patient to a superior hospital; and (2) performing vena cava angiography + balloon attachment + ECMO extraction in our operating room (prepared for stent implantation, and conversion to thoracotomy for vascular exploration and repair at any time during surgery). We informed the family members of the consultative opinions, and the second opinion was adopted.
On September 3, 2022, the patient was transferred to the operating room for ECMO withdrawal surgery. The operation process was as follows. The 21F ECMO catheter was cut at the right inguinal region, one super-hard guide wire was inserted to replace the ECMO catheter and reached the superior vena cava, which led a pig tail catheter to the same position. Angiography performed through the pigtail catheter revealed that the ECMO catheter was located in the superior vena cava, and a 24 mm × 40 mm balloon was placed at the position of the ECMO catheter in the superior vena cava, along the guide wire placed previously. Then, another guide wire and pigtail catheter were placed in reserve. We cut off the neck of the ECMO catheter, inserted a hard wire, and replaced the neck ECMO catheter with a 14F Gore sheath. The balloon was filled with a pressure pump, and the 14F sheath in the superior vena cava was removed, but the neck guide wire was retained. Radiography through the second pigtail catheter showed that the balloon was blocked without obvious blood leakage. After the balloon was attached for 30 min, no extravasation of the contrast agent was found by multi-angle radiography. All equipment was removed and the procedure ended. The patient returned to the ward after the operation. The changes in red blood cells and hemoglobin were monitored for 1 wk after the operation. No blood transfusion was required, and there was no obvious bleeding (Table 1).
| Day 1 | Day 2 | Day 3 | Day 4 | Day 5 | Day 6 | Day 7 | |
| RBCs, × 1012/L | 3.53 | 3.83 | 3.53 | 3.50 | 3.18 | 3.05 | 3.33 |
| Hb (g/L) | 105 | 112 | 102 | 101 | 92 | 90 | 98 |
In the later stage, the patient was successfully weaned from the ventilator after continuous anti-infective treatment, nutritional support, rehabilitation, and other symptomatic treatments. He was discharged from the hospital on September 25, 2022 and returned to the local hospital for consolidation treatment for 1 wk. After 1 mo of follow-up, the patient recovered well without sequelae.
After technical improvement, V-V ECMO has played an increasingly important role in the treatment of severe pneumonia, especially since the COVID-19 pandemic[5]. There has been an increase in reports of various complications during the procedure, including catheter implantation, bleeding, and infection. The present case represents a situation that has not been reported before, and the patient was discharged safely after multidisciplinary collaboration. The following two factors were considered to be related to our mistake: (1) Ultrasound positioning was not applied throughout the process, and errors occurred during puncture; and (2) the patient had a vascular malformation. There were small branch vessels between the internal jugular vein and the superior vena cava. The guide wire entered the branch vessels by mistake and directly entered the superior vena cava.
Differences in the vascular anatomy mean that there may be mistakes during V-V ECMO, but multidisciplinary collaboration can help keep patients safe by giving advice from different perspectives. Our experience with this case will provide a reference for similar situations in the future.
Provenance and peer review: Unsolicited article; Externally peer reviewed.
Peer-review model: Single blind
Specialty type: Emergency medicine
Country/Territory of origin: China
Peer-review report’s scientific quality classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
P-Reviewer: Chiu H, Taiwan S-Editor: Chen YL L-Editor: Wang TQ P-Editor: Zhao S
| 1. | Ferguson ND, Fan E, Camporota L, Antonelli M, Anzueto A, Beale R, Brochard L, Brower R, Esteban A, Gattinoni L, Rhodes A, Slutsky AS, Vincent JL, Rubenfeld GD, Thompson BT, Ranieri VM. The Berlin definition of ARDS: an expanded rationale, justification, and supplementary material. Intensive Care Med. 2012;38:1573-1582. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 1051] [Cited by in RCA: 963] [Article Influence: 74.1] [Reference Citation Analysis (0)] |
| 2. | Banfi C, Pozzi M, Siegenthaler N, Brunner ME, Tassaux D, Obadia JF, Bendjelid K, Giraud R. Veno-venous extracorporeal membrane oxygenation: cannulation techniques. J Thorac Dis. 2016;8:3762-3773. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 30] [Cited by in RCA: 63] [Article Influence: 7.0] [Reference Citation Analysis (0)] |
| 3. | Rupprecht L, Lunz D, Philipp A, Lubnow M, Schmid C. Pitfalls in percutaneous ECMO cannulation. Heart Lung Vessel. 2015;7:320-326. [PubMed] |
| 4. | Hadaya J, Benharash P. Extracorporeal Membrane Oxygenation. JAMA. 2020;323:2536. [RCA] [PubMed] [DOI] [Full Text] [Cited by in Crossref: 8] [Cited by in RCA: 25] [Article Influence: 5.0] [Reference Citation Analysis (0)] |
| 5. | Badulak J, Antonini MV, Stead CM, Shekerdemian L, Raman L, Paden ML, Agerstrand C, Bartlett RH, Barrett N, Combes A, Lorusso R, Mueller T, Ogino MT, Peek G, Pellegrino V, Rabie AA, Salazar L, Schmidt M, Shekar K, MacLaren G, Brodie D; ELSO COVID-19 Working Group Members. Extracorporeal Membrane Oxygenation for COVID-19: Updated 2021 Guidelines from the Extracorporeal Life Support Organization. ASAIO J. 2021;67:485-495. [RCA] [PubMed] [DOI] [Full Text] [Full Text (PDF)] [Cited by in Crossref: 240] [Cited by in RCA: 272] [Article Influence: 68.0] [Reference Citation Analysis (0)] |